Microbiota of the Human Ear: Difference between revisions
Hardackerk (talk | contribs) No edit summary |
Hardackerk (talk | contribs) |
||
| Line 58: | Line 58: | ||
<br><b>Outer Ear</b><br> | <br><b>Outer Ear</b><br> | ||
<br>The outer ear is protected by the skin and earwax. The skin forms a physical barrier to the entry of pathogenic microbes, and earwax, as mentioned above, prevents tearing of the skin by means of lubrication and prevents microbial growth through the presence of antimicrobial proteins in the earwax.[[#References|<sup>[2][16][24]</sup>]] However, outer ear infections do occur due to a variety of reason. | <br>The outer ear is protected by the skin and earwax. The skin forms a physical barrier to the entry of pathogenic microbes, and earwax, as mentioned above, prevents tearing of the skin by means of lubrication and prevents microbial growth through the presence of antimicrobial proteins in the earwax.[[#References|<sup>[2][16][24]</sup>]] However, outer ear infections do occur due to a variety of reason. The environmental conditions have a substantial impact on the development of external auditory infections. Warm, humid, and tropical climates increase the occurrence of ear infections. Cerumen does come in two morphotypes. Studies show that the wet cerumen yields increased growth in <i>E. coli</i>, <i>S. epidermidis</i>, and <i>Corynebacterium</i>.[[#References|<sup>[4]</sup>]] Removal of earwax can greatly increase the incidence of outer ear infections due to abrasions and the removal of the antimicrobial properties that accompany earwax.[[#References|<sup>[22]</sup>]] Common infections of the outer ear include acute diffuse otitis externa and otomycosis. Infections of the outer ear are referred to as otitis externa or external otitis.<br> | ||
<br><u><i>Pseudomonas aeruginosa</i></u> | <br><u><i>Pseudomonas aeruginosa</i></u> | ||
Revision as of 23:19, 5 May 2015
By Kyle Hardacker
Introduction
The human body can be thought of as a superorganism. Many microbes can be found in or around the human body and microbial cells are in much higher abundance than human cells. The human body serves as a microbial ecosystem with a wide variety of environments ranging from the skin to mucous membranes and the digestive tract. Due to the microbial environmental diversity in and around the human body, the microbial population varies depending on location. This confers a wide range of bacteria and other microbes inhabiting the human body. The human ear serves as a unique environment with its own microbiome due to its distinct anatomy.[3]
Anatomy & Physiology of the Ear
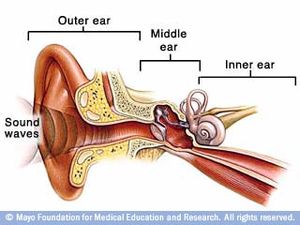
Three main compartments subdivide the human ear: the outer, middle and inner ear. Figure 1 shows the three different sections of the human ear. Figure 2 shows more details, and various structures in each section of the ear.
