Pseudomonas aeruginosa infection
Etiology/Bacteriology
Taxonomy
| Domain = Bacteria
| Phylum = Proteobacteria
| Class = Gamma Proteobacteria
| Order = Pseudomonadales
| Family = Pseudomonadaceae
| Genus = Pseudomonas
| species = Pseudomonas aeruginosa
Description
Pseudomonas aeruginosa is an opportunistic pathogen commonly found in the environment mainly in soil and water, but is also regularly found on plants and sometimes on animals, including humans. It is a Gram-negative, rod-shaped bacterium that is motile by means of a single polar flagellum and known to be highly antibiotic resistant and able to grow in a variety of generally inhospitable environments, often through its ability to form resilient biofilms[1]. The bacteria often produce the blue-green pigment pyocyanin, a redox-active phenazine, which is known to kill mammalian and bacterial cells through the generation of reactive oxygen intermediates [2]. Pseudomonas infections often have a characteristic sweet odor and have become a substantial cause of infection in patients with immunodeficiencies. It is one of the main agents of hospital-acquired infections such as pneumonia, urinary tract infections (UTIs), and bacteremia [3].
Pathogenesis
P. aeruginosa is an opportunistic pathogen that rarely causes disease in healthy individuals. Most infections are able to take hold by the loss of the integrity of a physical barrier to infection (eg, skin, mucous membrane) or the presence of immune deficiency. This bacterium has also minimal nutritional requirements and can tolerate a wide variety of physical conditions like temperatures up to 41 degrees Celsius.
Transmission
Pseudomonas aeruginosa is a common inhabitant of soil, water, vegetation, and animals. It is found on the skin of some healthy persons and has been isolated from the throat (5 percent) and stool (3 percent) of non-hospitalized patients [3]. In some studies, gastrointestinal carriage rates increased in hospitalized patients to 20 percent within 72 hours of admission.
P. aeruginosa finds numerous reservoirs in a hospital setting such as disinfectants, respiratory equipment, food, sinks, taps, toilets, showers and mops. Because of its ubiquity, it is constantly reintroduced into the hospital environment on food, visitors, and patients transferred from other facilities. Transmission occurs from patient to patient on the hands of healthcare workers, by patient contact with contaminated reservoirs, and by the ingestion of contaminated materials [1].
Infectious dose, incubation, and colonization
The infectious dose of P. aeruginosa is unknown, as it is an opportunistic pathogen that can colonize healthy hosts without disease. Likewise, the incubation period is disputed, as the infection can manifest in many ways depending upon the site of infection. The pathogenesis of Pseudomonas is multifactorial and complex because Pseudomonas species are both invasive and toxigenic. The 3 stages are (1) bacterial attachment and colonization, (2) local infection, and (3) bloodstream dissemination and systemic disease [2]. The importance of colonization and adherence is most evident when studied in the context of respiratory tract infection in patients that need complicate mechanical ventilation, such as those with cystic fibrosis. [3]
Epidemiology
Frequency
The Centers for Disease Control and Prevention (CDC) has estimated the overall prevalence of P. aeruginosa infections in US hospitals at approximately 4 per 1000 discharged patients (0.4%). P. aeruginosa accounts for 10.1% of all hospital-acquired infections and is also the fourth most commonly isolated nosocomial pathogen. [3]
Morbidity and Mortality
All P. aeruginosa infections are treatable and potentially curable, but fulminant infections, such as bacteremic pneumonia, sepsis, burn wound infections, and meningitis, generally have extremely high mortality rates. [medscape] These infections are a serious problem in patients with cancer, cystic fibrosis, and severe burns. The fatality rate in these patients is near 50 percent. [1]
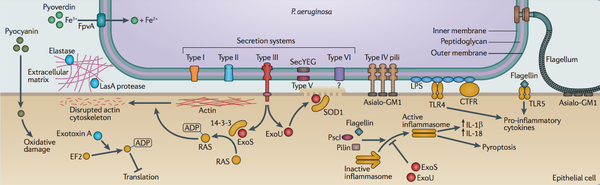
Virulence Factors
Virulence Factors P. aeruginosa has a variety of virulence factors that contribute to its ability to grow in various host environments and cause many different types of infections. These virulence factors include: adhesins, secreted toxins, proteases, effector proteins, and pigments, which distrupt or control host cellular pathways and target the extracellular matrix.
