Onchocerciasis (Onchocerca volvulus): Difference between revisions
No edit summary |
|||
| (11 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
{{Conway}} | |||
[[File:Adultvolvulus.jpeg|320px|thumb|left|Picture of Adult <i>Onchocerca volvulus</i> worms from the World Health Organization. [[#References|[10]]] ]] | |||
==Etiology/Bacteriology== | ==Etiology/Bacteriology== | ||
| Line 10: | Line 11: | ||
| Genus = <i>Onchocerca</i> | | Genus = <i>Onchocerca</i> | ||
| species = <i>O. volvulus</i> | | species = <i>O. volvulus</i> | ||
{| | {| | ||
| Line 33: | Line 33: | ||
===Virulent Factors=== | ===Virulent Factors=== | ||
<i>O. volvulus</i> is a naturally parasitic hookworm. The reason it is so virulent to humans is the worm's ability to circumvent the innate immune response. The microfilariae that the filariae produce are capable of arresting complement action in the innate immune response[[#References|[9]]]. This is accomplished by the presence of a factor that cleaves the C3b molecule to an iC3b that will not contribute to C3 convertase. This inhibits the complement cascade from completing. Inhibiting the innate immune response also disrupts the adaptive immune response allowing the parasite to continue to thrive. | |||
==Symptoms== | ==Symptoms== | ||
| Line 53: | Line 54: | ||
==Diagnosis== | ==Diagnosis== | ||
Diagnosis of Onchocerciasis is possible through a variety of different methods. These methods include: | |||
<br /><br />• Palpation of the nodules present on an individual. Taken into account the living/travel history of a suspected individual this is a commonly described method. | |||
<br /><br />• Skin snips is the most common method described. A tool is used to scrape a razor thin piece of skin from an individual's arm. This primitive biopsy is combined with saline and examined under a microscope to view microfilariae[[#References|[6]]]. This method needs to be done on individuals that have been infected for years or the microfilariae will not be present near the epidermis. | |||
<br /><br />• Slit Lamp. This method also must be performed on particularly advanced individuals. It is the examination of the eye in search of ocular microfilariae. | |||
<br /><br />• Mazzotti test. This test is a dose of antibacterials that kill local microfilariae if a skin snip test is negative. the result kills local microfilariae and induces dermatitis that will recede in a few days due to the inflammatory reaction[[#References|[6]]]. | |||
<br /><br />• DEC patch test is the same as the Mazotti test except with topical antibiotics. Antibiotics are applied and then covered with a bandage for days. Then the patch is removed and checked for dermatitis caused by dead microfilariae. | |||
<br /><br />• An antigen dipstick assay is also available. This is the most promising, least invasive procedure. It tested 100% of positive patients plus almost 90% of future patients before any other method. This method is still in the testing phase at the time[[#References|[5]]]. | |||
<br /><br />• Nodulectomy. While the most invasive of the diagnostic techniques it is the most precise. Directly removing the adult worms from a nodule can provide an idea of the advancement of the infection and not just a diagnosis[[#References|[6]]]. | |||
==Treatment== | ==Treatment== | ||
[[File:Walkingblind.jpeg|200px|thumb|left|Children lead men affected by Onchocerciasis. [[#References|[11]]]] | |||
===Traditional=== | ===Traditional=== | ||
Traditional treatment of Onchocerciasis varies by region. Most of the treatments before pharmaceutical drugs were based on treating the symptoms of the disease and not the cause. The few attempts of treating the disease with traditional methods were based on a zoonotic approach. The cattle parasite <i> O. ochengi </i> causes very similar symptoms in cattle as <i>O. volvulus</i> does in humans. This caused one of the common treatments to be vedgetation and fruit that the cattle tended to eat[[#References|[12]]]. | |||
===Merck & Mectizan Donation Program=== | |||
On October 21, 1987 Merck Pharmaceuticals announced a break through in the treatment of Onchocerciasis. The company announced that it had developed a drug virtually free of side effects(not necessarily true) that would stop the production of microfilariae, thus preventing blindness and other severe side effects of the disease[[#References|[13]]]. The drug would also sterilize the existing filariae. This means that after approximately 15 years of treatment the patient would be parasite free. Merck then took the initiative and developed a program call the Mectizan Donation Program. Under this program any country affected by the disease that can show a financial need and the stability to distribute the drug appropriately will receive the drug for free[[#References|[3]]]. This program is working under the World Health Organization and is responsible for almost completely eradicating the illness in the Americas. The Mectizan Donation Program is Merck's largest global donation initiative reaching more than 60 million people a year in Africa, Latin America, and Yemen[[#References|[14]]]. | |||