Outer Ear
The outer ear consists of the fleshy outer portion most commonly thought of when picturing the ear. This structure is referred to as the auricle or the pinna and is supported by cartilage. The auricle functions to funnel sound from the environment into the next section of the outer ear, the external auditory meatus. The external auditory meatus is the ear canal that leads to the tympanic window. The external auditory meatus is the passageway through the temporal bone and is coated in cerumen (earwax). The outer ear is exposed to the environment and is covered in skin. Earwax is produced in the outer ear in order to clean and lubricate the skin of the outer ear. Earwax contains a mixture of hydrocarbons, fatty acids, and cholesterol as well as a mix of antimicrobial proteins.[24][26] Earwax is produced by a combination of sebaceous and apocrine glands in the outer third portion of the outer ear.[2] The skin of the ear canal grows from inside to out and pushes skin cells to the exterior of the ear where it is eventually shed. This process expels the cerumen from the ear canal.[1] Human cerumen is dimorphic with wet and dry morphotypes.[18] The external auditory meatus terminates at the tympanic membrane (tympanic window or eardrum). The tympanic membrane is the thin membrane that separates the outer and middle ear.[1][2]
Middle Ear
The middle ear, or tympanic cavity, is an air-filled cavity contain a set of three ossicles: the malleus, incus and stapes. The ossicles are conjoined sequentially with the malleus anchored to the tympanic membrane and the stapes anchored to the inner ear. The hammer, anvil, and stirrup respectively conduct the oscillations of the tympanic membrane from sound vibrations entering the outer ear to the inner ear via the oval window. The Eustachian tube connects the middle ear to the nasopharynx and functions to equilibrate air pressure between the middle and outer ear to prevent perforation of the ear drum. This is the reason that people can pop their ears by closing their mouth, plugging their nose and exhaling. The increase in pressure in the nasopharynx is transmitted into the middle ear via the Eustachian tube, causing the tympanic membrane to pop.[1][2]
Inner Ear
The inner ear contains the organs and nerves that are involved in hearing and balance. The cochlea separates the inner and middle ear and is the snail-shaped auditory organ. The oval window of the cochlea vibrates as sound is conducted into the inner ear and the vibrations of the oval window. The perilymph inside the cochlea conducts the sound waves to the vestibular membrane. Inside of the vestibular membrane is endolymph fluid that conducts sound to the basilar membrane. Inside the basilar membrane, specialized hairs detect the sound waves and the action potentials created are sent to the brain via the vestibulocochlear nerves. The vestibule and semicircular canals function to maintain balance. The vestibule and semicircular canals sense the motion of the endolymph with specialized hair cells and assess the bodies position with respect to gravity. The action potentials are sent to the brain via the vestibulocochlear nerve. The endolymph and perilymph differ based on the potassium and sodium concentration. The endolymph contains higher concentration of potassium ions than sodium ions.[13] The difference in ion concentrations between the two presents a different environment to potential bacteria.
Microbiota of the Ear

Outer Ear
The outer ear is exposed to the external environment and much like skin on other parts of the human body is in contact with microbial life. Both the auricle and the external auditory meatus house a variety of microbes under healthy conditions. The outer ear is exposed to the outside oxygen-filled environment, the majority of the bacterial flora on the auricle and in the external auditory canal is made up of aerobic species.[4] The outer ear is home to a diverse set of microbes including bacteria, viruses, and fungi.[3]
Bacteria in the Auricle & Skin of External Auditory Meatus
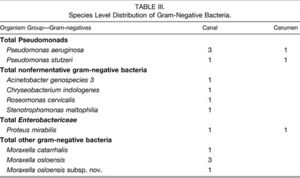
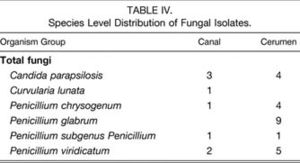
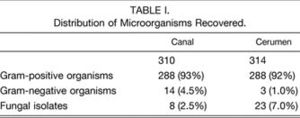
The skin of the external auditory canal and auricle is predominantly occupied by Gram-positive over Gram-negative bacteria (Fig. 3). The main Gram-positive bacteria are staphylococci, coryneforms, streptococci and enterococci, micrococci, and bacillus (Fig. 4). Of the Gram-positive bacteria, the predominant species are Staphylococcus auricularis, S. capitis (both capitis and ureolyticus), S. epidermidis, S. warnen, Turicella otitidis, Alloiococcus otitis, Micrococcus luteus, and E. coli (Fig. 5).[5] Gram-negative species inhabit the auricle and skin of the external auditory meatus to a much lesser extent with Pseudomonas aeruginosa and Moraxella osloensis in relative abundance. Some fungal microbes can be found in the skin of the outer ear, but are less abundant than either Gram-positive or Gram-negative bacteria. Candida parapsilosis, C. albicans, and Penicillium species form the majority of fungal isolates of the ear integument (Fig. 6).[25][27]