Adhesins
P. aeruginosa can adhere to the epithelial cells through use of its fimbriae, which bind to specific receptors on host epithelial cells, such as galactose, mannose, or sialic acid receptors. Colonization of the respiratory tract, for example, requires fimbrial adherence, so a protease enzyme may be used to help degrade the extracellular matrix and expose the appropriate receptors on the epithelial cell surface. Research has shown that tissue injury may be a crucial part of colonization of the respiratory tract, eyes, and urinary tract in a step called opportunistic adherence. Mucoid strains of Pseudomonas, which produce an exopolysaccharide seem to have an additional or alternative adhesin that attaches to mucin on the host cells, but the adhesins on the surface of Pseudomonas are not fully understood at this point. It is known that this exopolysaccharide is a repeating polymer of mannuronic and glucuronic acid, which is known as alginate. This alginate forms a slime that makes up the matrix of a Pseudomonas biofilm, an important part of both transmission and infection. This biofilm protects the cells from the host defenses and makes them less susceptible to antibiotics. These strains are most often found in the lungs of patients with cystic fibrosis.
Invasins
The production of extracellular proteases are important for P. aeruginosa’s virulence, especially in adherence and invasion of host cells [3]. There are two extracellular proteases, elastase and alkaline protease, associated with virulence and the pathogen’s invasive stage. Elastase cleaves collagen, IgG, IgA, and complement in addition to lysing fibronectin to expose receptors for bacterial attachment. It also has been shown to disrupt the respiratory epithelium and interfere with ciliary function. Both interfering with and lysing fibrin, alkaline protease is important, together with elastase, in destroying the extracellular matrix of the cornea and other structures composed of fibrin and elastin. Together, these two proteases also cause inactivation of gamma interferon (IFN) and tumor necrosis factor (TNF). P. aeruginosa also produces a pore-forming cytotoxin that is cytotoxic for most eukaryotic cells, but was originally called leukocidin for its effect on neutrophils. Pseudomonas also produces two hemolysins, a phospholipase and a lecithinase. These hemolysins work together to break down lipids and lecithin. These hemolysins, in conjunction with the cytotoxin, contribute to invasion of host cells through their cytotoxic effects on neutrophils, lymphocytes, and other eukaryotic cells. The blue pigment, pyocyanin, is an important determinant of virulence for Psuedomonas. It impairs the normal function of nasal cilia, disrupts respiratory epithelium, and instigates a proinflammatory response from phagocytes. Pyochelin, a derivative of pyocyanin, is a siderophore that allows the pathogen to sequester iron from the environment for growth. It is thought that this could play a role in invasion if the iron its sequestering is from the host in order to permit bacterial growth in an iron-limited environment.
Toxins
Two extracellular toxins, Exoenzyme S and exotoxin A, are important for the pathogenic activity of Pseudomonas aeruginosa. Exoenzyme S is like many other bacterial exotoxins in that it has the substructure of the A-component of a bacterial toxin in addition to its ADP-ribosylating activity. It is produced by pseudomonal infections in burned tissue and can often be found in the blood before bacteria are. This suggests that exoenzyme S acts to restrict the function of phagocytic cells in preparation for P. aeruginosa invasion. Exotoxin A causes ADP-ribosylation of eukaryotic elongation factor 2, which results in inhibited protein synthesis, which is the same mechanism of action as the diphtheria toxin. Despite this same mechanism of action, it is only partially identical to diphtheria toxin and antigenically-distinct. It does enter the cell in the same way and has the same enzymatic mechanism. The production of this toxin is regulated by environmental iron availablilty. It seems to mediate multiple levels of disease processes caused by an infection, such as its necrotizing activity at the site of bacterial colonization. Toxin-producing strains are more virulent and produce a more virulent form of pneumonia than those that don’t produce toxin. Purified exotoxin A is highly lethal to animals, including primates and humans.