==Prevention== | ==Prevention== | ||
| Line 84: | Line 96: | ||
[http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6220a4.htm 8] "Progress Towards the Elimination of Onchocerciasis in the Americas". 2013.CDC | [http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6220a4.htm 8] "Progress Towards the Elimination of Onchocerciasis in the Americas". 2013.CDC | ||
[http://jid.oxfordjournals.org/content/185/12/1786.short 9] Meri, T. et al. "Onchocerca volvulus microfilariae avoid complement attack by direct binding of factor H" 2002. | |||
[http://www.who.int/apoc/media/adult_worms.JPG 10] Mature Onchocerca volvulus. WHO | |||
[https://www.flickr.com/photos/medicalmuseum/3969963699/in/album-72157622366709345/ 11] Atlas of Tropical and Extraordinary Disease. National Museum of Health and Science. | |||
[http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3588050/ 12] Ndjonka, D. et al. "Natural Products as a Source for Treating Neglected Parasitic Diseases." 2013. | |||
[http://www.nytimes.com/1987/10/22/world/merck-offers-free-distribution-of-new-river-blindness-drug.html 13] "Merck Offers Free Distribution of New River Blindness Drug." 1987. New York Times. | |||
[http://www.mectizan.org/sites/www.mectizan.org/files/attachments/resources/MCT-2007-PA-003-BK.pdf 14] The Merck Mectizan Donation Program-River Blindness. 2007 | |||
Created by Tyler Potter, student of Tyrrell Conway at the University of Oklahoma. | Created by Tyler Potter, student of Tyrrell Conway at the University of Oklahoma. | ||
Latest revision as of 16:30, 11 February 2016


Etiology/Bacteriology
Taxonomy
| Domain = Animalia | Phylum = Nematoda | Class = Secernentea | Order = Spirurida | Family = Onchocecidae | Genus = Onchocerca | species = O. volvulus
Description
Onchocerciasis, also known as “River blindness” is an eye and skin infection caused by the parasitic worm Onchocerca volvulus. It is considered to be among the list of neglected tropical diseases. According to the CDC a neglected tropical diseases are a group of parasitic and bacterial diseases that attribute to substantial illness for more than one billion people globally [1]. The symptoms of onchocerciasis include nodules under the skin, debilitating itching, and eventually blindness. Onchocerciasis alone is believed to currently affect over 25 million worldwide with 300,000 completely blind and another 800,000 with substantial vision impairment [2]. The filarial worm is transmitted to human hosts through the bite of infected black flies from the genus Simulium. These flies tend to live around wetlands and large river basins, hence the common name “River blindness.” The majority of the population affected by the disease (99%) reside in the World Health Organization Africa Region while cases have been documented around the world including Central and South America [3].
Pathogenesis
Transmission
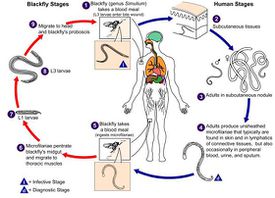
Transmission of the parasite O. volvulus is via a Simulian black fly vector. When the Simuliid black fly takes a blood meal from a an infected human host, O. volvulus larvae are present in the blood meal. A few days later the larvae has developed in the midgut of the fly and is able to travel in the saliva from the fly into a new host human when the fly feeds again. This period usually lasts about ten days from the first host to the new host. Once in the new host the maturing worm takes up residence in the subcutaneous tissue usually forming nodules or causing joint pain. Here it will mature and become filariae, the mature stage of the parasite. These filariae can live for up to 15 years and grow to be up to 80cm (32 inches) in length[4]. Once mature these filariae will produce anywhere from 700- 1800 microfilariae a day, averaging 1,600[3]. It is these microfilariae (larvae) that will cause most of the damage to the host in their attempt to reach the skin surface to be part of another Simuliid's meal. Microflariae can live in the larval stage in a human host for 3-5 years[5]. .
Epidemiology
Onchocerciasis is considered endemic across the tropical areas of Latin America, Africa and Yemen.

Usually found near large rivers or wetland areas. The tropical climates in these areas are perfectly suited for the Simuliam fly's mating habits. The Simuliid flies have aquatic larvae. This means that for the flies to complete their lifecycle the larvae require fast-flowing water in which the larvae can attach to submerged rocks or vegetation. Due to this part of the fly’s life cycle, endemic areas usually coincide with the path of rivers and streams. This fact has been confirmed with Onchocerciasis mapping[6]. Approximately 99% of infected people live on the African continent. The other 1% are located in Latin America and parts of the Middle East. It is commonly believed that Onchocerciasis was brought to the Americas by way of the slave trade. The parasite Onchocerca volvulus has become almost completely zoonotic in the areas it is known to exist in Latin America [6].
