African Trypanosomiasis: Difference between revisions
| Line 13: | Line 13: | ||
===Epidemiology=== | ===Epidemiology=== | ||
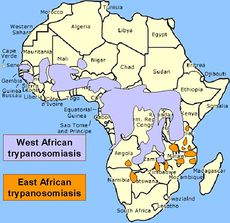
[[Image:epidemiology.jpg|230px|thumb|left|Geographical distribution of the two forms of Human African Trypanosomiasis. From: legacy.earlham.edu [http://legacy.earlham.edu/~harrico/Trypanosite2.htm]]] | [[Image:epidemiology.jpg|230px|thumb|left|Geographical distribution of the two forms of Human African Trypanosomiasis. From: legacy.earlham.edu [http://legacy.earlham.edu/~harrico/Trypanosite2.htm]]] | ||
Sleeping Sickness is limited to sub-Saharan Africa in its epidemiology. The two subspecies of the parasite which causes African Trypanosomiasis <i>rhodiense</i> and <i>gambiense</i> are geographically separate from each other. <br><br> | |||
The <i>rhodiense</i>-caused infection, often called East African Trypanosomiasis is present in specific areas within eastern and southern Africa. Countries with the highest prevalence of this form of the disease include Malawi, Zambia, Uganda, and Tanzania. <br><br> | |||
The <i>gambiense</i>-caused infection, which accounts for the vast majority of sleeping sickness cases, is also called West African Trypanosomiasis. The disease is found predominately in central and western African countries, most commonly in the Democratic Republic of Congo, Angola, Sudan, Chad, and the Central African Republic.<br><br> | |||
The disease very rarely occurs in any places outside of sub-Saharan Africa, and of those cases almost all occurred in people who had either recently traveled to areas in which the disease is endemic or recently immigrated from areas in which the disease is endemic. | |||
===Virulence Factors=== | ===Virulence Factors=== | ||
Revision as of 14:25, 23 July 2014
[3]]]

Etiology
Taxonomy
| Domain = Protozoa | Phylum = Sarcomastigophora | Class = Zoomastigophora | Order = Kinetplastida | Family = Trypanosomatidae | Genus = Trypanosoma | Species = T. brucei
|NCBI: Taxonomy Genome: Genome|}
Description
African Trypanosomiasis also called Sleeping Sickness is caused by Trypanosoma brucei, a unicellular parasitic protozoan. There are two separate subspecies which cause sleeping sickness in humans, Trypanosoma brucei gambiense which accounts for around 98% of cases and Trypanosoma brucei rhodesiense which accounts for the remaining 2% of cases. African trypanosomiasis is limited in epidemiology to areas of Sub-Saharan Africa. Trypanosoma brucei was first described as the causative agent of Sleeping Sickness in 1901. Although by the mid-1960s the disease had been largely eliminated, the disease saw a reemergence countries in which the disease was endemic gained independence and their health systems subsequently collapsed. The protozoan is spread via the tsetse fly, and key symptoms of the disease include headache, fever, stiffness and later coma and death.
Pathogenesis
Transmission
Infectious Dose, Incubation, and Colonization
Epidemiology
Sleeping Sickness is limited to sub-Saharan Africa in its epidemiology. The two subspecies of the parasite which causes African Trypanosomiasis rhodiense and gambiense are geographically separate from each other.
The rhodiense-caused infection, often called East African Trypanosomiasis is present in specific areas within eastern and southern Africa. Countries with the highest prevalence of this form of the disease include Malawi, Zambia, Uganda, and Tanzania.
The gambiense-caused infection, which accounts for the vast majority of sleeping sickness cases, is also called West African Trypanosomiasis. The disease is found predominately in central and western African countries, most commonly in the Democratic Republic of Congo, Angola, Sudan, Chad, and the Central African Republic.
The disease very rarely occurs in any places outside of sub-Saharan Africa, and of those cases almost all occurred in people who had either recently traveled to areas in which the disease is endemic or recently immigrated from areas in which the disease is endemic.
Virulence Factors
Clinical Features
Symptoms
Sleeping sickness is characterized by two different stages. The beginning stage of the disease occurs while the parasite is still located only in the peripheral circulation. The disease progresses into the second stage when the parasite crosses the blood-brain barrier, infecting the central nervous system. Both of the subspecies which cause African Trypanosomiasis have different progressions and symptoms but ultimately if left untreated both result in coma followed by death.
Trypanosoma brucei rhodiense which causes close to just 2% of all human sleeping sickness cases is characterized by rapid progression. The most common symptoms include headache, fever, joint aches and stiffness, and enlarged lymph nodes. Patients may also develop a large sore at the site of the tsetse fly bite. All of these symptoms usually appear within one to two weeks following infection with the parasite. It takes only several weeks for the parasite to cross the blood-brain barrier and infect the central nervous system. After infection by this subspecies, if left untreated, death typically occurs in just several months.
By comparison progression of sleeping sickness caused by the gambiense subspecies is much slower and initial symptoms of the disease are similar to that caused by the rhodiense subspecies but much milder. Weight loss and general fatigue are also common symptoms associated with infection by this subspecies. With this infection it typically takes somewhere between one and two years for the parasite to cross the blood-brain barrier, however it may take longer. When untreated death occurs most often within six years and infection rarely lasts longer than six to seven years.
Several characteristic symptoms occur when the parasite (either subspecies) crosses the blood-brain barrier and infects the central nervous system. The sleep cycle is almost always disturbed, with patients experiencing daytime sleepiness and issues sleeping during the night. Personality changes and confusion are also apparent once the infection reaches the CNS. Furthermore patients may experience partial paralysis and difficulties with balance.