Bacteria in Cerumen
The skin and the cerumen present different microbial populations in the external ear. Gram-positive bacteria still dominate the bacterial flora and the species distribution is relatively similar to that in the skin (Fig. 3). However, the Gram-negative bacteria species are less common in the cerumen than the canal and almost non-existent in the cerumen with Pseudomonas present (Fig. 3 & 5). Interestingly, fungal microbes across the board are more common in cerumen than the canal with similar species distribution (Fig. 3 & 6).[27] Earwax functions to prevent desiccation of the ear canal by lubricating the passageway, which prevents the thin layer of skin lining the ear canal from abrasion and subsequent infection.[2] Earwax also serves to protect the external auditory canal from microbial infection. Earwax not only is pushed out of the ear by skin growth, thereby physically removing microbes from the ear, earwax also contains antimicrobial peptides that prevent bacterial infestation of the ear.[1][5][16][24] Proteins in cerumen chemically prevent microbes from taking hold in the outer ear and serve as an important barrier to ear infections. These proteins suppress the growth rate of many bacterial and fungal microorganisms in the outer ear including E. coli, P. aeruginosa, S. aureus and C. albicans.[16] Certain bacteria may or may not be completely wiped out, but cerumen keeps bacteria in the outer ear under control.[16][24][27]
Middle Ear
Although the middle ear is segregated from the external portion of the ear via the tympanic membrane the middle ear is connected to the nasopharynx by the way of the Eustachian tube. In this way the middle ear is somewhat in contact with the external environment. However, bacteria would still need to travel through the nasal cavity and up the Eustachian tube which is no easy task. The mucous and cilia in the nasal cavity function to trap and expel foreign particles including bacteria that may travel up to the middle ear.[6] That being said microbes are present in the middle ear. For instance alpha hemolytic streptococci are present in a healthy middle ear.[23]
Inner Ear
Unlike the outer and middle ear, the inner ear is completely secluded from the outside environment. The cochlea, semicircular canals, and vestibule are enclosed by the bony labyrinth. This makes it much more difficult for bacteria to translocate across the oval window. The immune system is more prevalent in the inner ear which also reduces the possibility of microbial entry into the inner ear.[1][2]
Commensal Bacteria
Infections of the Ear

Outer Ear
The outer ear is protected by the skin and earwax. The skin forms a physical barrier to the entry of pathogenic microbes, and earwax, as mentioned above, prevents tearing of the skin by means of lubrication and prevents microbial growth through the presence of antimicrobial proteins in the earwax.[2][16][24] However, outer ear infections do occur due to a variety of reason. The environmental conditions have a substantial impact on the development of external auditory infections. Warm, humid, and tropical climates increase the occurrence of ear infections. Cerumen does come in two morphotypes. Studies show that the wet cerumen yields increased growth in E. coli, S. epidermidis, and Corynebacterium.[4] Removal of earwax can greatly increase the incidence of outer ear infections due to abrasions and the removal of the antimicrobial properties that accompany earwax.[22] Common infections of the outer ear include acute diffuse otitis externa and otomycosis. Infections of the outer ear are referred to as otitis externa or external otitis.
Pseudomonas aeruginosa
One of the most common outer ear infections is acute diffuse otitis externa, pictured in figure 7. Commonly referred to as swimmer’s ear, the main microbial agent is P. aeruginosa. Swimmer’s ear can be caused by swimming in polluted water or by cleaning one’s ears with Q-tips.[22] P. aeruginosa is present in the outer ear of healthy individuals but does not normally cause infection.[27] However P. aeruginosa is able to infect immune compromised individuals. When water is trapped in the ear or earwax is removed via Q-tips allows P. aeruginosa to grow relatively unchecked because of favorable conditions or antimicrobial earwax deficiency.[22] Polluted water may contain an excess of bacteria or an abrasion in the skin could allow P. aeruginosa entry from the environment. In any case, once P. aeruginosa gains access to the outer ear and is able to reproduce to reach a critical mass, the ear becomes inflamed, itchy, irritated, and painful. The ear becomes crusty obstructed leading to conductive hearing loss. Cleansing of the ear canal as well as antibiotic treatment via ear drops can reduce and ultimately eliminate swimmer’s ear.[22]
P. aeruginosa can also infect the auricle via ear piercings. Piercing of the upper ear cartilage leads to an external ear infection which presents with swelling, inflammation, irritation, and drainage of pus and/or blood.[12] Infection via S. aureus can occur in a similar fashion due to ear piercing from untrained individuals.
