Neisseria meningitidis: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
{{Biorealm Genus}} | {{Biorealm Genus}} | ||
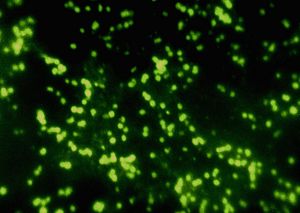
[[Image:neisseria.jpg|thumb|right| | [[Image:neisseria.jpg|thumb|right|300x|''Neisseria meningitidis'' group C, in spinal fluid. From [http://pathmicro.med.sc.edu/fox/spiro-neisseria.htm, CDC/Dr. M.S. Mitchell, University of South Carolina School of Medicine.]]] | ||
==Classification== | ==Classification== | ||
Revision as of 01:31, 15 June 2007
A Microbial Biorealm page on the genus Neisseria meningitidis
Classification
Higher Order Taxa
Bacteria; Proteobacteria;Betaproteobacteria; Neisseriales; Neisseriaceae; Neisseria.
Genus
Neisseria Meningitidis
|
NCBI: Taxonomy |
Description and Significance
Neisseria meningitidis is a parasitic, aerobic, Gram-negative, non endospore forming, nonmotile (although piliated) , coccal bacterium that is responsible for causing meningitis, inflammation of the meninges layer covering the brain. Because it is an aerobic organism, like most members of the Neisseriaceae family, it also has catalase and oxidase activity. Colonies appear smooth, moist, and glistening (Rake). N. meningitidis resides primarily in humans on the surface of mucosal membranes such as those found in the respiratory tract. Progression through meningitis almost always follows after entering the blood stream. (See Pathology below) Symptoms of this disease was first noted in 1805, having been described as an epidemic cerebrospinal fever (Vieusseaux) but it was not isolated until 1887 by Weichselbaum (Weichselbaum). In the U.S., every year, there are approximately 3000 to 4000 cases of N. meningitidis linked meningitis (Wong et al). Because this bacterium poses a health threat, genome sequencing has already begun for a few of these strains to enable deeper understanding of its mechanism of infection. This also provides for studies towards dealing with antibiotic resistant strains.
Genome Structure
Of the 13 N. meningitidis serotypes, there are three that are sequenced – strain Z2491 from serotype A, MC58 from serotype B, and FAM18 from serotype C. All three serotypes have a single circular chromosome that is approximately 2.2 megabasepairs in size with a G C content of 51%. Z2491, serotype A, has a GC content of 51% with 2,184,406 nucleotides and 2208 genes of which 2049 encode protein, 72 encode structural RNA, and 87 are pseudo genes. The respective numbers for MC58, serotype B, are 51% GC content, 2,272,360 nucleotides, 2225 genes of which 2063 are for proteins, 71 for structural RNA, and 91 are pseudo genes. Lastly, FAM18, serotype C has a GC content of 51%, 2,194,961 nucleotides in length including 2046 genes of which 1917 are protein coding, 71 are structural RNA coding, and 58 are pseudo genes. (8,9,10). In contribution to its pathogenicity, a highly variable type IV pilus is encoded by 8 silent copies of the pilin gene. Pili serve multiple purposes including surface adhesion, genetic transformation, and motility. Serotype B also encodes an FtsE protein, an ATP binding protein involved in cell division that’s analogous to FtsZ in Bacillus subtilis. So far, there is one plasmid sequenced for this species, the pJS-B plasmid that encodes seven “hypothetical proteins” whose functions are still unknown (11).
Cell Structure and Metabolism
Neisseria meningitidis, like most other members of the Neisseriaceae family are aerobic organisms with catalase and oxidase activity. One interesting observation made by Duong and Archibald was that in both N. gonorrhoeae and N. meningitidis, the superoxide dismutase (SOD) enzyme was not present. As a compensation for oxidative damage in a low pressure oxygen environment, N. gonorrhoeae’s natural environment, catalase activity was notably high in addition to high glutathione content (Archibald).
In terms of metabolism, N. meningitidis requires mineral salts, lactate, some amino acids such as cysteine, and glutamic acid as a carbon source (Catlin). In 2004, knock out experiments of the gdhA gene which encodes glutamate dehydrogenase in N. meningitidis, confirmed the importance of glutamic acid metabolism towards growth and virulence. In addition to organic nutrient requirements, iron is also needed as an electron acceptor as demonstrated by the increase in generation times during iron restriction (Archibald and DeVoe). In a human host, this iron is supplied from heme iron in the blood where active transport is mediated a TonB dependent receptor.
