Acinetobacter baumannii: The Emergence of a Dangerous Multidrug-Resistant Pathogen
By: Kerri-Lynn Conrad

Introduction

A. baumannii (Figure 1) is a pathogenic species of bacteria whose spread has recently gained worldwide attention, most notably after outbreaks in United States military hospitals in Iraq and Afghanistan. The alarming rate by which A. baumannii has attained resistance to most classes of known antibiotics poses a great threat to our containment of the infection. A. baumannii can rapidly modify transmembrane proteins and efflux pumps to prevent current antibiotics from penetrating its inner membrane and executing their mechanism of action. Furthermore, the enhanced ability of A. baumannii (Figure 2) to obtain DNA from the external environment has allowed the species to obtain novel drug and heavy metal ion resistance genes. With resistance documented to all known classes of antibiotics, as well as cellular mechanisms that prevent dessication and the action of antimicrobials, the world is in great need of innovative pharmaceuticals and antimicrobials that can eliminate this dangerous pathogen.
Genome Structure
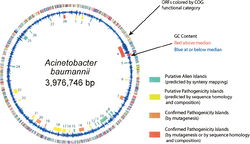
The genome of Acinetobacter baumannii (Figure 3) is a singular circular chromosome, accompanied by two plasmids, though this number can vary depending on the strain (3). The genome contains 3,976,746 base pairs and is composed of 3830 open reading frames. Approximately 17.2% of the open-reading frames are located within putative alien islands, highlighting Acinetobacter baumannii’s remarkable ability to incorporate foreign DNA into its genome (1).
Acinetobacter baumannii has several genes that permit it to pick up foreign DNA from its environment, as well as other microbes. These genes include PilQ, ComE, and PilF, commonly found in gram-negative bacteria, as well as closely related species Acinetobacter baylyi. Interestingly, the genome of Acinetobacter baumannii lacks a gene for ComP, a gene for a membrane transporter important for foreign DNA uptake in many species. Nonetheless, the ComEA gene of A. baumannii codes for a transmembrane protein that can bind foreign DNA in the environment and transport it to the internal environment of the cell where it can be incorporated into the genome. One study has suggested that the ComEA gene or possibly even the type IV pilus of A. baumannii allow it to effectively obtain foreign DNA from the environment, thus eliminating the need for the ComP gene found in many other species (1).
Closely tied to A. baumanniii’s ability to obtain foreign DNA for incorporation into its own genome are the putative alien islands (pAs) that permit the pathogenicity of A. baumanniii, distinguishing it from other Acinetobacter species. pAs obtained from the environment or from other species can possess a variety of functions. Nevertheless, many of the pAs that remain preserved in the A. baumannii genome are responsible for pathogenic and virulence factors, and are deemed PAIs. Of the approximately 28 pAs in the A. baumannii genome, 12 share significant sequence identity with virulence genes in other species of bacteria. The largest of these PAIs is a 133,740 base pair island containing several transposons, integrases, and eight genes with significant sequence homology to Legionella/Coxiella Type IV virulence/secretion apparatus (1). Seven of the twelve PAIs contain genes that encode proteins or efflux pumps that confer drug resistance to A. baumanniii, although many strains of A. baumanniidevelop additional drug resistance genes through the evolutionary pressures of treatment with pharmaceuticals (1).
In addition to the virulence-conferring genes of the A. baumannii PAIs, the pAs obtained by the bacterium from the outside environment include genes for heavy metal resistance, iron metabolism, quorum sensing capabilities, lipid metabolism, amino acid uptake, and genes for the breakdown of xenobiotics (1).
