Reptile-Exotic-Pet-Associated-Salmonellosis: Difference between revisions
No edit summary |
No edit summary |
||
| Line 40: | Line 40: | ||
==Epidemiology== | ==Epidemiology== | ||
===Transmission of Salmonella=== | ===Transmission of Salmonella=== | ||
<br>The main pathway of transmission for <i>Salmonella</i> spp. is via the fecal-oral route usually beginning with the ingestion of contaminated food or water so that the bacterium can reach the intestinal epithelium, spreading throughout the gastrointestinal tract causing gastroenteritis. Humans typically acquire the organisms through direct transmission through handling of a reptile, and via indirect transmission by contact with an object contaminated by a reptile. Other sources of transmission include aquariums, terrariums, cages, as well as the water that most reptiles like turtles and amphibians live in. Clothing that has come into direct contact with reptiles has been associated as a source of transmission, and also bites and claw scratches have been shown to be effective at transmitting <i>Salmonella</i> spp. | |||
<br><i>Salmonella</i> has been shown to be able to survive for long periods of time in the environment and especially in those environments where it is wet and warm, and has been isolated for prolonged periods from surfaces contaminated by reptile feces (Centers for Disease Control, Jan 2013). It is of important note to highlight the fact that the CDC found that <i>Salmonella</i> has been reported to “survive 89 days in tap water, 115 days in pond water, within dried reptile feces from cages 6 months after removal of the reptile, and from aquarium water 6 weeks after removal of a turtle (CDC, Jan 2013). These findinds alone show the danger associated with such a long living organism and help demonstrate the prevalence of the disease Salmonellosis and the dangers associated with <i>Salmonella</i> as a world-wide issue. | |||
===Pathology and Immune Response=== | ===Pathology and Immune Response=== | ||
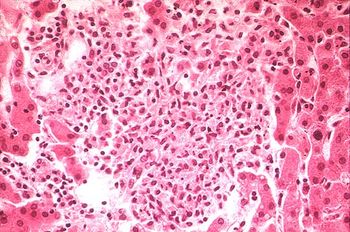
[[Image:yellow_salmonella.JPG|thumb|300px|right|''Salmonella typhimurium'' (red) invading cultured human cells. From [http://www2.niaid.nih.gov/biodefense/public/images.htm Rocky Mountain Laboratories, NIAID, NIH.]]] | [[Image:yellow_salmonella.JPG|thumb|300px|right|''Salmonella typhimurium'' (red) invading cultured human cells. From [http://www2.niaid.nih.gov/biodefense/public/images.htm Rocky Mountain Laboratories, NIAID, NIH.]]] | ||
Revision as of 00:01, 19 April 2015
By Tomas Grant
Introduction
Introduce the topic of your paper. What microorganisms are of interest? Habitat? Applications for medicine and/or environment?
Salmonella spp. are rod-shaped, flagellated, and facultative anaerobic bacteria which belong to the family Enterobacteriaceae, and as apart of the phylum Proteobacteria are Gram-negative. The genus Salmonella consists of two species S. enterica and S. bongori , the majority of the diversity lies within the more than 2,600 servovars of the species S. enterica . The three main servers within this species are (1) S. typhi, the cause of systemic infections and typhoid fever, (2) S. Enteritidis, a major food cause of food poisoning associated with poultry farming, and (3) S. typhimurium, which is not fatal in humans, but may cause gastroenteritis, but also more serious cases including septicemia, meningitis, and subnormal empyema. (Rabsch et, al, “The Zoonotic agent Salmonellosis).