Ecology
As mentioned in the previous section, iron reduction is a necessary part of N. meningitidis metabolism. Humans are its primary reservoir from which heme iron, along with other nutrients in the blood, satisfies its requirement for growth. The result of this is an aggregation of blood cells – clumping, a sign of infection. Although not always, it has been shown by Lappann et al that N. meningitidis is capable of forming biofilm communities in a slow flow environment (see Current Research below).
Pathology
Neisseria meningitidis is often transferred from person to person in aerosol form as from a sneeze. Upon infection, it first takes residence on the muscosal membrane surface as in the nose, throat, and respiratory tract by attaching with its pili. It then gradually infects deeper into the tissue until it gains access to the bloodstream where it then travels to infect the meninges of the brain. Three primary characteristics make N. meningitidis an evasive bacterium to the immune system. Of the 13 serotypes, type A, B, C, Y, and W135 (Neisseria meningitidis NCBI Entrez Genome Project) produce an antiphagocytic capsular polysaccharide, a coat that contains highly variable surface proteins thus contributing to its evasiveness. In addition, as mentioned earlier, the pilus coding genes are also highly variable contributing to its pathogenicity. Lastly, N. meningitidis produces large amounts of the endotoxin lipopolysaccharide (LPS) especially during the exponential growth phase which is excreted after blebbing (DeVoe). Naturally, people with a weakened immune system or are immunosuppressed are at greater mortality risk which is why most victims are children.
Applications to Biotechnology
There are no compounds produced by N. meningitidis that are used for biotechnology.
Current Research
Regulation and differential expression of gdhA encoding NADP-specific glutamate dehydrogenase in Neisseria meningitidis clinical isolates.
In this article, a direct association was found between the virulence of meningococcal on infant rats with the degree of glutamate dehydrogenase expression. Glutamate dehydrogenase converts glutamate to alpha-ketoglutarate, an intermediate in the TCA cycle. The degree of expression is dictated by the number of active copies of the gdhA gene. On a wildtype strain, there are two copies, gdhA P1 and gdhA P2. P2’s activity is regulated by a positive regulatory ligand (activator) gdhR as demonstrated through complementation experiments where gdhR knockouts failed to grow on glucose media. In the presence of glucose, NADP linked GDH levels increase and enhances growth by facilitating nitrogen metabolism. In the mice infected with different mutants, it was found that the most virulent strains were those with both copies active followed by one copy followed by no copy.
Type IV pilus retraction in pathogenic Neisseria is regulated by the PilC proteins. Type IV pili synthesis is regulated by PilC proteins that are integrated in the outer membrane. Mutant strains for PilC failed to properly synthesize pili. In addition, pili are also capable of retraction which is mediated by the PilT nucleotide-binding protein. It is this retraction that gives N. meningitidis its twitching motility. The process involves translocation of the PilT protein to the cytosolic side of the membrane. Researchers are currently engineering meningococcal strains for use as a tool to study PilC and PilT protein role in pili synthesis and retraction. Pili are used by bacteria in a variety of different ways such as for adhesion to a surface and conjugal DNA transformation, in addition to motility.
Meningococcal biofilm formation: structure, development, and phenotypes in standardized continuous flow system. This article showed that noncapsulated meningococcus were able to form biofilms much like gonococcus, Salmonella and Escherichia coli. Biofilms provides resistance against antibiotics such as penicillin. With penicillin, a transpeptidase inhibitor, it is not so much that the biofilm provides the protection but that N. meningitidis is a Gram-negative cell which has little cell wall, if any, for the antibiotic to act on. It was also noted that within the biofilm growth, microcolonies were formed, made possible by the pilE gene product pilus subunits. However, the contrary is not true in that biofilim formation was not dependent on pili. Moreover, it was shown that pili formation was not for the sole purpose of forming microcolonies. PilX, a type IV pilus protein plays an important role in forming aggregates similar to what happens to the erythrocytes of a host. Lastly, what’s interesting is why a capsule is maintained across the genus even though biofilms can be formed. It is speculated that capsule formation is maintained as a transient vessel when the bacterium is relocated in a different niche outside of the biofilm community. A capsule would provide protection from desiccation.