Of paramount importance to the pathogenic potential of A. baumannii are the plethora of antibiotic resistance genes contained within its genome. The AYE strain of A. baumannii has a 86,190 base pair PAI inserted into its genome that contains 45 of its 52 drug resistance genes (2). Similarly, a more recent isolate, the ATCC17978 strain of A. baumannii contains a 13,277 base pair PAI that contains 74 drug resistance genes, 32 efflux pumps, 11 genes related to drug/metabolite transporters (DMTs), as well as 26 genes encoding resistance to a variety of heavy metals, including copper, cadmium, zinc, and arsenic (1). The drug resistance genes on the PAI of this strain confer resistance to several classes of antibiotics, including β -lactams, aminoglycosides, fluoroquinolones, chloramphenicol, tetracycline, and rifampin (2). Genomic comparisons of the AYE and ATCC17978 A. baumannii strains suggest that the ATCC17978 strain has disposed of some of the drug resistance genes observed in the AYE strain in order to evolve a potent drug resistance cassette observed in its genomically inserted PAI (1). It is clear from these genomic analyses that the ability to obtain foreign DNA from environmental sources has proven immensely important in the development of A. baumannii pathogenesis. It is likely that this pathogen will continue to optimize its virulent potential through the attainment, integration, and use of foreign genes.
Cell Structure

A. baumannii is a gram-negative, non-motile, rod-shaped bacterium. Like other species of Acinetobacter, A. baumannii contains a cell envelope with multiple layers, including an outer membrane and inner cytoplasmic membrane separated by a layer of periplasmic space (4).
Unique to A. baumannii is the small amount of porins in the cell membrane. In bacterial cells, porins allow for the transport of various molecules across the lipid membrane. Various cellular functions and consequences have been attributed to the presence of porins in the membrane, some helpful and others detrimental to subsistence. In some cases, porins can permit cells to adhere to other bacterial cells (such as in the formation of biofilms). Nonetheless, porins can allow the entry of antibiotic and other antimicrobial compounds across the cell membrane and into the cytoplasm, where they disrupt normal enzymatic processes or destroy cellular structures and organelles (5). The decreased porin expression observed in A. baumannii has been viewed as another mechanism by which this pathogen sustains resistance to antibiotics and antimicrobial agents, by simply preventing these compounds from entering the cell. For example, A. baumannii has been able to become resistant to imipenem and carbapenem antibiotics by eliminating several porins, including porin CarO, as well as another porin that seems to share significant sequence homology with the OprD porin found in other gram negative bacteria (6,7).
In addition to porins, scattered in the membrane of A. baumannii are efflux pumps that allow for the removal of organic compounds, as well as antibiotic or antimicrobial agents that could prove detrimental to the cell. There are several classes of efflux pumps, however, the majority of drug efflux pumps found in A. baumannii belong to either the Major Facilitator Superfamily (MFS) or the Resistance-Nodulation-Division (RND) family. These efflux pumps operate by proton motive force expulsion (5).
Also found in the cell membrane of A. baumannii are protein channels and transporters involved in the uptake of foreign DNA (Figure 4). Located in the outer membrane is PilQ, which allows initial entry of foreign DNA. The DNA is then bound by ComE, and is transported through the periplasmic space by PilE, or the type IV pilus to the ComA transmembrane protein located in the inner membrane. Transport through ComA allows the DNA to enter the cytoplasm of A. baumannii. Once inside the cell, this foreign DNA is either degraded, integrated into the genome, or exists as a plasmid (1).
Of particular interest with regard to the cellular structure of A. baumannii is the bacteria’s outer membrane protein A (OmpA). OmpA has been associated with the ability of A. baumannii to form biofilms on both biological surfaces such as the human skin, as well as abiotic environments such as catheters and shunts (8). Furthermore, OmpA is believed to be a major component of the mechanism by which A. baumannii invades epithelial cells. OmpA allows A. baumannii to adhere and invade epithelial cells by a zipper-like mechanism that involves the motion of both microtubules and microfilaments (9).
Metabolism
A. baumannii are aerobic, non-fermentative, catalase-positive and oxidase-negative bacteria (10). Like other A. baumannii species, they are unable to reduce nitrate to nitrite. They obtain nitrogen from ammonium and nitrate salts. They are able to use various organic compounds for metabolism and energy production, including sugars, fatty acids, some amino acids, unbranched hydrocarbon chains, and some aromatic compounds (including aromatic amino acids). The use of sugars as a carbon source for metabolic pathways by A. baumannii is restricted to D-glucose, D-ribose, D-xylose, and L-arabinose (4).
D-glucose is metabolized by A. baumannii through the Etner-Doudoroff pathway. Pentoses used by A. baumannii in metabolism are degraded by an aldose dehydrogenase. The oxidized pentoic acids are then converted to α-ketoglutarate through several steps involving dehydration and dehydrogenation mechanisms (4).
