Campylobacter in United States
Introduction
Campylobacteriosis occurs as a result of an infection by the spiral-shaped bacteria Campylobacter. It causes a variety of symptoms like diarrhea, cramps, and fevers. Campylobacteriosis usually does not lead to mortality, but it can lead to complications like Gullian-Barré Syndrome which involves neural damage and arthritis. In the United States, antibiotics have been used in poultry, one of the major ways the disease is spread, in an attempt to kill the bacteria, but this has led to a problem of antibiotic resistant Campylobacter. Thus, government agencies in the U.S. have released guidelines such as teaching people to safely handle food to reduce Campylobacter infections.
Description of Campylobacteriosis
Campylobacteriosis is a common infectious disease found in the United States. It is a main cause of diarrheal illness shown by the numerous records of human gastrointestinal infection (17,5). The major clinical manifestations of campylobacteriosis consist of bloody diarrhea, cramping, abdominal pain, and fever that lasts for three to seven days (4). In some cases, campylobacteriosis may lead to arthritis, Gullain-Barre Syndrome, or even mortality as indicated by observations of 124 deaths in a year in the United States (1,3).
Description of the Microbe
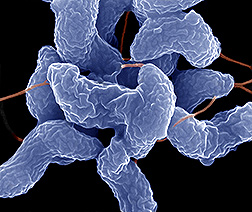
See Campylobacter.
Cell Structure:
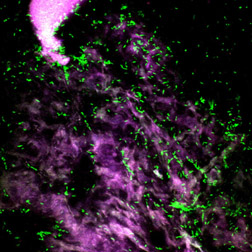
Campylobacter is a spiral-shaped bacteria that grows best at the body temperature similar to that of birds, which carry this bacteria without being infected itself. These bacteria are extremely delicate and can be killed by oxygen since they only thrive in areas with less oxygen (6). Campylobacter pathogenesis is mediated by flagellar adhesins or outer bacterial membrane components as well as toxins (7). There are several bacterial factors that have been pointed to as the cause for the disease:

- Capsule: Many bacteria have capsular polysaccharides and they play a large role in survival and often contribute to pathogenesis. Campylobacter's capsule helps it with epithelial invasion and adherence and causing diarrhoeal disease. On top of playing a vital role in adhesion to the epithelial cells, the capsule also helps to provide protection against host antimicrobial shields (10). The capsule also has lipoolidosaccahriades (LOS) that help the bacteria avoid the immune system through molecular mimicry of human neuronal gangliosides, thought to lead to autoimmune disorders that may cause paralytic neuropathy in 1 in every 1000 cases of campylobacterosis (8).
- Flagellin: Campylobacter uses its flagella for motility and for invasion (9). It is highly mobile, able to overcome peristalsis, as well as enter the mucous layer. It contains a single unsheathed flagella at one or both poles. Other than for the purpose of motility, Campylobacter also uses its flagella to excrete proteins that help it adhere and invade the host (10).
- Cytolethal Distending Toxin: Cytolethal distending toxin (CDT) maybe be important for the regulation of cell cycle as well as an inductor of host cell death and is the only toxin that Campylobacter has (9). CDT prevents host cells from entering mitosis and leads them to death. This toxin consists of three proteins that are membrane associated and contribute to inflammatory responses (10).
- Glycosylation: Campylobacter modifies its flagella post-translationally. N-linked glycosylation of more than 30 proteins helps the bacterium adhere and invade the human epithelia. O-linked glycosylation is vital to proper flagellin assembly and motility (10).
- Adherence factors: Though Campylobacter does not have adherence organelles, there are several proteins that contribute to adherence to human epithelial cells. CadF is a protein that helps Campylobacter bind and inavde. JlpA is an adhesin lipoprotein on the surface that contributes to inflammation (8).