Biofilms
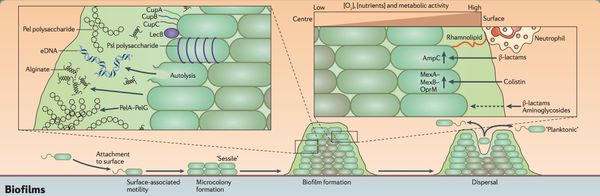
P. aeruginosa has an ability to develop incredibly hardy biofilms on many seemingly uninhabitable surfaces. After attachment to a surface, movement across that surface by twitching motility leads to the formation of microcolonies. Evolution of mature biofilm architecture depends on the biofilm matrix, which consists of the polysaccharides Pel, Psl, and alginate, extracellular DNA, and proteins, including CupA, CupB, and CupC fimbriae and LecB. These fimbriae mediate bacterial attachment during the initial stages of biofilm formation. The matrix delays diffusion of some antibiotics into the biofilm, effectively rendering it highly resistant to antibiotics. The oxygen and nutrient gradient in the biofilm affects this susceptibility to antibiotcis as well, as exposure to β-lactams or colistin can lead to the expression of resistance factors such as efflux pumps. [4]
Clinical features
Pseudomonal infections can involve any part of the body. They frequently create biofilms in the areas that they infect, which make the infection much harder to cure and more antibiotic resistant. Most often these infections are found in certain populations of patients such as those with intravenous lines, burns, cancer, cystic fibrosis, diabetes, catheters, surgery, trauma, and neonatal infants. [3]
Respiratory Tract
Nosocomially-acquired pneumonia often develops in patients with immunosuppression and chronic lung disease in the intensive care unit (ICU) setting, which can be primary, following aspiration of the organism from the upper respiratory tract, especially in patients on mechanical ventilation, and has a particularly high mortality rate [medscape, nature]. It may also occur as a result of a bacteremic infection spread to the lungs. This is observed commonly in patients following chemotherapy-induced neutropenia. P. aeruginosa is also commonly isolated from the respiratory tracts of cystic fibrosis patients and is often a cause of severe decline in these patients. Chronic lung colonization and infection also occur in patients with diseases affecting the airways of the lungs such as bronchiectasis and chronic obstructive pulmonary disease [4].
Central Nervous System
A P. aeruginosa infection in the CNS can cause meningitis and brain abscess, most often following an extension from a contiguous parameningeal structure, such as an ear, a mastoid, paranasal sinus surgery, or diagnostic procedures [3]. In some patients, a CNS infection is due to hematogenous spread of the organism from infective endocarditis, pneumonia, or UTI. Patients with a CNS infection present with fever, headache, and confusion. The onset of disease may be fulminant or somewhat less severe, a characteristic that usually depends on the immune status of the patient.
Ear
P. aeruginosa can also cause swimmer’s ear, and patients present with pain, which is worsened by friction on the ear, itching, and ear discharge. It is also is a common cause of chronic otitis media (middle ear infection). Malignant otitis externa (severe outer ear infection) is an invasive infection observed mostly in patients with uncontrolled diabetes. It begins as a normal outer ear infection, but after failing to respond to antibiotic treatment, the infection worsens. Symptoms usually include persistent pain, swelling, and tenderness of the soft tissues of the ear, with discharge, and some patients present with a facial nerve palsy. Extension of the infection can result in osteomyelitis and cranial nerve palsies, which can possibly lead to a CNS infection.