Aspergillus niger & Candida albicans

Otomycosis is another common outer ear infection. There are multiple causes of otomycosis but the most common causes are A. niger and C. albicans. The fungal microbes cause symptoms of pain, hearing loss, aural fullness, and itching. In extreme cases otomycosis can permanently damage the ear canal and the tympanic membrane leading to hearing loss.[10] C. albicans, like P. aeruginosa, is present in normal outer ear microbiota.[27] C. albicans is also an opportunistic pathogen, attacking immune compromised individuals. Most of the C. ablicans in the human body resides in the human gut, but C. albicans is also found in the exterior of the human ear.[27] Otomycosis is treatable with the usage of antifungal drops into the ear.[10]
Middle Ear
Middle ear infections are termed otitis media. Since the middle ear is not directly accessible by bacteria from the external environment, bacteria must either travel up the Eustachian tube or through a perforated tympanic membrane in order to access the middle ear.[1][2] According to the CDC, there are three main forms of otitis media that are caused by various microbes: acute otitis media, otitis media with effusion, and chronic suppurative otitits media. This article focuses on the more common acute otitis media and the microbes responsible.
Alloiococcus otitis & Turicella otitidis
Some causes of otitis media are caused by bacteria found in the outer ear. Both A otitis and T. otitidis can be found in the normal microbial flora of the outer ear yet do not cause infection of the outer ear.[27][29] There is controversy over whether these bacteria cause acute otitis media. Some say they play no role, some say they cause middle ear infection, and some say that these two bacteria enter the middle ear through the tympanic membrane when it is inflamed by an already pre-existing ear infection with the presence of the two microbes only serve to prolong the middle ear infection.[30] This highlights the complex interplay between the microbiome and the human body. A. otitis and T. otitidis are commensal in the external auditory meatus yet possibly pathogenic in the middle ear.
Streptococcus pneumoniae & Haemophilus influenzae & Moraxella catarrhalis
These microbes are the most common cause for acute otitis media.[15] S. pneumoniae, H. influenzae, and M. catarrhalis are all associated with the upper respiratory tract of humans.[19] They access the middle ear via the Eustachian tube connecting to the nasopharynx.
Both S. pneumoniae and H. influenzae are facultative anaerobes which makes them well-suited for the tympanic cavity environment.[19] Once the microbes have taken hold in the middle ear patients present with ear pain, drainage of fluid and diminished hearing.[15] Acute otitis media is common is children and presents with additional symptoms such as increased irritability, fever of 100 °F or higher, and difficulty sleeping.[8] In most cases acute otitis media will resolve itself without treatment; However, in the severe cases amoxicillin is administered as a first line of defense. This is only done in severe cases to avoid adverse side effects of the antibiotics on young children.[15]
Moraxella catarrhalis is another upper respiratory bacterium that is known to migrate to the inner ear causing acute otitis media.[19]
Inner Ear
The inner ear is quarantined off from the rest of the ear by the bony labyrinth that encases the cochlea, semicircular canals, and vestibule. There is no access to the external environment via the external auditory canal and Eustachian tube for the outer and middle ear respectively. In most cases the cause of inner ear infections are usually viral. The two main inner ear maladies are vestibular neuritis and Labyrinthitis. Both of these conditions affect the balance of an individual and cause vertigo and sometimes nausea. Both vestibular neuritis and Labyrinthitis onset are preceded by an upper respiratory infection such as the common cold, herpes simplex virus, or flu.[17]
Vestibular neuritis
Labyrinthitis
In both cases the cause is viral (although the exact causes have yet to be fully uncovered), but Labyrinthitis can have bacterial causes such as meningitis or middle ear infections. Vestibular neuritis and Labyrinthitis both deal with improper neuron output. Vestibular neuritis is caused by imbalance of neuron input between each ears and leads to dizzying and confusing interpretation of the signals by the brain. This causes the vertigo and nausea. Also, vestibular neuritis does not affect hearing.[17] Labyrinthitis disrupts the vestibular nerve leading to severe vertigo and imbalance by causing inflammation of the bony labyrinth, specifically the vestibule and vestibular nerve.