Genome:
The genome of Campylobacter is the most recent and first food-borne pathogen to be sequenced in 2000 by the Sanger Institution. The exact order of the 1.64 million bases that make up the pathogen's genetic code has been determined by researchers at the Sanger Centre in Cambridge, U.K. It was also discovered by the Sanger group that repeated sequences of either guanine or cytosine bases might have allowed this bacterium to evolve in order to shield itself from being recognized by the host immune system, which is crucial information to help researchers develop vaccines to protect against this pathogen. These repeated sequences lead to mutations, which lead to changes to the structure and function of the gene's protein. Such mutagenic changes primarily target genes involved in the production of lipopolysacharides, sugars which coat the surface of the Campylobacter (11). These mutations primarily affect genes that help produce lipopolysacharides, the sugars that coat the surface of Campylobacter. By frequently altering these genes, Campylobacter may change how its surface looks to the immune system and may thus avoid recognition by antibodies made during previous infections (11, 21).
Transmission of Disease
Campylobacteriosis is caused by a bacteria from the genus Campylobacter, such as Campylobacter jejuni. Usually people contract this disease by ingesting contaminated food such as undercooked poultry or by coming in contact with the stool of an infected animal (1). Although this disease occurs in single, sporadic cases, outbreaks can also occur by consuming unpasteurized milk or contaminated water (2). In a study found by Keith, statistics have been found that rural areas, where there is a high consumption of raw milk, have infection rates that are five to six times higher than other areas (1).
Prevention
See #What is being done to improve the situation?
A Problem in the United States
In the United States, about 2 million people are infected by Campylobacter each year (1). Of the people infected in the United States, young men and infants have the highest campylobacteriosis isolation rates. It is thought that young men have a high isolation rate, because they handle food poorly as they learn to prepare their own meals independently for the first times (12,14). Researchers believe that infants have a high incidence rate, because they are highly susceptilbe to infection upon their first exposures to the bacteria and that only a small number of parents seek medical care for their infants upon infection (12). Campylobacteriosis is a problem in the United States, because it leads people to suffer from symptoms like diarrhea, fever, and abdominal cramps. While many people do not require antibiotic treatment, some people, like those experiencing high fever or those with weakened immune systems, need antibiotics like erythromycin (12). However, using antibiotics in treating humans and farm animals has led to the problem of antibiotic resistance. One of the most common ways in which people become infected with Campylobacter and then develop campylobacteriosis is by consuming poultry that contains the bacteria. Thus, as a preventative measure, antibiotics like fluroquinolone were injected into poultry to kill the bacteria (13). But, in a study mentioned by Altekruse et al., 20% of the Campylobacter bacteria recovered from chicken in the supermarket were resistant to antibiotics like ciprofloxacin (12). This poses the challenge of finding new ways to treat people with campylobacteriosis if the antibiotics we use today are losing their effectiveness. Thus, it is important to find ways to effectively treat Campylobacter infections.
Solution and Prevention to Campylobacter Infection
There is no specific treatment to Campylobacter infection. However, if a person is suffering from diarrhea, nausea, or cramps, they should drink extra fluids and see a doctor immediately (6).
One way to prevent campylobacteriosis is by having a series of infection control measures on all stages of food processing. A report from CDC points out that, "Universal pasteurization of milk and proper treatment of all drinking water might prevent 80 percent of the U.S. outbreaks due to Campylobacter" (15). The report shows that sanitation and avoidance of eating raw foods could minimize the chance of Campylobacter infections (16). On the other hand, the Food Safety and Inspection Service of the United States had enforced “a combination of Hazard Analysis and Critical Control Points of microbial testing, pathogen reduction performance standards, and sanitation operation” from agricultural production to processing of foods since 1998. FSIS also has a safe food handing education program to teach people how to prevent and reduce Campylobacter infections (17). However, a study from the University of Maryland had randomly made 719 samples of retail raw meats from Washington D.C area to test for campylobacter. The study found out that “70.7% of chicken sample” and “14% of turkey samples yielded Campylobacter”. The study suggests that a more hazard analysis of critical control point and safety education have to be implemented to effectively prevent Campylobacter (22).