The tri-carboxylic acid cycle in A. baumannii is similar to cycles observed in other proteobacteria. Several of the enzymes involved in TCA cycle steps have been purified from A. baumannii. The bacterium’s citrate synthase is composed of four identical subunits. A. baumannii’s aconitase has been shown to form glyoxylate from a citrate substrate. In addition to these enzymes, two NADP linked isocitrate dehydrogenases have been isolated, and are induced by glyoxylate or pyruvate. Finally, the α-ketoglutarate dehydrogenase complex of A. baumannii functions as it does in the TCA cycle of other organisms, with ATP exhibiting an inhibitory effect on the action of the complex, whereas ADP or AMP increase its activity and appropriately lower the Km of the enzyme (4).
A. baumannii can degrade aromatic compounds through the β-ketoadipate pathway, involving β-ketoadipate enol-lactone hydrolase and β-ketoadipate succinyl -CoA transferase as the primary metabolizing enzymes. Through this pathway, aromatic compounds are ultimately converted to succinic acid and acetyl-CoA (4).
A. baumannii uses the cytochrome system in its electron transport pathways, demonstrated by complete inhibition of NADH oxidase activity when the cells were treated with cyanide. Cytochrome a1, cytochrome a2, cytochrome b1, cytochrome c, as well as flavin have been shown to play a role in the electron transport pathways and cellular respiration of A. baumannii (4).
In nucleic acid metabolism, A. baumannii must use uracil as pyrimidine in both RNA and DNA synthesis. Because A. baumannii lacks the thymine phosphorylase and thymidine kinase enzymes, it cannot incorporate thymine into DNA molecules (4).
Epidemiology

A. baumannii causes approximately 2% to 10% of gram-negative bacterial infections observed in the United States and Europe (Figure 5)(2). Most infections are observed in health care settings, such as hospitals and nursing homes. Cases of A. baumannii infection have increased dramatically in the United States between 2002 and 2007 (12). These infections often involve immune-compromised patients. Major risk factors for A. baumannii infection include invasive procedures, such as those that involve mechanical ventilation devices, catheters, or shunts, open wounds, immune system impairment, long-term hospitalization, as well as the use of antibiotic and antimicrobial agents, to which A. baumannii can gain rapid resistance (11).
Non-specific nutritional requirements and resistance to desiccation permit A. baumannii to grow in various environments, and therefore initial contact with the pathogen preceding infection can be made in a variety of ways. A. baumannii is a natural inhabitant of the human skin flora. Human skin to skin contact has been suggested as a possible means of transmission of A. baumannii, especially in clinical settings (for example, transmission from a physician to an immune compromised patient without proper aseptic technique). However, further research is needed to confirm this route of transmission (11). Other studies have shown the ability of A. baumannii to colonize food including some raw fruits and vegetables, as well as some species of arthropods (11, 16). As a result of the food colonization studies, it has been suggested that another means of transmission may be through hospital food, as in some intensive care units digestive tract colonization accounts for 41% of A. baumannii cases (15).
The primary means of transmission is hypothesized to be the result of A. baumannii colonization on abiotic surfaces, such as plastic catheters and mechanical ventilators. Particularly high rates of transmission and infection are observed in hospital intensive care units, as would be expected with the highly compromised conditions patients would attain in order to warrant admission into the ICU (11, 13). In one study conducted in Spain, more than 90% of A. baumannii infections were acquired through hospitalization, while only 4% of infections were obtained from settings outside the hospital. Of the A. baumannii cases investigated, 39% were respiratory infections, 24% were abscess infections, and 23% were urinary tract infections. A. baumannii infection of the bloodstream was observed in only 3% of case studies (14). Another study conducted over a ten year period in the New England region suggested there may be seasonality to A. baumannii infection, with most infections occurring in the July through October period. Most of the A. baumannii infections during this period resulted in pneumonia or bloodstream infection (17).
Few studies have been performed on the mortality rates associated with A. baumannii infection. One study performed in a hospital intensive care unit suggested that A. baumannii infection resulted in a 7.8% increase in mortality among these patients. However, the statistical relevance of these findings has been challenged (11, 18). In a separate study, A. baumannii infection was shown to have no relevant effect on patient mortality rate. However, A. baumannii infection was shown to prolong a patient’s hospital stay by 4.5 days (19).