Beneficial Ear Microbiota
Good Microbes and the Microbiome
More and more scientists are beginning to realize that the interplay between the human body and naturally occurring biological flora can be beneficial for both the host and the microbe.[3] In order to restore proper gut health fecal transplants were performed in order to replace the beneficial bacteria.[11] This logic has been extended to the treatment of ear infections. Alpha hemolytic streptococci are present in the middle ear naturally and evidence notion that these bacteria effectively interfere with the activity of S. pneumonia, H. influenza, and M. catarrhalis. In this way alpha hemolytic streptococci and other probiotics can be utilized to combat pesky ear infecitons by essentially replacing the naturally occurring bacterial flora in the middle ear in this case.[7][23][29]
References
[1] Alberti, P.W. (1988) The Anatomy and Physiology of the Ear and Hearing. Otologic Medicine and Surgery, 54-63.
[2] Alvord, L. S. & Farmer, B. L. (1997). Anatomy and orientation of the human external ear. J Am Acad Audiol 8, 383-390.
[3] Belkaid, Y. & Segre, J. A. (2014). Dialogue between skin microbiota and immunity. In Science, pp. 954-959. United States: American Association for the Advancement of Science.
[4] Brook, I. (1981). Microbiological studies of the bacterial flora of the external auditory canal in children. Acta Otolaryngol 91, 285-287.
[5] Campos, A., Betancor, L., Arias, A., Rodriguez, C., Hernandez, A. M., Lopez Aguado, D. & Sierra, A. (2000). Influence of human wet cerumen on the growth of common and pathogenic bacteria of the ear. J Laryngol Otol114, 925-929.
[6] Dahl, R. & Mygind, N. (1998). Anatomy, physiology and function of the nasal cavities in health and disease. In Adv Drug Deliv Rev, pp. 3-12.
[7] Di Pierro, F., Donato, G., Fomia, F., Adami, T., Careddu, D., Cassandro, C. & Albera, R. (2012). Preliminary pediatric clinical evaluation of the oral probiotic Streptococcus salivarius K12 in preventing recurrent pharyngitis and/or tonsillitis caused by Streptococcus pyogenes and recurrent acute otitis media. In Int J Gen Med, pp. 991-997. New Zealand.
[8] Froom, J., Culpepper, L., Grob, P. & other authors (1990). Diagnosis and antibiotic treatment of acute otitis media: report from International Primary Care Network. BMJ 300, 582-586.
[9] Harimaya, A., Takada, R., Hendolin, P. H., Fujii, N., Ylikoski, J. & Himi, T. (2006). High incidence of Alloiococcus otitidis in children with otitis media, despite treatment with antibiotics. In J Clin Microbiol, pp. 946-949. United States.
[10] Ho, T., Vrabec, J. T., Yoo, D. & Coker, N. J. (2006). Otomycosis: clinical features and treatment implications. In Otolaryngol Head Neck Surg, pp. 787-791. United States.
[11] Kassam, Z., Hundal, R., Marshall, J. K. & Lee, C. H. (2012). Fecal transplant via retention enema for refractory or recurrent Clostridium difficile infection. In Arch Intern Med, pp. 191-193. United States.
[12] Keene, W. E., Markum, A. C. & Samadpour, M. (2004). Outbreak of Pseudomonas aeruginosa infections caused by commercial piercing of upper ear cartilage. In JAMA, pp. 981-985. United States.
