Clostridium sporogenes
1. Classification
a. Higher order taxa
Domain Bacteria; Phylum Firmicutes; Class Clostridia; Order Clostridiales; Family Clostridaceae; Genus Clostridium
2. Description and significance
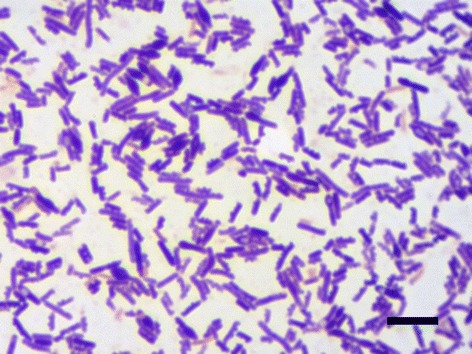
Clostridium sporogenes is a Gram-positive, rod shaped bacteria that exhibits spore production and flagellar motility (1). C. sporogenes can be found in a variety of places including: soil, sediment in both marine and freshwater environments, preserved meat and dairy products, fecal matter, snake venom, and infections in domestic animals and humans (1). C. sporogenes is phenotypically similar to other members of its genus C. difficile and C. botulinum, but it lacks the capability to produce the neurotoxin botulinum that causes human disease. Therefore, C. sporogenes is classified as a harmless biosafety level I organism by the American Type Culture Collection (13). This classification of C. sporogenes makes it a viable candidate for use in the medical field. For example, C. sporogenes spores only release pathogens in tumor-specific vectors, having potential to be beneficial in cancer treatments aiming to reduce damage to non-cancerous cells within the host (20).
3. Genome structure
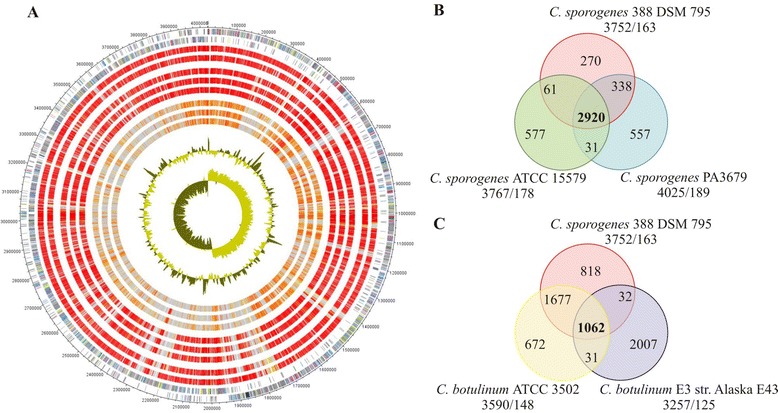
The Clostridium sporogenes DSM 795 genome, the first strain of C. sporogenes ever to be isolated, consists of a single circular chromosome 4.1 Mega-base pairs in length with an overall GC content of 27.81% (18). A total of 3,832 genes are encoded by the genome; 3,744 genes have been identified as protein coding via computational analysis (i.e. they contain an open reading frame of 300 or more bases within the gene sequence), and 80 genes have been identified to encode RNAs (10 rRNA genes and 70 tRNA genes). Six different genes that encode selenocysteine-containing proteins are located within the genome. Selenocysteine has a lower reduction potential than cysteine, therefore, it is preferred over cysteine in proteins involved in antioxidant activity (19).
Clostridium botulinum strain A consists of a circular chromosome 3.9 Mega-base pairs in length with an overall GC content of 28.2%. A plasmid of 16,344 base pairs is also found within the genome (6). 16S rDNA sequence analysis shows a 99.7% sequence similarity between Clostridium sporogenes and Clostridium botulinum strain A. Similarity between C. sporogenes and C. botulinum is furthered by the 2,016 orthologous genes shared between the two.
4. Cell structure
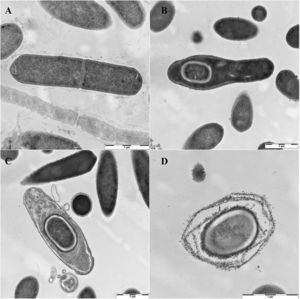
Clostridium sporogenes are rod-shaped bacteria, typically linked in long chains, that are Gram-positive. The cell wall consists of a thick layer of peptidoglycan, a polymer of amino acids and sugar (21). Other components anchored in the cell wall, such as teichoic acid and proteins, protrude out of the peptidoglycan layer, giving the cell surface a rigid look. C. sporogenes exhibit motility using flagella (3). Motility plays an important role in the bacterium’s reaction to stimuli. Cell membranes containing stimuli receptors detect stimuli causing activation of the flagella. If the stimuli is sensed as beneficial, the flagella orient cellular movement towards the stimuli (and visa versa). Like other members of the Clostridium genus, C. sporogenes produce endospores as a mechanism to survive unfavorable environmental conditions, thus making the bacterium difficult to kill (7). An important distinction between C. sporogenes and its close relative C. botulinum is that C. sporogenes does not produce botulinum neurotoxins.