A. baumannii infection has been an epidemiological concern in hospitals for many years. Additionally, A. baumannii was the bacterium most isolated from open wounds during the Vietnam War. However, it wasn’t until the outbreaks of A. baumannii infection among soldiers serving in Iraq and Afghanistan that the pathogen garnered public attention. Between January 2002 and August 2004, A. baumannii was isolated from the blood of 102 soldiers being treated in military health care facilities. All of the soldiers had served in either the Afghanistan or Iraq regions, and it is believed that the majority of the cases were obtained through infection of open wounds (11).
Pathology

Although the exact molecular mechanism by which A. baumannii gains entry into host cells has yet to be elucidated, many theories suggest the use of outer membrane proteins. As stated previously, it is believed that OmpA, the most abundant cell membrane protein of A. baumannii, allows the bacteria enter epithelial cells by means of a zipper-like mechanism ( a form of receptor-mediated entry). In this mechanism, OmpA interacts with host cell membrane receptors. After OmpA binds to the receptor, the A. baumannii cell is surrounded and enclosed by the host cell membrane by means of cytoskeletal rearrangement involving the rearrangement of actin and components of the cellular membrane (9). Outer membrane protein 38 (Omp38) has also been suggested as another protein involved in the pathogenesis of A. baumannii. In a recent study, Omp38 was purified from A. baumannii and localized to the mitochondrial membrane of host epithelial cells. Omp38 also induced apoptosis of epithelial cells as a result mitochondrial disintegration upon Omp38 localization with the mitochondrial membrane. The results observed with purified Omp38 were replicated when the cells were infected with standard A. baumannii cells. This study promotes the idea that Omp38 contributes to the pathogenesis of A. baumannii by disintegrating the mitochondrial membrane, causing the release of pro-apoptotic molecules, eventually leading to host cell death (20).
A. baumannii can infect all organs, however infections are most often found in organs that have high fluid content, such as the lungs and associated respiratory structures, the bladder and other urinary tract structures, and the peritoneal fluid of the abdominal cavity (Figure 6) (11). The risk of infection increases dramatically when medical devices such as ventilators, endotracheal intubators, and catheters are inserted into these bodily tracts (21).
The most dangerous pathological consequences of A. baumannii result when the microbe infects the respiratory tract. Infection of the respiratory tract often results in a severe case of pneumonia for the patient. Symptoms of these A. baumannii- induced pneumonia cases are similar to those of other respiratory infections, including high fever or hypothermia, rigors, change in the color of septum, chest pain, and shortness of breath (21). Mortality rate from A. baumannii-induced pneumonia can range from 40-64% if the bacteria can be isolated from the blood or pleural effusions during the time of illness (21). Treating these cases of pneumonia has proven difficult for health care practitioners, as A. baumannii strains have gained resistance to most classes of antibiotics since the 1970’s. Nonetheless, a recent study found that imipenem antibiotics proved most effective in treating A. baumannii associated pneumonia. However, because imipenem resistance is increasing within A. baumannii strains, it has been found that intravenous administration of colistin is an effective alternative, although not preferred because of the compound’s nephrotoxic effect (22).
Multidrug-Resistance
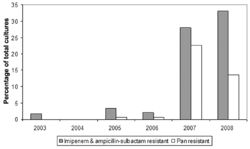
A. baumannii’s role as a dangerous emerging pathogen is most directly associated with its ability to quickly develop resistance to antibiotic and antimicrobial compounds (Figure 7). There are several mechanisms by which A. baumannii has been able to develop resistance to most classes of antibiotics. By reducing porin expression, increasing expression of certain transmembrane efflux pumps, and acquiring foreign DNA from the environment, including plasmids with a multitude of antibiotic resistance genes, enable A. baumannii to survive even the most aggressive pharmaceutical treatments (23, 24). Mechanisms of resistance to selected classes of antibiotics are detailed below.
Resistance to Tetracycline Antibiotics
A. baumannii have two transmembrane efflux pumps, TetA and TetB that allow for the efflux of tetracycline and closely related minocycline antibiotics (25). A. baumannii also has the TetM gene, whose protein product protects the bacterium’s ribosome from the action of tetracycline antibiotics (26).
