Campylobacteriosis
Etiology/Bacteriology
Taxonomy
| Domain = Bacteria | Phylum = Proteobacteria | Class = Epsilon Proteobacteria | Order = Campylobacterales | Family = Campylobacteraceae | Genus = Campylobacter | Species = jejuni
Description
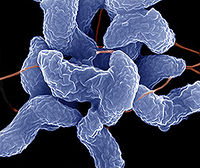
Camplobacteriosis, caused by Campylobacter jejuni in the human body, is the most common cause of diarrhea in the US. Campylobacter is a Gram-negative spiral bacterium which damages the small intestine and colon. This pathogenic bacteria causes bloody diarrhea, cramping, vomiting, abdominal pain, and fever. Campylobacter is microaerophilic as well as a thermophile and takes 2-5 days to begin showing symptoms. It is a self limiting bacteria that runs its course in 5-7 days. This non-spore forming prokaryote was isolated in 1972 and genome sequenced in 2000. Campylobacter usually occurs in isolated events affecting 1.3 million people a year. C. jejuni has a very low infectious dose of 500. It is a motile pathogen that causes disease by producing cytolethal distending toxin which stops the cell from dividing and activating the immune system. This helps C. jejuni to evade the small intestine and colon. Campylobacter is transmitted by raw or uncooked poultry, unpasteurized dairy, contaminated water, produce, and stool from animals or humans. It is rarely passed from human to human, but rather through consumption of infected food. Prevention is possible by simply cooking meat thoroughly, washing hands, and not using contaminated cooking utensils for uncooked goods. While some antibiotics such as Azithromycin are used to treat most abstain from medicine allowing the pathogen to run its course while replenishing the body with water and electrolytes. In rare incidents Camplobacter can cause longer term consequences such as arthritis, Guillian-Barre syndrome, and gastrointestinal perforation. C. jejuni is estimated to kill 76 people a year, mostly infants and children. To discover Camplobacter as the infectious agent fecal matter must be cultured.
Pathogenesis
Transmission
The main transmission route for Campylobacter is ingestion of contaminated food followed by consumption of contaminated waster then fecal-oral ingestion. Roughly 57% of cases can be traced to chicken and 35% to cattle. Animal farms as well as slaughter houses were found to have a high infestation of Campylobacter. Transmission can be found in cross-contamination of these farms and water supply as well as contamination in ones own kitchen. Unpasteurized milk has also proven to transmit Campylobacter through utter infection and contact with milk. Campylobacter is most common in developing countries causing 19% of diagnosed C. jejuni to be associated with international travel.
Infectious Dose, Incubation, Colonization
The infectious dose of C. jejuni is around 500 organisms. The incubation period for this organism is 1-11 days with the average being 2-5 days. C. jejuni typically colonizes the gall bladder and intestine.
Epidemiology
Campylobacter jejuni is the leading cause of bacterial diarrhea in the U.S. and is prevalent in other developed countries as well. The first reported outbreak of Campylobacteriosis was in 1978. The majority of campylobacteriosis cases are sporadic with only 3% being associated with households and 2.3% being in a cluster. Campylobacteriosis is often underreported so numbers of infected persons per year are often low. It is estimated that around 70% of poultry are infected with Campylobacter depending on the region. Children under 5 and young adults are the most likely to be infected by this pathogen. The incidence of disease has remained stable in the past few years.
Virulence Factors
Motility through flagellin
Chemotaxis which includes sensing the environment and rotating flagella accordingly to benefit the bacteria. Mucin has been found to be a positive chemotaxin for C. jejuni which is compatible with the bacteria’s colonization of the intestine where there is abundant mucus. This virulence factor would serve as a guide towards colonization for the bacteria. Bile and L-fucose are also positive chemotaxins for C. jejuni.
Invasion
Adhesion
Cell wall
Cytolethal distending toxin
Hemolysin
Superoxide dismutase for getting rid of the reactive oxygen species superoxide
Antibiotic resistance to tetracycline, erythromycin, ciprofloxacin, kanamycin, nalidixic acid and chloramphenicol
Iron acquisition
Clinical features
Symptoms
One of the main identifying symptoms of Campylobacteriosis is bloody or mucosal diarrhea. Other symptoms may include muscle pain, headache, fever, and nausea. The disease is self-limiting and most symptoms cease after 5 days. Reactive arthritis, Guillain-Barré syndrome, and bacteraemia have been known to occur, but these conditions are rare.