Salmonellosis is one of the most common foodbourne diseases and can be caused by the various serovars of the species S. enterica , and is found worldwide, causing 93.8 million cases of gastroenteritis and over 155,00 deaths annually worldwide (Noellie et el 2014). Understanding the pathology of foodbourne Salmonellosis is important however, there is an increasing concern for Reptile-Exotic-Pet-Associated-Salmonellosis (REPAS ), in which Salmonella serovars act as major zoonotic agents of infection through direct or indirect animal contact in people’s homes, veterinary clinics, farms, zoological gardens, and other professional, public and private settings. (Rabsch et, al, “The Zoonotic agent Salmonellosis) . There are a number of reports that describe the prevalence of Salmonella spp. in reptiles ranging from lizards, snakes, and turtles, and multiple serovars have been identified and shown to be associated with each of these organisms (Sylvester et al, 2014). Reptiles have been shown to be asymptomatic carriers of Salmonella and have been shown to have a natural interaction with the bacteria, with these bacteria being natural inhabitants of reptile gut microflora, shredded at various rates throughout the reptile’s lifecycle. (INSERT) Figure showing prevalence of Salmonella by Species
At right is a sample image insertion. It works for any image uploaded anywhere to MicrobeWiki. The insertion code consists of:
Double brackets: [[
Filename: PHIL_1181_lores.jpg
Thumbnail status: |thumb|
Pixel size: |300px|
Placement on page: |right|
Legend/credit: Electron micrograph of the Ebola Zaire virus. This was the first photo ever taken of the virus, on 10/13/1976. By Dr. F.A. Murphy, now at U.C. Davis, then at the CDC.
Closed double brackets: ]]
Other examples:
Bold
Italic
Subscript: H2O
Superscript: Fe3+
Classification
Higher order taxa:
Kingdom:Bacteria
Phylum: Proteobacteria
Order: Gammaproteobacteria
Suborder: Enterobacteriales
Family: Enterobacteriaceae
Genus: Salmonella
Species:
Salmonella enterica subsp. I serovar Typhimurium (S. typhimurium LT2), S. enterica subsp. enterica serovar Typhi (S. typhi CT18), S. enterica subsp. enterica serovar Typhi Ty2 (S. typhi Ty2)
NCBI: Taxonomy Genome: S. typhi CT18 S. typhi Ty2 S. typhimurium|}
Epidemiology
Transmission of Salmonella
The main pathway of transmission for Salmonella spp. is via the fecal-oral route usually beginning with the ingestion of contaminated food or water so that the bacterium can reach the intestinal epithelium, spreading throughout the gastrointestinal tract causing gastroenteritis. Humans typically acquire the organisms through direct transmission through handling of a reptile, and via indirect transmission by contact with an object contaminated by a reptile. Other sources of transmission include aquariums, terrariums, cages, as well as the water that most reptiles like turtles and amphibians live in. Clothing that has come into direct contact with reptiles has been associated as a source of transmission, and also bites and claw scratches have been shown to be effective at transmitting Salmonella spp.
Salmonella has been shown to be able to survive for long periods of time in the environment and especially in those environments where it is wet and warm, and has been isolated for prolonged periods from surfaces contaminated by reptile feces (Centers for Disease Control, Jan 2013). It is of important note to highlight the fact that the CDC found that Salmonella has been reported to “survive 89 days in tap water, 115 days in pond water, within dried reptile feces from cages 6 months after removal of the reptile, and from aquarium water 6 weeks after removal of a turtle (CDC, Jan 2013). These findinds alone show the danger associated with such a long living organism and help demonstrate the prevalence of the disease Salmonellosis and the dangers associated with Salmonella as a world-wide issue.
Pathology and Immune Response

Include some current research, with at least one figure showing data.
Risks Associated With S. enterica infections
Diversity of Serovars
Antibiotic Resistance and Health Risks
Include some current research, with at least one figure showing data.
Disease Prevention Measures
Include some current research, with at least one figure showing data.
References
[1] Fàbrega, Anna, and Jordi Vila. "Salmonella Enterica Serovar Typhimurium Skills to Succeed in the Host: Virulence and Regulation." Clinical microbiology reviews 26.2 (2013): 308-41.
Authored for BIOL 238 Microbiology, taught by Joan Slonczewski, 2015, Kenyon College.