Eye
The most common Pseudomonas infection in nonimmunocompromised patients is in the eye. By producing extracellular enzymes that create a rapidly destructive lesion, it can cause bacterial keratitis (infection of the cornea), scleral abscess, and endophthalmitis (infection of the intraocular cavity) in adults and ophthalmia neonatorum in children [3,4]. Because the cornea, aqueous humor, and vitreous humor are a relatively immunocompromised environment, predisposing conditions such as trauma, contact lens use, preexisting ocular conditions, exposure to an ICU environment, and AIDS. Symptoms of an infection are pain, redness, swelling and impaired vision. Physical examination reveals swelling of the eyelid, redness and swelling of the conjunctiva, and a mucousal discharge.
Bones and Joints
Infections of the skeletal system most often involve the vertebral column, the pelvis, and the sternoclavicular joint. These infections are most often from either a blood-borne infection, which might stem from intravenous drug use, pelvic infections, or UTI, or contiguous from an open wound due to trauma, surgery, or a soft tissue infection. Those most at risk for these infections are those with puncture wounds to the foot, peripheral vascular disease, intravenous drug abuse, or diabetes. Skeletal infections manifest differently depending upon the location of the infection. Vertebral infections may involve the cervical spine, in which patients most often present with neck or back pain that can last from weeks to months and decreased range of motion. Patients with pyoarthrosis, or septic arthritis present with swelling and pain of the affected joint and a persistent fever. If a patient presents with neurological symptoms, spinal cord involvement is likely.
Gastrointestinal Tract
An aspect of Pseudomonal infections that is often underestimated, GI infections can affect every portion of the GI tract especially in very young children and adults with cancers and undergoing chemotherapy. The symptoms can range from very mild to severe necrotizing enterocolitis, which has significant morbidity and mortality. Young infants who may contract the disease in a nursery epidemic may present symptoms of irritability, vomiting, diarrhea, and dehydration. Shanghai fever is an enteritis manifestation of a pseudomonal infection, which presents with headache, fever, exhaustion, enlargement of the spleen, rose spots, and dehydration [3]. Typhlitis is most common in patients with neutropenia as a result of acute leukemia, which presents with sudden fever, abdominal distension, and abdominal pain.
Urinary Tract Infection
Most often, pseudomonal UTIs are hospital-acquired due to catheterization, instrumentation, and surgery. These UTIs can stem from an ascending infection or through bacteremic spread, in addition to being a source of bacteremia. It is impossible to distinguish a pseudomonal UTI from others without a urine culture and antibiotic susceptibility test.
Skin and Soft Tissue Infections
Thriving in wet environments only, Pseudomonas will flourish on moist skin, such as improperly attended wounds or skin frequently submerged in water, such as with green nail syndrome. Decubiti, pressure-induced ulceration of the skin, eczema, and athlete’s foot are the most frequent sites of secondary wound infections by Pseudomonas. Here is most often exhibited the characteristic blue-green pigment and fruity odor. Deep abscesses, cellulitis, and subcutaneous nodules may also occur. Burn victims are also highly susceptible to bacterial wound sepsis, which involves the proliferation of 100,000 organisms per gram of tissue, including the surrounding healthy tissue [3,4]. These burn infections often appear incredibly discolored, and symptoms may include fever, disorientation, hypotension, low urine production, bowel obstruction, and decreased white blood cell count. Improperly treated hot tubs and swimming pools are frequent sources of soft tissue and skin infections, with patients presenting with varying types of skin lesions called “hot tub folliculitis” on any part of the body submerged in the water.
Bacteremia
The mortality rate for pseudomonal bacteremia is greater than 10% and is most often acquired in a healthcare setting, with symptoms depending upon the primary site of infection. Most often these symptoms are fever, rapid breathing, and rapid heart rate, with hypotension, shock, and jaundice developing in some patients. Bacteremia often causes ecthyma gangrenosum, which are painless nodular skin lesions with ulceration and haemorrhage most often found in the armpit, groin, or perianal area [3,4].
Endocarditis
P. aeruginosa can infect both native heart valves and prosthetic heart valves. General symptoms include fever, murmur, and malaise, while more specific symptoms depends upon which valve is involved. Peripheral lesions and hemorrhages and an enlarged spleen can occur in addition to these specific symptoms.