Resistance to Polymixin Antibiotics
Colistin, described above in the treatment of A. baumannii associated pneumonia is an example of a Polymixin antibiotic. This class of antibiotics is the last means of defense against A. baumannii infection, because of the damaging effect these compounds can have on the kidneys. Recent studies have detailed cases of A. baumannii infection that did not respond to treatment with colistin or Polymixin B (27, 28). It is hypothesized that A. baumannii has become resistant to these antibiotics by modifying certain liposaccharide compounds in the cell membrane, preventing binding of the antibiotic to the cell membrane, as observed in Polymixin resistant strains of E. coli and Salmonella (29). Polymixin resistant A. baumannii strains show the great need for the development of new antibiotic agents.
Resistance to Quinolone Antibiotics
A. baumannii has developed resistance to quinolone antibiotics by modifying its DNA gyrase enzyme, lowering the affinity of the antibiotic for the DNA-gyrase complex (30).
Implications for Hospitals

Several epidemiological studies have confirmed that most cases of A. baumannii are obtained in hospitals or other healthcare facilities (14). Additionally, most cases are associated with long-term hospital stays or admittance to intensive care units. Without proper sterilization techniques, A. baumannii can colonize medical equipment and supplies. The identification of A. baumannii as an inhabitant of the skin flora suggests the possibility that this pathogen can be transmitted to patients from physical contact with their healthcare providers (11). The conditions that would warrant patient hospitalization are closely associated with immune impairment. The high concentrations of immune compromised patients, coupled with ideal growing surfaces (catheters, shunts, ventilators), and the physical contact required for adequate care make hospitals ideal environments for the spread of A. baumannii. The resistance of this microbe to most classes of antibiotics has made outbreaks of A. baumannii within hospitals even more frightening for patients and healthcare providers alike.
To avoid an epidemic of A. baumannii in hospital settings, appropriate measures must be taken to ensure that the medical devices that are inserted into the biological tracts of patients are sterilized effectively (Figure 8). Furthermore, practitioners must ensure that they are using sterile technique with all procedures. One study found that one hospital’s attempt to reduce person to person transmission by re-training staff members in proper glove changing and disposal, as well as a review of general sterile practice resulted in a decrease in cases of A. baumannii resulting from person to person transmission (31).
Future Work
It is with great urgency that novel pharmaceuticals be developed to combat multidrug-resistant strains of A. baumannii. However, this is no easy task. In 2010, 1040 new FDA approved drugs were screened for effectiveness in treating A. baumannii infections. Only 5 of these drugs (Thimerosal, Doxycycline, Polymyxin B sulphate, Rifaximin and Tyrothricin) showed antibacterial activity when A. baumannii was treated (32). Although these agents did eliminate A. baumannii infection, these drugs are all classic antibiotics; the initial aim of the study was to identify antimicrobial agents that A. baumannii would have a more difficult time developing resistance to. Nonetheless, none of the FDA-approved antimicrobial compounds tested had an effect on A. baumannii (32). Further research into the development of novel antimicrobial agents needs to continue in order to control outbreaks of A. baumannii.
References
1Smith, M.G.; Gianoulis, T.A.; Pukatzski, S.; Mekalanos, J.J.; ornston, L.N.; Gerstein, M.; Snyder, M. 2007. New insights into Acinetobacter baumannii pathogenesis revealed by high-density pyrosequencing and transposon mutagenesis Genes & Dev. 2007. 21: 601-614
2Fournier P.E.; Vallenet, D.; Barbe, V.; Audic, S.; Ogata, H. 2006 Comparative Genomics of Multidrug Resistance in Acinetobacter baumannii. PLoS Genet 2(1): e7. doi:10.1371/journal.pgen.0020007
3 Iacono, M.; Villa, L.; Fortini, D.; Bordoni, R.; Imperi, F.; Bonnal, R.J.P.; Sicheritz-Ponten, J.; DeBellis, G.; Visca, P.; Cassone, A.; Carattoli, A. 2008. Whole-Genome Pyrosequencing of an Epidemic Multidrug-Resistant Acinetobacter baumannii Strain Belonging to the European Clone II Group. Antimicrobial Agents and Chemotherapy 52(7): 2616–2625.
