Coxsackievirus A16

Etiology/Bacteriology
Taxonomy
ssRNA positive-strand viruses, no DNA stage
| Order = Picornavirales
| Family = Picornaviridae
| Genus = Enterovirus
| species = Enterovirus A
{|NCBI: Taxonomy Genome: Genome|}
Description
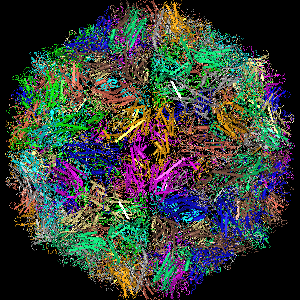
Coxsackievirus belongs in the Picornaviridae family that includes polioviruses and non-polioviruses. The Coxsackievirus is a non-poliovirus. Coxsackieviruses have two groups, group A and group B. Group A includes Coxsackievirus A16 (CA16), which is a common cause of hand, foot, and mouth disease (HFMD) in children under the age of 5. CA16 is a small, non-enveloped, icosahedral particle with a single positive-stranded genomic RNA.[2] Some symptoms that might occur are fevers, rashes on hands and feet, and blister like sores in the mouth. The symptoms last around a week, and then disappear. [3] CA16 is transmitted via the fecal-oral route, or oral-oral route. Although there are HFMD cases around the world, Asia currently has the most outbreaks. CA16 causes a mild and, sometimes, asymptomatic version of HFMD. Serious cases lead to meningitis, conjunctivitis, myocarditis, and pericarditis.
Pathogenesis
Epidemiology
The first coxsackievirus was isolated in 1948 in Coxsackie, New York. [4] In 1955 CA16 was first isolated in South Africa, and then sequenced in 1994. [5] Coxsackievirus A16 normally affects children 10 and younger, but children under 5 have significant susceptibility. [5] There have been adults infected with CA16 as well. It is all around the world, but mostly during the warmer seasons. Areas around the equator experience cases all year because of the heat. It is highly contagious, and 50% of HFMD cases are caused by CA16. Many recent reports have been in the Western Pacific region. In 1998 Taiwan had an outbreak of HFMD with 1.5 milllion cases, but only 78 children died. [6] China had 1844 people infected with HFMD in 2011-2012 and 422 of them had CA16 infections only, while 38 had CA16 and EV71 infections. Southern Viet Nam had an outbreak of HFMD in 2005 including 214 cases of CA16 infection. [6] There have not been many cases relating myocarditis and CNS damage to coxsackievirus A16, but it can happen.
Transmission
Spreading of CA16 infections results from contact with an infected person’s saliva, feces, respiratory aerosols, or contaminated water. Children 5 and under are the most susceptible to CA16 infection because their immune systems are not fully equipped. The first week of infection is when a person is most contagious. An infected person’s feces can be infected with CA16 even after the symptoms clear up. [7]
Incubation and Infectious Dose
Exposure of the coxsackievirus A16 happens 3 to 6 days before the symptoms begin. [8] An infectious dose for CA16 is not known right now. Because CA16 does not cause severe symptoms of HFMD, not much research has been done about its infectious dose or vaccine. Replication begins in the upper respiratory tract, and also occurs in the submucosal lymph tissue. [9] Since CA16 replicates and invades the submucosal layers it can go into the blood stream and target organs.
Virulence Factors
Virulence factors for CA16 are being researched. As of right now, 3C proteases are known to play an important role in viral replication.[10] CA16 viral replication activates the mitochondrial pathway related caspase 9 protein and the Fas death receptor pathway related caspase 8 protein causing apoptosis of the host cell. DNA fragmentation is caused by a CA16 infection, and it is also a key feature of apoptosis.[10] The CA16 mechanism is still unclear. It is known that nonstructural proteins 2C and 3C inhibit the fusion of autophagosomes with lysosomes, which prevents the viral RNA to be degraded. CA16 uses autophagy to help its own replication. [11]
Clinical Features