Diagnosis
A complete blood count (CBC) is often performed to look for a rise in white blood cell count with a shift towards more immature leukocytes circulating in the blood. Blood cultures are often performed as well, both aerobic and anaerobic, to look for bacteremia. If endocarditis is suspected, echocardiography should be considered to verify diagnosis. UTIs are most often diagnosed through urinalysis and possibly a urine culture. Sputum and respiratory secretions are cultured in the diagnosis of pneumonia, but more accurate quantitative cultures are being performed more often to get a more accurate picture of the potential Pseudomonas infection. Blood gas analysis and chest radiography are also performed in cases of pneumonia. Wound and burn cultures in addition to cultures from other body fluids are important in accurate diagnosis and understanding of the scope of the infection. A bacterial count of greater than 100,000 organisms per gram of tissue is diagnostic of burn wound infection. If meningitis is suspected, a Gram stain and culture of cerebrospinal fluid should be performed, and in cases of suspected brain abscess, a CT scan or MRI is most often used. A triple-phase bone scan or MRI should be used to diagnose a suspected skeletal infection. Fluorescein staining and slit-lamp examination of the cornea is used to diagnose infections of the eye.
Treatment
Across the board, antimicrobials are the first choice in combatting P. aeruginosa infection. Often a two-drug therapy is used. Sometimes, steroids are used in conjunction with these antibiotics. The specific drugs used often depends on the site of the infection and, therefore, their ability to reach the site of infection in the highest percentages possible. Sometimes, surgery is required, such as in the case of malignant otitis or retinal detachment due to eye infection. Infections of the eye are treated depending upon severity, but antibiotics are always used in some form to manage the infection. Hydration is important in addition to antibiotics in GI infections. Addressing susceptibility patterns, especially in burn centers where Pseudomonas may be harbored, is important to detect multiple drug resistant strains. Surgical debridement of necrotic tissue is necessary to treat soft tissue infections as well. [3]
Prevention
Preventing transmission through medical equipment like catheters is an important way to prevent Pseudomonas infections. Aseptic techniques and sterile environments are important to prevent the spread of P. aeruginosa. Proper hygiene regarding medical devices like catheters is important to prevent opportunistic infection in a patient as well. Prophylactic use of antibiotics is not recommended to prevent the evolution of antibiotic-resistant strains of bacteria. Severe burn victims should be put into strict isolation to prevent unnecessary contact with potential pathogens. Care should be taken to seek help when there might be potential infection, such as with corneal scratches due to contact lenses.
Host Immune Response
P. aeruginosa are susceptible to the immune system when granulocytes are introduced into serum, which which alone, P. aeruginosa are resistant to. Pseudomonal cells are most efficiently killed when opsonizing antibodies that are directed primarily at the antigenic determinants of LPS are present. Phagocytosis is crucial to defense from P. aeruginosa infections. Once estabilished, antitoxins are important in controlling the disease. Since Pseudomonas infections are most often seen in those with compromised immune systems, which can be due to a variety of factors, it is obvious that the humoral immune response is crucial in both preventing and controlling infection. The exception to this is seen in patients with cystic fibrosis, who circulate high levels of antibodies, but are unable to clear P. aeruginosa from their lungs.
References
1. Textbook of Bacteriology. Todar's Online Textbook of Bacteriology.
2. Pollack M. Pseudomonas Aeruginosa. In: Mandell GL, Bennett JE, Dolin R, eds. Principles and Practice of Infectious Diseases. 5th ed. New York, NY: Churchill Livingstone; 2000:2310-27.
3. Medscape. "Pseudomonas aeruginosa Infections." http://emedicine.medscape.com/article/226748-overview
4. Hauser, A. "Pseudomonas aeruginosa". Nature. http://www.nature.com/nrmicro/posters/pseudomonas/posters.pdf
Created by Lillian Flannigan, student of Tyrrell Conway at the University of Oklahoma.