Morbidity and Mortality
Campylobacter has a high infection rate of 1.3 million a year and a low mortality rate of 76 a year. Mortality is usually due to rare complications such as Guillain-Barre syndrome and impoverished environments dehydration. For the most part Campylobacter passes through ones system without any residual effects.
Diagnosis
Diagnosis of Campylobacter is done by confirming its presence in the patient’s stool. The two methods currently used in identification are growth on a selective medium such as Preston Campylobacter selective agar (Bolton F.J. and Robertson L. (1982) J. Clin. Pathol. 35. 462-467.) and Polymerization Chain Reaction (PCR) (World J Gastroenterol. 2013 May 28; 19(20): 3090–3095. Published online 2013 May 28. doi: 10.3748/wjg.v19.i20.3090 PMCID: PMC3662949 Mao-Jun Zhang, Bo Qiao, Xue-Bin Xu, and Jian-Zhong Zhang)to determine the DNA presence of Campylobacter jejuni as well as other related species and subspecies.
Treatment
Treatment of Campylobacteriosis is done by managing the symptoms and any complications until the symptoms subside. Symptoms mainly include diarrhea leading to dehydration, and vomiting. Antibiotics can be used but are not usually administered unless serious complications arise. A majority of people recover from the symptoms within a week; however, some cases have known to take up to approximately 10 days.
Replacements of fluids and electrolytes lost during diarrhea and vomiting are keys to recovery and preventing symptoms from being prolonged. Water or rehydration drinks are recommended. Drinks such as soda and fruit juices contain too much sugar and too few electrolytes to be considered effective treatments for dehydration.
Maintaining a normal diet as much as possible will help in recovering faster. Avoid foods that have high fat and sugar content as well as spicy foods, alcohol, and coffee until approximately 2 days after symptoms subside. (Centers for Disease Control and Prevention (2010). Campylobacter. Available online: http://www.cdc.gov/nczved/divisions/dfbmd/diseases/campylobacter.)
Prevention
Several leading organizations including WHO, CDC, FDA, USDA, and state health departments have ongoing studies, investigations, and monitoring of Campylobacter across the world. Although the bacteria spreads through fecal oral transmission, a majority of infections occur from food born contamination, especially unpasteurized milk and poultry products.
Risk Avoidance
Proper food handling and washing hands are key practices to prevent the spread of Campylobacter jejuni.
• Make sure that the meat is cooked throughout (no longer pink in the center). All poultry should be cooked to at least an internal temperature of 165°F.
• Wash hands with soap before and after preparing food, especially raw meats.
• Prevent cross-contamination while preparing foods by using separate cutting boards for raw meats and other foods
• Cleaning all cutting boards, kitchen countertops, and silverware with soap and hot water.
• Do not drink unpasteurized milk or untreated surface water.
• Be sure that persons with diarrhea wash their hands carefully and frequently with soap to help reduce the risk of spreading the infection.
• Washing hands with soap after coming in contact with pet feces.
Centers for Disease Control and Prevention 1600 Clifton Rd. Atlanta, GA 30333, USA < http://www.cdc.gov/nczved/divisions/dfbmd/diseases/campylobacter/>
Immunization
Studies are still ongoing as to human vaccinations and immunizations against Campylobacter jejuni. Currently there are Immunizations available to chickens. Conventional methods of using heat or chemically killed vaccines have not completely protected against infection occurring. Using nanoparticales and constructing a DNA vaccine that targets the flagellum of the bacteria, which is a key mechanism of attachment in the gastrointestinal tract, have resulted in a significant decrease in the campylobacter’s ability to colonize the host. (Intranasal Immunization with Chitosan/pCAGGS-flaA Nanoparticles Inhibits Campylobacter jejuni in a White Leghorn Model, Jin-lin Huang, Yan-Xin Yin, [...], and Xin-an Jiao, Journal of Biomedicine and Biotechnology. 2010; 2010: 589476)
Host Immune Response
References
References
Created by Halen Borron, Kelley Raines, and Evan Robinson, students of Tyrrell Conway at the University of Oklahoma.