Symptoms
CA16 is one of the most common causes of hand, foot, and mouth disease (HFMD). The majority of CA16 infections in HFMD are asymptomatic, but some cause a fever, poor appetite, and a sore throat. Painful sores can develop in the mouth (herpangina). Rashes are mainly on the palms of hand and soles of feet, but can be on knees, elbows, buttocks, or genital areas. Dehydration is a major concern because of the pain experienced from swallowing. HFMD normally happens in children under 5, but adult cases have been recorded. HFMD is prominent during the warmer months, and the symptoms clear up in about a week without treatment. [3]
Serious cases of HFMD caused by CA16 can lead to myocarditis or meningitis; these cases are very rare. There has been one report that linked a CA16 infection with 15-month-old boy that died from myocarditis and intactable shock.[12]
Diagnosis
The majority of physicians diagnose HFMD based on the symptoms that are present. To diagnose a CVA16 infection, throat swabs and fecal specimen are collected. Viral tests can also be used to identify CVA16, but they are rarely done because they are expensive and it takes two weeks to get the results back. Since the symptoms clear in a week, viral tests are not done unless there are serious complications.[8]
Treatment
Because coxsackievirus A16 is self-limiting, the symptoms disappear after 7 to 10 days without any treatment. Physicians will prescribe symptomatic treatments for infected individuals. Acetominophen (Tylenol) can reduce the fever, and some pain. Sometimes Lidocain oral gel, benzydamine spray, mouthwash, or choline salicylate oral gels are recommended for mouth and throat ulcers. Preventing dehydration by adequate fluid intake is encouraged. [13] An antiviral chemical used to treat herpes simplex, acyclovir, was used to successfully treat CA16, but the study was inconclusive.[14]
Prevention

Coxsackievirus A16 infection is very contagious, and can be prevented. To prevent infection of CVA16, good hygiene must be practiced. Hands need to be washed after using the toilet, changing diapers, before preparing food, etc. Children should be taught proper hygiene and hand washing to avoid infection and spreading of CA16. Other preventative measures include covering of one’s nose and mouth when coughing or sneezing, and not sharing cups, eating utensils, or towels with an infected person. Sterilization of toys, beds, changing tables, and eating utensils should be performed at child day cares and houses.[13] Repeated infections are not typical, but they are possible because HFMD can also be caused by other strains of coxsackieviruses and enterovirus 71.
Vaccination
There is current research being done on making a vaccine for coxsackievirus A16. One study found that sera from infected patients or immunized animals block the cytopathic effects caused by CA16. Immunization with an inactive vaccine of CA16 causes neutralization antibodies to work against CA16 in mice. [2]
Human Immune Response
The mechanism and pathogy for coxsackievirus A16 are currently unknown, but research is being done to understand them. One article stated that IgM works against CA16. [14] IgM is good at triggering complement that causes membrane attack complex, inflammation, and opsinization. The membrane attack complex causes a cell to lysis and die, while opsinization coats the pathogen for macrophages to phagocytose and destroy the virus. A coxsackievirus-specific secretory IgA antibody has been seen in the throat and intestines of infected patients after the infection has cleared. [15] Another study reported that there were more T helper 1 cells, and plasma IFN-gamma and IL-17A levels, making the T helper cells unbalanced. White blood cell counts, neutrophil differentiation, maturation, and migration also increased with CA16 infection. [16] Much more research is to be done on CA16, and it's effects.
References
1. College of Arts and Sciences | The University of Oklahoma. Study Abroad.
2.Qunying Mao, Yiping Wang, Xin Yao, Lianlian Bian, Xing Wu, Miao Xu & Zhenglun Liang (2014) Coxsackievirus A16, Human Vaccines & Immunotherapeutics, 10:2, 360-367. http://dx.doi.org/10.4161/hv.27087
3. http://www.austincc.edu/microbio/2993k/cox.htm
4. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3381541/
5. http://www.cdc.gov/hand-foot-mouth/about/signs-symptoms.html
6. http://www.wpro.who.int/publications/docs/GuidancefortheclinicalmanagementofHFMD.pdf
7. http://www.medicinenet.com/coxsackie_virus/page3.htm
8. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3764954/
9. http://emedicine.medscape.com/article/215241-overview#showall
10. http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0111174
11. http://www.ncbi.nlm.nih.gov/pubmed/25853521
12. http://www.researchgate.net/publication/6910582_Fatal_coxsackievirus_A16_infection
13. http://www.cdc.gov/hand-foot-mouth/about/prevention-treatment.html
14. http://www.biomedcentral.com/content/pdf/1471-2180-11-246.pdf
15. Nahmias A, O'Reilly R. 1982. Immunology of human infection. Plenum Medical, New York.
16. http://www.spandidos-publications.com/etm/9/6/2213
Created by Sarah Steckler, student of Tyrrell Conway at the University of Oklahoma.