[13] Konishi, T., Hamrick, P. E. & Walsh, P. J. (1978). Ion transport in guinea pig cochlea. I. Potassium and sodium transport. Acta Otolaryngol 86, 22-34.
[14] Lee, S. H., Chung, M. H., Lee, J. S., Kim, E. S. & Suh, J. G. (2006). A case of Staphylococcus aureus endocarditis after ear piercing in a patient with normal cardiac valve and a questionnaire survey on adverse events of body piercing in college students of Korea. In Scand J Infect Dis, pp. 130-132. Sweden.
[15] Lieberthal, A. S., Carroll, A. E., Chonmaitree, T. & other authors (2013). The diagnosis and management of acute otitis media. In Pediatrics, pp. e964-999. United States.
[16] Lum, C. L., Jeyanthi, S., Prepageran, N., Vadivelu, J. & Raman, R. (2009). Antibacterial and antifungal properties of human cerumen. In J Laryngol Otol, pp. 375-378. England.
[17] Marill, K.A. (2011). Vestibular Neuronitis : Pathology. eMedicine. Medscape Reference
[18] Matsunaga, E. (1962). The dimorphism in human normal cerumen. Ann Hum Genet 25, 273-286.
[19] Monso, E., Ruiz, J., Rosell, A., Manterola, J., Fiz, J., Morera, J. & Ausina, V. (1995). Bacterial infection in chronic obstructive pulmonary disease. A study of stable and exacerbated outpatients using the protected specimen brush. Am J Respir Crit Care Med 152, 1316-1320.
[20] Montain, S. J., Cheuvront, S. N. & Lukaski, H. C. (2007). Sweat mineral-element responses during 7 h of exercise-heat stress. Int J Sport Nutr Exerc Metab 17, 574-582.
[21] Nichols, A. C. & Perry, E. T. (1956). Studies on the growth of bacteria in the human ear canal. J Invest Dermatol 27, 165-170.
[22] Nussinovitch, M., Rimon, A., Volovitz, B., Raveh, E., Prais, D. & Amir, J. (2004). Cotton-tip applicators as a leading cause of otitis externa. In Int J Pediatr Otorhinolaryngol, pp. 433-435. Ireland.
[23] Roos, K., Hakansson, E. G. & Holm, S. (2001). Effect of recolonisation with "interfering" alpha streptococci on recurrences of acute and secretory otitis media in children: randomised placebo controlled trial. BMJ 322, 210-212.
[24] Schwaab, M., Gurr, A., Neumann, A., Dazert, S. & Minovi, A. (2011). Human antimicrobial proteins in ear wax. Eur J Clin Microbiol Infect Dis 30, 997-1004.
[25] Staley, R., Fitzgibbon, J. J. & Anderson, C. (1997). Auricular infections caused by high ear piercing in adolescents. Pediatrics 99, 610-611.
[26] Stransky, K., Valterova, I., Kofronova, E., Urbanova, K., Zarevucka, M. & Wimmer, Z. (2011). Non-polar lipid components of human cerumen. Lipids 46, 781-788.
[27] Stroman, D. W., Roland, P. S., Dohar, J. & Burt, W. (2001). Microbiology of normal external auditory canal. Laryngoscope 111, 2054-2059.
[28] Tagg, J. R. & Dierksen, K. P. (2003). Bacterial replacement therapy: adapting 'germ warfare' to infection prevention. In Trends Biotechnol, pp. 217-223. England.
[29] Tano, K., von Essen, R., Eriksson, P. O. & Sjostedt, A. (2008). Alloiococcus otitidis--otitis media pathogen or normal bacterial flora? APMIS 116, 785-790.
[30] White, R.K. (2012). The Association of Outer Ear Commensal Bacteria With Otitis Media in Children. University of Waikato. Unpublished.
Authored for BIOL 238 Microbiology, taught by Joan Slonczewski, 2015, Kenyon College.