What is being done to improve the situation?
In 1995 the FDA approved the use of fluoroquinoles in poultry to reduce the prevalence of the Campylobacter bacteria amongst the flocks (18). Fluoroquinoles are a group of antimicrobials that target gram negative bacteria like Campylobacter (19). However, this caused a rise in the levels of Campylobacter bacteria that showed antimicrobial-resistance (20). To avoid further rise in resistant strains of Campylobacter, the FDA removed the approval on the use of Fluoroquinoles on this bacteria in 2005 (18). This suggests that more research on the bacteria must be done to understand the nature of the pathogen before antimicrobials are used to treat the disease. In order to ultimately improve the situation, more of Campylobacter's virulence factors need to be known to treat the disease on a microbial level.
References
1. Keith, Jolley. "The Campylobacter jejuni Multi Locus sequence Typing website." Bioinformatics. 2004. Wellcome Trust. <http://pubmlst.org/campylobacter/>
2. CDC. Preliminary FoodNet data on the incidence of infection with pathogens transmitted commonly through food--10 states, 2006. MMWR Morb Mortal Wkly Rep. Apr 13 2007;56(14):336-9.
3. Allos BM. Campylobacter jejuni infection as a cause of the Guillain-Barre syndrome. Infect Dis Clin North Am. Mar 1998;12(1):173-84.
4. Helms M, Simonsen J, Molbak K. Foodborne bacterial infection and hospitalization: a registry-based study. Clin Infect Dis. Feb 15 2006;42(4):498-506
5. Ang, Jocelyn Y. "Camplyobacter Infections" Emedicine. Sep 7, 2007. WebMD. http://emedicine.medscape.com/article/970552-overview
6. Center of Disease Control and Prevention, “Campylobacter General Information”. May 21, 2008 <http://www.cdc.gov/nczved/dfbmd/disease_listing/campylobacter_gi.html#5>
7. Butzler, Jean-Paul, and Johannes Oosterom. "Campylobacter: pathogenicity and significance in foods." International Journal of Food Microbiology 12.1 (1991): 3.
8. Young, Kathryn T., Lindsay M. Davis, and Victor J. Dirita. "Campylobacter Jejuni: Molecular Biology and Pathogenesis." Nature Reviews 5 (2007): 667,671.
9. Dasti, Javid I., Malik A. Tareen, Raimond Lugert, Andreas E. Zautner, and Uwe Grob. "Campylobacter Jejuni: A Brief Overview On Pathogenicity-Associated Factors and Disease-Meditating Mechanisms." International Journal of Medical Microbiology (2009).
10.Zilbauer, Matthius, Nick Dorrell, Brendan W. Wren, and Mona Bajaj-Elliot. "Campylobacter Jejuni- Mediated Disease Pathogenesis." Transactions of the Royal Society of Tropical Medicine and Hygiene 102.2 (2008): 124-26.
11. Pennisi, Elizabeth. “Microbial Genetics: First Food-Borne Pathogen Sequenced.” Science Magazine 283. 5406 (1999): 1243. 20 August 2009 <http://www.sciencemag.org/cgi/content/full/sci;283/5406/1243?maxtoshow=&HITS=10&hits=10&RESULTFORMAT=&fulltext=Campylobacter+jejuni&searchid=1&FIRSTINDEX=0&resourcetype=HWCIT>.
12. Altekruse, Sean F., Norman J. Stern, Patricia I. Fields, and David L. Swerdlow. "Campylobacter jejuni-An Emerging Foodborne Pathogen." Emerging Infectious Diseases 5.1 (1999): 28-35. 13 August 2009 <http://www.cdc.gov/ncidod/EID/vol5no1/altekruse.htm>.