5. Metabolic processes
C. sporogenes are obligate anaerobes, so they can neither utilize nor survive in the presence of oxygen. The bacterium obtains energy through the fermentation of amino acids, also known as Stickland fermentation (3) In the Stickland reaction an electron donor amino acid is oxidized into a carboxylic acid one carbon shorter than the original amino acid, while an electron acceptor amino acid is reduced into a carboxylic acid the same length as the previous amino acid (17). This mechanism allows C. sporogenes to avoid the use of [H+] ions as electron acceptors (9). While nutrition is more commonly supplied by amino acid fermentation, glucose fermentation, where glucose is broken down into ethanol and carbon dioxide, can be utilized as a secondary source of nutrition. C. sporogenes is considered a neutrophile, thus having an optimal pH range of about 6.0 – 7.6 (3).
6. Ecology
Clostridium sporogenes is commonly isolated from soil, marine and fresh lake water sediment, preserved meat and dairy product, human intestines as well as human infections (3). Some strains are capable of producing bacteriocin-like substances that can inhibit other C. sporogenes strains (4). In the gut microflora of human, C. sporogenes converts tryptophan into indole and subsequently indole-3-propionic acid (IPA), a potent antioxidant in human body (12) that being investigated as a possible treatment for Alzheimer's disease (2).
7. Pathology
Unlike Clostridium botulinum, C. sporogenes does not carry plasmids that are responsible for neurotoxicity (22). C. sporogenes toxins can induce hemorrhage in rabbit but not in other animals (10). Although isolated from many infections, the role of C. sporogenes as pathogen has been not yet determined. However, the highly proteolytic nature of C. sporogenes is thought to possibly act as adjuvant for opportunistic pathogens in human and animal infections (3).
8. Medical Applications
Due to its anaerobic nature and sporulation, C. sporogenes colonizes specific hypoxic areas of solid tumor when intravenously delivered into tumor-transplanted mice (16). Combined administration of C. sporogenes with enzyme for antitumor prodrug cleavage is currently being investigated as a promising and low-toxicity treatment in cancer therapy (14) (15)
9. Current Research
Spores of C. sporogenes target the hypoxic core of a tumor and can cause the tumor to lyse as a reaction to simple reproduction and expansion of the bacteria. C. sporogenes can be effectively transformed with a plasmid expressing prodrug-converting enzyme (PCE) that cleaves nontoxic, pre-administered prodrug CB1954 into its cytotoxic form which lyses solid tumor at the hypoxic core (11). The experiment was repeated three times over the period of seventy days, and no microenvironmental shifts were observed in the tumor area (11). The same specificity was demonstrated in the transformation through conjugation of C sporogenes with cytosine deaminase (CD) plasmid, whose product can cleave the pre-administered 5-flourocytosine (5-FC) into the cytotoxic 5-flourouracil (5-FU) for tumor lysis (15). However, due to high risk of infection and toxicity after the spore germinated in tumor-bearing animal (8), bacterial treatment is not widely accepted. Researchers have attempted to overcome this limitation by heat-inactivating C.sporogenes to produce its non-viable derivative before administration to a tumor culture. Non-viable C. sporogenes have demonstrated an ability to inhibit colorectal cancer cells in vivo (5).
10. References
[1] ABIS Encyclopedia. “Clostridium sporogenes.” ABIS Encyclopedia. Regnum Prokaryote, n.d. Web.
[2] Bendheim, Paul E., et al. "Development of indole-3-propionic acid (OXIGON™) for alzheimer’s disease.” Journal of Molecular Neuroscience 19.1-2 (2002): 213-217.
[3] Bergey, D. H., William B. Whitman, Paul De Vos, George M. Garrity, and D. Jones. "Genus I. Clostridium.” Bergey's Manual of Systematic Bacteriology. 9th ed. Vol. 3. New York: Springer, (2009). 817. Print.
[4] Betz, John V., and Kenneth E. Anderson. "Isolation and characterization of bacteriophages active on Clostridium sporogenes.” Journal of bacteriology 87.2 (1964): 408-415.
[5] Bhave, Madhura Satish et al. “Effect of Heat-Inactivated Clostridium Sporogenes and Its Conditioned Media on 3-Dimensional Colorectal Cancer Cell Models.” Scientific Reports 5 (2015): 15681. PMC. Web.
