Mycoplasma Salivarium
Classification
Bacteria; Mycoplasmatota; Mollicutes; Mycoplasmatales; Mycoplasmataceae
Species
|
NCBI: [1] |
Mycoplasma Mycoplasma salivarium
Description and Significance
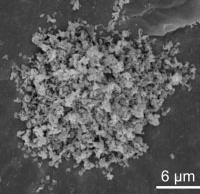
The smallest known species of bacterium is Mycoplasma salivarium (type strain 23064), commonly known as Asterococcus salivarius or Schizoplasma salivarium. Since they lack a cell wall, they are susceptible to several conventional antibiotics like penicillin. Binary fission allows M. salivarium to multiply, but because division is not always timed with genome replication, multinucleate filaments and various forms can emerge. They have a diameter of between 200 and 250 nm and are approximately spherical or bottle-shaped. It is thought to be a communicational organism and a component of the oral flora because it is present in practically every mouth of a healthy population (Kornspan et al., 2013).
However, M. salivarium has also been linked to periodontal disease, septic arthritis, eye and ear diseases, and oral infections. This species has been isolated from the synovial fluid of both monkeys and people with chronic arthritis. It came from a biliary stent and was recovered. Additionally, it was found in the pleural cavity of a man who was hospitalized and did not react to the standard course of therapy with conventional antibiotics. It also has been grown from brain abscesses. Recently, it has been reported as a prevalent occurrence in patients with ventilator-acquired pneumonia, a severe illness that can occur in ICU patients, and it may have a role in reducing the immune response to other pathogens, allowing opportunistic infections to develop.
Genome Structure
There is growing evidence that the CRISPR/Cas systems in the human oral microbiome contain not just a canonical immune defense mechanism, but also multiple alternative mechanisms that can affect bacterial physiological functions like DNA repair, resistance gene acquisition, regulation of interspecific competition and intraspecific diversification, and gene expression regulation.
Under the right circumstances, several Mycoplasma species have been reported to fuse with the host cells, during which the host cells' ability to function is compromised. It was assumed that the essential element supporting this process was the presence of mycoplasma nucleases, which may destroy the DNA of host cells. The presence of bottle-shaped M. salivarium cells in epithelial cells under electron microscopy indicated a fusion between the mycoplasma cells and the host cells' cytoplasm. The replication-associated recombination protein A (rarA) gene and the F0F1 ATP synthase subunit epsilon (ATP5F1E) gene are where the M. salivarium CRISPR/Cas system is situated. Researchers also discovered that the cas9 gene is disrupted by a frameshift mutation, which results in a UAA stop codon in the midst of the cas9 gene sequence. The crRNA-guided endonuclease activity of cas9 may be compromised by this frame-shift mutation (Mizuki et al., 2022).
Cell Structure, Metabolism and Life Cycle
The genomes contain just 475 to 1,545 protein-coding sequences, which is a tiny number. By scavenging both free reactive oxygen and nitrogen species, M. salivarium significantly decreased oxidative stress. In the presence of tannic acid, red blood cells, or mucin, M. salivariums oxidant scavenging capacity was significantly boosted and was primarily restricted to the cytosolic fraction. The ability of M. salivariums cytoplasm to scavenge oxidants was heat stable and unaffected by sodium azide or extended proteolysis. According to research, lipase-digested lecithin is a crucial component of filmmaking (Thoendel et al., 2017).
Ecology and Pathogenesis
Mycoplasmas are crucial for plant, animal, and human health as well as for agriculture. Each cell has only one copy of the 16S rRNA and 23S rRNA. M. salivarium is said to prefer the sulci of the gingiva. Due to evidence that the organism exists in the oral cavity of edentulous (toothless) subjects, it alternately colonizes on other areas like the pharynx and the dosum of the tongue. Subjects with and without various oral disorders provided saliva samples, which researchers tested for mycoplasmas in. There was a substantial difference in viable counts only between teenagers and each of the other age groups, but not between age groups other than the teenagers. Viable counts appeared to rise with age up until the twenties and then not change as much beyond that.
M. salivarium is thought to engage in a number of metabolic processes that let it attack host tissues and evade phagocytosis. Human gingival fibroblasts and peripheral blood mononuclear cells are stimulated by M. salivarium to produce interleukin-6 (IL-6), IL-8, IL-1, and tumor necrosis factor alpha. These cytokines' secretion is a crucial phase of immunological and inflammatory responses. Periodontal disorders are known to be related with IL-1 and IL-6 in particular (Ichimaru et al., 1979).
M. salivarium has been found to invade the epithelial cells of oral leukoplakia in immunohistochemistry and immunoelectron microscopy investigations. The underlying mechanism of oral leukoplakia, an oral potentially malignant condition, is still unknown. It is characterized by a variety of site-specific chromosomal abnormalities and gene changes in epithelial cells. Also unknown is the connection between M. salivarium in epithelial cells and the onset or progression of oral leukoplakia (Shibata et al., 1997).
References
Henrich, Birgit & Schmitt, Marcus & Bergmann, Naomi & Zanger, Klaus & Kubitz, Ralf & Häussinger, Dieter & Pfeffer, Klaus. (2009). Mycoplasma salivarium detected in a microbial community with Candida glabrata in the biofilm of an occluded biliary stent. Journal of medical microbiology. 59. 239-41. 10.1099/jmm.0.013110-0.
Ichimaru, H., & Nakamura, M. (1979). The Components of Mycoplasma salivarium and its Growth Medium that are Responsible for Film Formation. Journal of General Microbiology, 112(2), 389–392. https://doi.org/10.1099/00221287-112-2-389
Kornspan, J. D., Ginsburg, I., & Rottem, S. (2013). The oxidant scavenging capacity of the oral Mycoplasma salivarium. Archives of oral biology, 58(10), 1378–1384. https://doi.org/10.1016/j.archoralbio.2013.05.001
Mizuki, H., Shimoyama, Y., Ishikawa, T., & Sasaki, M. (2022). A genomic sequence of the type II-A clustered regularly interspaced short palindromic repeats (CRISPR)/CRISPR-associated system in Mycoplasma salivarium strain ATCC 29803. Journal of oral microbiology, 14(1), 2008153. https://doi.org/10.1080/20002297.2021.2008153.
Shibata, K. I., Hasebe, A., Sasaki, T., & Watanabe, T. (1997). Mycoplasma salivarium induces interleukin-6 and interleukin-8 in human gingival fibroblasts. FEMS Immunology &Amp; Medical Microbiology, 19(4), 275–283. https://doi.org/10.1111/j.1574-695x.1997.tb01097.x
Thoendel, M., Jeraldo, P., Greenwood-Quaintance, K. E., Chia, N., Abdel, M. P., Steckelberg, J. M., Osmon, D. R., & Patel, R. (2017). A Novel Prosthetic Joint Infection Pathogen, Mycoplasma salivarium, Identified by Metagenomic Shotgun Sequencing. Clinical Infectious Diseases, 65(2), 332–335. https://doi.org/10.1093/cid/cix296
Author
Page authored by Kristina T., student of Prof. Bradley Tolar at UNC Wilmington.
Winner: 2022 People's Choice Award