4 Juni, E. 1978. Genetics and Physiology of Acinetobacter. Ann. Rev. Microbiol. 32:349-371.
5 Vila, J.; Marti, S.; Sanchez-Cespedes, J. 2007.Porins, efflux pumps and multidrug resistance in Acinetobacter baumannii. 59(6):1210-1215.
6 del Mar Tomas, M.; Beceiro, A.; Perez, A.; Velasco, D.; Moure, R.; Villanueva, R.; Martinez-Beltran, J.; Bou, G. 2005. Cloning and Functional Analysis of the Gene Encoding the 33- to 36-Kilodalton Outer Membrane Protein Associated with Carbapenem Resistance in Acinetobacter baumannii. 49(12):5172-5175.
7 Mussi, M.A.; Limansky, A.S.; Viale, A.M. 2005. Acquisition of resistance to carbapenems in multidrug-resistant clinical strains of Acinetobacter baumannii: natural insertional inactivation of a gene encoding a member of a novel family of β-barrel outer membrane proteins. Antimicrob Agents Chemother. 49:1432-40.
8 Gaddy, J.A.; Tomaras, A.P.; Actis, L.A. 2009. The Acinetobacter baumannii 19606 OmpA Protein Plays a Role in Biofilm Formation on Abiotic Surfaces and in the Interaction of This Pathogen with Eukaryotic Cells. Infect Immun.77(8): 3150–3160.
9 Choi, C.H.; Lee, J.S.; Lee, Y.C.; Park, T.I.; Lee, J.C. 2008. Acinetobacter baumannii invades epithelial cells and outer membrane protein A mediates interactions with epithelial cells. BMC Microbiology 8(216):1-11.
10 Van Looveren, M.; Goossens, H.; ARPAC Steering Group. 2004. Antimicrobial resistance of Acinetobacter spp. in Europe. Clinical Microbiology and Infection 10(8): Article first published online: 9 AUG 2004
11 Fournier, P.E.; Richet, H. 2006. The Epidemiology and Control of Acinetobacter baumannii in Health Care Facilities. Health Care Epidemiology 42(1):692-699.
12 Miller, L.A.; Mera, R.; Amrine-Madsen, H.; Sahm, D.F. 2009. Marked increase of Acinetobacter baumannii resistance to multiple antibiotics during the period 2002-2007 in a large US surveillance study. Biometrics. September 2009:C2-622.
13 Apisarnthanarak, A.; Pinitchai, U.; Thongphubeth, K.; Yuekyen,C.; Warren, D.K.; Fraser, V.J. 2008. A Multifaceted Intervention to Reduce Pandrug-Resistant Acinetobacter baumannii Colonization and Infection in 3 Intensive Care Units in a Thai Tertiary Care Center: A 3-Year Study. Clin Infect Dis.47(6):760-767.
14 Rodriguez-Bano, J.; Cisneros, J.M.; Fernandez-Cuenca ,F. 2004. Clinical features and epidemiology of Acinetobacter baumannii colonization and infection in Spanish hospitals. Infect Control Hosp Epidemiol 25:819–824.
15 Corbella ,X.; Pujol, M.; Ayats, J. 1996. Relevance of digestive tract colonization in the epidemiology of nosocomial infections due to multiresistant A. baumannii. Clin Infect Dis 1996; 23:329–334.
16 La Scola, B.; Raoult, D. 2004. Acinetobacter baumannii in human body louse. Emerg Infect Dis 10:1671–1673.
17 Mc Donald, C.L.; Banerjee, S.N.; Jarvis W.R. 1999. Seasonal variation in Acinetobacter infection: 1987–1996. Clin Infect Dis 29:1133–1137.
18 Blot, S.; Vandewoude, K.; Colardyn, F. 2003. Nosocomial bacteremia involving Acinetobacter baumannii in critically ill patients: a matched case-control study. Intensive Care Med 29:471–475.
19 Daniels, T.L.; Deppen, S.; Arbogast, P.G.; Griffin, M.R.; Schaffner, W.; Talbot, T.R. 2008. Mortality rates associated with multidrug-resistant Acinetobacter baumannii infection in surgical intensive care units. Infect Control Hosp Epidemiol.29(11):1080-1083.