[6] Bradbury, Mark, et al. "Draft genome sequence of Clostridium sporogenes PA 3679, the common nontoxigenic surrogate for proteolytic Clostridium botulinum.” Journal of bacteriology 194.6 (2012): 1631-1632.
[7] Brunt, Jason et al. “Functional Characterisation of Germinant Receptors in Clostridium Botulinum and Clostridium Sporogenes Presents Novel Insights into Spore Germination Systems.” Ed. Abraham L. Sonenshein. PLOS Pathogens 10.9 (2014): e1004382. PMC. Web.
[8] Dang, Long H. et al. “Combination Bacteriolytic Therapy for the Treatment of Experimental Tumors.” Proceedings of the National Academy of Sciences of the United States of America 98.26 (2001): 15155–15160. PMC. Web.
[9] Golovchenko, N. P., B. F. Belokopytov, and V. K. Akimenko. "Glucose metabolism in Clostridium sporogenes and Clostridium sticklandii bacteria.” Mikrobiologiia 52.6 (1983): 869.
[10] Hara, K, Y., A. Ogura, Y. Noguchi, and S. Kumagai. "Characteristics of Toxicity and Haemorrhagic Toxin Produced by Clostridium Sporogenes in Various Animals and Cultured Cells.” Journal of Medical Microbiology 46.4 (1997): 270-75. Web.
[11] Heap, John T. et al. “Spores of Clostridium Engineered for Clinical Efficacy and Safety Cause Regression and Cure of Tumors in Vivo.” Oncotarget 5.7 (2014): 1761–1769. Web.
[12] Karbownik, Małgorzata, et al. "Indole‐3‐propionic acid, a melatonin‐related molecule, protects hepatic microsomal membranes from iron‐induced oxidative damage: Relevance to cancer reduction.” Journal of cellular biochemistry 81.3 (2001): 507-513.
[13] Kubiak, Aleksandra M. et al. “Complete Genome Sequence of the Nonpathogenic Soil-Dwelling Bacterium Clostridium Sporogenes Strain NCIMB 10696.” Genome Announcements 3.4 (2015): e00942–15. PMC.
[14] Lambin, Philippe, et al. "Colonisation ofClostridiumin the body is restricted to hypoxic and necrotic areas of tumours.” Anaerobe 4.4 (1998): 183-188.
[15] Liu, S. C., et al. "Anticancer efficacy of systemically delivered anaerobic bacteria as gene therapy vectors targeting tumor hypoxia/necrosis.” Gene therapy 9.4 (2002): 291-296.
[16] Minton, N. P. "Clostridia in cancer therapy.” Nature reviews. Microbiology 1.3 (2003): 237.
[17] Nisman, B. "The stickland reaction.” Bacteriological reviews 18.1 (1954): 16.
[18] Poehlein, Anja, et al. "Genome sequence of Clostridium sporogenes DSM 795T, an amino acid-degrading, nontoxic surrogate of neurotoxin-producing Clostridium botulinum.” Standards in genomic sciences 10.1 (2015): 1-12.
[19] Schnabel, R., E. Lubos, CR Sinning, PS Wild, T. Munzel, and S. Blankenberg. "Selenium Supplementation Improves Antioxidant Capacity in Vitro and in Vivo in Patients with Coronary Artery Disease The Selenium Therapy in Coronary Artery Disease Patients (SETCAP) Study.” National Center for Biotechnology Information 156 (2008). Web.
[20] Theys, J et al. “Repeated Cycles of Clostridium-Directed Enzyme Prodrug Therapy Result in Sustained Antitumour Effects in Vivo.” British Journal of Cancer 95.9 (2006): 1212–1219. PMC.
[21] Vollmer, Waldemar, and Joachim-Volker Höltje. "The architecture of the murein (peptidoglycan) in gram-negative bacteria: vertical scaffold or horizontal layer (s)?.” Journal of bacteriology 186.18 (2004): 5978-5987.
[22] Weickert, M J, G H Chambliss, and H Sugiyama. “Production of Toxin by Clostridium Botulinum Type A Strains Cured by Plasmids.” Applied and Environmental Microbiology 51.1 (1986): 52–56. Print.
[23] Wikoff, William R. et al. “Metabolomics Analysis Reveals Large Effects of Gut Microflora on Mammalian Blood Metabolites.” Proceedings of the National Academy of Sciences of the United States of America 106.10 (2009): 3698–3703. PMC. Web.
Edited by Kristina Platt, Phuong Nguyen, Sakib Hossain, students of Jennifer Talbot for BI 311 General Microbiology, 2014, Boston University.
