The Gut-Brain Axis and OCD
Introduction
By Ali Hatfield
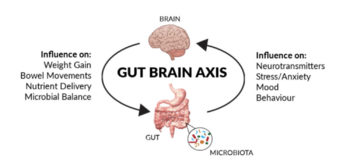
The systems of the human body are connected in many more ways than the average person could think of. At first thought the digestive system, commonly referred to as the human gut, is deeply separated from the nervous system. However, recent research has shown that this is not the case, and there are many more connections between the two than most would imagine. Studies have shown correlations between human gut microbial activity having an effect on psychological well-being, either improving or declining mental health. In cases with a direct connection between gut microbiota and brain activity, this is known as the gut-brain axis. This communication from bowel to brain is bidirectional, with interference in the gut microbiota having the ability to alter the nervous system, and interference with the nervous system having the ability to alter gut activity. [1]
The gut microbiota can affect a variety of psychological disorders, one of which being obsessive compulsive disorder (OCD). OCD is an anxiety related disorder that is believed to affect about 1% of the population, yet the number of diagnoses is hard to perfect in the case of psychological conditions.[2] It is reportedly more frequently found in women than in men in adults (age >18) and more frequently found in boys than girls (age <18).[2] Like many psychological disorders, obsessive compulsive disorder is a condition that displays a wide range of symptoms and manifests itself differently in each person afflicted by the disorder.
Sample citations: [3]
[4]
A citation code consists of a hyperlinked reference within "ref" begin and end codes.
To repeat the citation for other statements, the reference needs to have a names: "Cite error: Closing </ref> missing for <ref> tag Primarily, while the restoration of a healthy concentration of gut bacteria is likely to have beneficial effects, if the homeostatic conditions are not maintained it can cause relapse. To prevent this, a regular routine of probiotic administration would likely be necessary, which may defeat the purpose of using the microbiota as treatment if people are attempting it as an alternative to daily medication, such as SSRIs. Additionally, conditions that are impairing proper bacterial colonization in the gut must be remedied, and if the original issue in the gut is deriving from the central nervous system, this may create a negative cycle that prevents restoration of the gut microbiota. Often, OCD sufferers have had their obsessions and compulsions for an extended period of time to the point that they have solidified in their regular lifestyle or routine. In cases such as these, improving microbial health in the gut to combat the biological basis of OCD might not be enough to alleviate the psychological symptoms.
Conclusion
Research shows an undeniable connection between the human gut microbial community and the central nervous system, creating a bidirectional axis that affects each other regularly. Most well known is the correlation between gut health and depression and anxiety, but the correlations do not stop there. While there is less literature on the link between obsessive compulsive disorder and the gut-brain axis, enough is present to push the momentum forward on researching this topic. OCD is an illness that causes significant interference in the lives of those inflicted with it, and in order to treat it it needs to be fully understood. The hypothalamic-pituitary-adrenal axis and effect of antibiotics initially demonstrate this relationship, with the high overlap in OCD and IBS patients also supporting this. In short, gut microbiota dysregulation affects psychological well-being, with OCD being an example of the disorders it can cause or exacerbate. With this information, we can look into possible therapeutic interventions from the perspective of the gut microbiota, rather than just psychopharmacological options. Further research is needed to reach these steps, but as more is learned about the connection between gut and brain, massive scientific breakthroughs will follow.
References
- ↑ [https://doi.org/10.1016/j.cgh.2018.10.002 Osadchiy, V., Martin, C. R., & Mayer, E. A.. (2019). The Gut–Brain Axis and the Microbiome: Mechanisms and Clinical Implications. Clinical Gastroenterology and Hepatology, 17(2), 322–332.]
- ↑ 2.0 2.1 [1]
- ↑ Hodgkin, J. and Partridge, F.A. "Caenorhabditis elegans meets microsporidia: the nematode killers from Paris." 2008. PLoS Biology 6:2634-2637.
- ↑ Bartlett et al.: Oncolytic viruses as therapeutic cancer vaccines. Molecular Cancer 2013 12:103.
Authored for BIOL 238 Microbiology, taught by Joan Slonczewski, 2022, Kenyon College