20 Choi, C.H.; Lee, E.Y.; Lee, Y.C.; Park, T.I.; Kim, H.J.; Hyun, S.H.; Kim, S.A., Lee, S.K., Lee, J.C. 2005. Outer membrane protein 38 of Acinetobacter baumannii localizes to the mitochondria and induces apoptosis of epithelial cells. Cell Microbiol.7(8):1127-1138.
21 Chen, M.Z.; Hsueh, P.R.; Lee, L.N.; Yu,C.J.; Yang, P.C.; Luh, K.T. 2001. Severe community-acquired pneumonia due to Acinetobacter baumannii. Chest. 120(4):1072-1077.
22 Garnacho-Montero, J.; Ortiz-Leyba, C.; Jiménez-Jiménez, F.J.; Barrero-Almodóvar, A.E.; García-Garmendia, J.L.; Bernabeu-Wittel, I.M.; Gallego-Lara, S.L.; Madrazo-Osuna J. 2003. Treatment of multidrug-resistant Acinetobacter baumannii ventilator-associated pneumonia (VAP) with intravenous colistin: a comparison with imipenem-susceptible VAP. Clin Infect Dis.36(9):1111-1118.
23 Fernández-Cuenca, F.; Martínez-Martínez, L.; Conejo, M.C.; Ayala, J.A.; Perea, E.J.; Pascual, A. 2003. Relationship between beta-lactamase production, outer membrane protein and penicillin-binding protein profiles on the activity of carbapenems against clinical isolates of Acinetobacter baumannii. J Antimicrob Chemother. 51(3):565-574
24Poole, K. 2005. Efflux-mediated antimicrobial resistance. J Antimicrob Chemother. 56(1):20-51.
25 Huys, G.; Cnockaert, M.; Vaneechoutte, M.; Woodford, N.; Nemec, A.; Dijkshoorn, L.; Swings, J. 2005. Distribution of tetracycline resistance genes in genotypically related and unrelated multiresistant Acinetobacter baumannii strains from different European hospitals.Res Microbiol. 156(3):348-355
26 Ribera, A.; Ruiz, J.; Vila, J. 2003. Presence of the Tet M determinant in a clinical isolate of Acinetobacter baumannii. Antimicrob Agents Chemother.47(7):2310-2312.
27 Gales, A.C.; Reis, A.O.; Jones, R.N. 2001. Contemporary assessment of antimicrobial susceptibility testing methods for polymyxin B and colistin: review of available interpretative criteria and quality control guidelines. J Clin Microbiol. 39(1):183-190.
28 Reis, A.O.; Luz, D.A.; Tognim, M.C.; Sader, H.S.; Gales, A.C. 2003. Polymyxin-resistant Acinetobacter spp. isolates: what is next? Emerg Infect Dis.9(8):1025-1027.
29 Peterson, A.A.; Fesik, S.W.; McGroarty, E.J. 1987. Decreased binding of antibiotics to lipopolysaccharides from polymyxin-resistant strains of Escherichia coli and Salmonella typhimurium. Antimicrob Agents Chemother. 31(2):230-237.
30 Vila, J.; Ruiz, J.; Goñi, P.; Jimenez de Anta, T. 1997. Quinolone-resistance mutations in the topoisomerase IV parC gene of Acinetobacter baumannii. J Antimicrob Chemother. 39(6):757-762.
31 Scerpella, E.G.; Wanger, A.R.; Armitige, L.; Anderlini, P.; Ericsson, C.D. 1995. Nosocomial outbreak caused by a multiresistant clone of Acinetobacter baumannii: results of the case-control and molecular epidemiologic investigations. Infect Control Hosp Epidemiol. 16(2):92-7.
32 Chopra, S.; Torres-Ortiz, M.; Hokama, L.; Madrid, P.; Tanga, M.; Mortelmans, K.; Kodukula, K.; Galande, A.K. 2010. Repurposing FDA-approved drugs to combat drug-resistant Acinetobacter baumannii. J Antimicrob Chemother.65(12):2598-2601
Edited by Kerri-Lynn Conrad, student of Joan Slonczewski for BIOL 238 Microbiology, 2011, Kenyon College.