References
(1.) [Archibald, Frederick S. and Minh-Ngoc Duong. "Superoxide Dismutase and Oxygen Toxicity Defenses in Genus Neisseria." Infection and Immunity FEB 1986 631-641. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=262393]
(2.) [Archibald, Frederick S. and I.W. DeVoe “Iron in Neisseria meningitidis: Minimum Requirements, Effects of Limitation, and Characteristics of Uptake.” Journal of Bacteriology OCT 1978 35-48. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=218629]
(3.) [Catlin, B.W. Nutritional profiles of N. gonorrhoeae, N. meningitidis, and N. lactamica in chemically defined media and the use of growth requirement of gonococcal typing. Journal of Infectious Disease 1973. 28; 178-194.]
(4.) [DeVoe, I. W. “The Meningococcus and Mechanisms of Pathogenicity.” Microbiological Reviews JUNE 1982. Pp.162-190 http://mmbr.asm.org/cgi/reprint/46/2/162?view=long&pmid=6126800]
(5.) [Lappann, Marin, Janus A >J. Haagensen, Heike Claus, Ulrich Vogel, Søren Molin. “Meningococcal biofilm formation: structure, development, and phenotypes in a standardized continuous flow system” Molecular Microbiology 13 OCT 2006. 62 (5) 1292-1309 http://www.blackwell-synergy.com/doi/abs/10.1111/j.1365-2958.2006.05448.x]
(6.) [Morand, Philippe C., Emmanuelle Bille, Sandrine Morelle, Emmanuel Eugène, Jean-Luc Beretti, Mathew Wlfgang, Thomas F. Meyer, Michael Koomey, Xavier Nassif. “Type IV pilus retraction in pathogenic Neisseria is regulated by the PilC proteins.” The EMBO Journal 22 APR 2004 23, 2009-2017. http://www.nature.com/emboj/journal/v23/n9/abs/7600200a.html]
(7.) [NCBI Entrez Genome Project. “Neisseria meningitidis Z2491 prject at Sanger Institute” http://www.ncbi.nlm.nih.gov/sites/entrez?db=genomeprj&cmd=search&term=txid65699%5Borgn%5D Last Accessed: June 02, 2007]
(8.) [NCBI Entrez Genome Sequence. “Neisseria meningitidis Z2491 complete genome” http://www.ncbi.nlm.nih.gov/sites/entrez?Db=Genome&Cmd=ShowDetailView&TermToSearch=156 ]
(9.) [NCBI Entrez Genome Sequence. “Neisseria meningitidis MC58 complete genome” http://www.ncbi.nlm.nih.gov/sites/entrez?Db=Genome&Cmd=ShowDetailView&TermToSearch=155 ]
(10.) [NCBI Entrez Genome Sequence. “Neisseria meningitidis FAM18 complete genome” http://www.ncbi.nlm.nih.gov/sites/entrez?Db=Genome&Cmd=ShowDetailView&TermToSearch=20258 ]
(11.) [NCBI Entrez Genome Sequence. “Neisseria meningitidis pJS-B complete sequence” http://www.ncbi.nlm.nih.gov/sites/entrez?Db=genome&Cmd=ShowDetailView&TermToSearch=17045 ]
(12.) [Pagliarulo, Caterina, Paola Salvatore, Lucia Rosaria De Vitis, Roberta Colicchio, and Caterina Monaco. "Regulation and differential expression of gdhA encoding NADP-specific glutamate dehydrogenase in Neisseria meningitidis clinical isolates." Molecular Biology 17 NOV 2003 1757-1772. http://www.blackwell-synergy.com/links/doi/10.1111/j.1365-2958.2003.03947.x/abs/]
(13.) [Rake, G. “Studies on meningococcus infection. I. Biological properties of “Fresh” and “Stock” strains of meningococcus.” Journal of Experimental Medicine. 1933 57; 549-559]
(14.) [Vieusseaux M: Mémoire sur le maladie qui a regne a Génève au printemps de 1805. Journal de Médecine, Chimie, et Pharmacologie 1805. 11;163]
(15.) [Weichselbaum A: Ueber die aetiologie der akuten meningitis cerebrospinalis. Fortschr Med 1887; 5:573-583.]
Edited by Steven Chou, Student of Rachel Larsen at UCSD.