13. Engberg, Jorgen, Frank M. Aarestrup, Diane E. Taylor, Peter Gerner-Smidt, and Irving Nachamkin. "Quinolone and Macrolide Resistance in Campylobacter jejuni and C. coli: Resistance Mechanisms and Trends in Human Isolates." Emerging Infectious Diseaseshttp://www.cdc.gov/ncidod/EID/vol7no1/pdfs/engberg.pdf>. 7.1 (2001): 24-34. 18 August 2009 <
14. Friedman, Cindy R., Robert M. Hoekstra, Michael Samuel, Ruthanne Marcus, Jeffrey Bender, Beletshachew Shiferaw, Sudha Reddy, Shama Desai Ahuja, Debra L. Helfrick, Felicia Hardnett, Michael Carter, Bridget Anderson, and Robert V. Tauxe. "Risk Factors for Sporadic Campylobacter Infection in the United States: A Case-Control Study in FoodNet Sites." Clinical Infectious Diseases 38.3 (2004): S285-296. 13 August 2009 <http://www.journals.uchicago.edu/doi/abs/10.1086/381598>.
15. Campylobacter isolates in the United States, 1982- 1986," Centers for Disease Control, "Morbidity and Mortality Weekly Report," U.S. Department of Health and Human Services, Vol. 37, No. SS-22.
16. World Health Organize, “Campylobacter Fact Sheets”, Novemeber 2000. <http://www.who.int/mediacentre/factsheets/fs255/en/>
17. Food Safety and Inspection Services, United States Department of Agriculture, “Campylobacter Fact Sheets”, September 27, 2006 <http://www.fsis.usda.gov/factsheets/Campylobacter_Questions_and_Answers/index.asp#6>
18. Campylobacter Technical Information. 21 May 2008. Centers for Disease Control and Prevention. 24 August 2009 <http://www.cdc.gov/nczved/dfbmd/disease_listing/campylobacter_ti.html> .
19. Fluoroquinoles: Bacteria and Antibacterial Drugs: Merck Manual Professional. November 2005. Merck. 24 August 2009. <http://www.merck.com/mmpe/sec14/ch170/ch170f.html> .
20. Butzler, J.-P. "Campylobacter, from obscurity to celebrity" Clinical Microbiology & Infection Volume 10 (2004): Pages 868-876. Wiley Interscience. 24 August 2009. <http://www.ncbi.nlm.nih.gov/pubmed/15373879?ordinalpos=1&itool=EntrezSystem2.PEntrez.Pubmed.Pubmed_ResultsPanel.Pubmed_DiscoveryPanel.Pubmed_Discovery_RA&linkpos=4&log$=relatedreviews&logdbfrom=pubmed> .
21. Parkhill J, Wren BW, Mungall K, Ketley JM, Churcher C, Basham D, Chillingworth T, Davies RM, Feltwell T, Holroyd S, Jagels K, Karlyshev AV, Moule S, Pallen MJ, Penn CW, Quail MA, Rajandream MA, Rutherford KM, van Vliet AH, Whitehead S, Barrell BG. “The genome sequence of the food-borne pathogen Campylobacter jejuni reveals hypervariable sequences.” Nature 403 (2000): 665-668. 26 August 2009 < http://www.nature.com/nature/journal/v403/n6770/full/403665a0.html>.
22. Cuiwei Zhao, Beilei Ge, Juan De Villena, Robert Sudler, Emily Yeh,Shaohua Zhao, David G. White, David Wagner, and Jianghong Meng. “Prevalence of Campylobacter spp., Escherichia coli, and Salmonella serovars in retail chicken, turkey, pork, and beef from the Greater Washington, D.C., area.”. Applied Envrionment Microbiology, 67(12):5431-6, December 2001.
Edited by Stephanie Ng, Jia Liang, Hannah Yoo, Linda Truong, Connie Choi, Yuliya Guberer, students of Rachel Larsen