Infectious Dose, Incubation
The actual infectious dose of O. volvulus required to cause Onchocerciasis is unknown, but it is believed to take hundreds of bites from infected Simuliids to contract the disease[4]. The incubation varies from host to host and by the amount of bites from infected vectors. The generally accepted incubation period ranges from 3 months-2 years. This is considered the time from initial infection to the time that the mature filariae produce larvae.
Virulent Factors
O. volvulus is a naturally parasitic hookworm. The reason it is so virulent to humans is the worm's ability to circumvent the innate immune response. The microfilariae that the filariae produce are capable of arresting complement action in the innate immune response[9]. This is accomplished by the presence of a factor that cleaves the C3b molecule to an iC3b that will not contribute to C3 convertase. This inhibits the complement cascade from completing. Inhibiting the innate immune response also disrupts the adaptive immune response allowing the parasite to continue to thrive.
Symptoms
Onchocerciasis causes a wide array of symptoms. These can include but are not limited to:
Nodules
Skin nodules are where the adult worms reside. Normally nodules only contain 3-5 adult worms, but in extreme cases there has been up to 50 adult worms found inside a single nodule. These nodules tend to form in subcutaneous tissues over bony areas as a form of protection from the immune system. These areas include areas such as the hips, pelvis, ribs, shoulder blades, and skull[3]. If ruptured it is possible that these nodules will trigger a very painful immune response.

Onchocercal Dermatitis
Skin lesions known as Onchocercal Dermatitis are formed by the microfilariae of the parasite. Onchocercal dermatitis is characterized as an intense pruritis. It causes premature wrinkling, enlargement of femoral and inguinal lymph nodes, obstruction of the peripheral lymphatic system, and localized edema[2]. A specific form of onchocercal dermatitis has shown in Yemen known as "Sowdah." Sowdah is considered to be a form of hyperactive onchodermatitis. It causes uncontrollable itching and de-pigmentation of the skin that is commonly called "leopard skin"[7].
Onchocercal Ocular Disease/Blindness
Blindness is the most notable symptom of Onchocerciasis, but it is not immediate. As the microfilariae try to make it towards the skin in order to continue the life cycle, some of the organisms make it into the cornea of the eye. The eye is not a common spot for a Simuliid to feed. Therefore the microfilariae that make it to the eye tend to die. The corpses of the microfilariae trigger an inflammatory response that leaves scar tissue in the eye. This makes blindness very gradual, but inevitable without proper treatment. For this reason it is very rare to see anyone under the age of 30 to exhibit serious ocular deficiency. This scar tissue causes multiple issues within the eye including punctate (snowflake) keratitis, sclerosing keratitis, and iridocyclitis[2].
Morbidity/Mortality
The morbidity of Onchocerciasis varies by region due to the epidemiology of the disease. In the Americas there has been a conscious effort to eradicate the disease since 1991. By 2012 the only cases that had ocular degeneration occurred in southern Venezuela. There have not been any new cases of blindness in the Americas attributed to Onchocerciasis since 1995[8]. Unfortunately this is not the case on the African continent. That leaves more than 99% of the affected population in Africa, or approximately 18 million people as of 2007[6]. This includes almost all of the cases that are showing ocular degeneration and/or blindness. The mortality rate of Onchocerciasis is practically zero unless the disease is couple with another serious condition such as HIV.
Diagnosis
Diagnosis of Onchocerciasis is possible through a variety of different methods. These methods include:
• Palpation of the nodules present on an individual. Taken into account the living/travel history of a suspected individual this is a commonly described method.
• Skin snips is the most common method described. A tool is used to scrape a razor thin piece of skin from an individual's arm. This primitive biopsy is combined with saline and examined under a microscope to view microfilariae[6]. This method needs to be done on individuals that have been infected for years or the microfilariae will not be present near the epidermis.
• Slit Lamp. This method also must be performed on particularly advanced individuals. It is the examination of the eye in search of ocular microfilariae.
• Mazzotti test. This test is a dose of antibacterials that kill local microfilariae if a skin snip test is negative. the result kills local microfilariae and induces dermatitis that will recede in a few days due to the inflammatory reaction[6].
• DEC patch test is the same as the Mazotti test except with topical antibiotics. Antibiotics are applied and then covered with a bandage for days. Then the patch is removed and checked for dermatitis caused by dead microfilariae.
• An antigen dipstick assay is also available. This is the most promising, least invasive procedure. It tested 100% of positive patients plus almost 90% of future patients before any other method. This method is still in the testing phase at the time[5].
• Nodulectomy. While the most invasive of the diagnostic techniques it is the most precise. Directly removing the adult worms from a nodule can provide an idea of the advancement of the infection and not just a diagnosis[6].
Treatment

Traditional
Traditional treatment of Onchocerciasis varies by region. Most of the treatments before pharmaceutical drugs were based on treating the symptoms of the disease and not the cause. The few attempts of treating the disease with traditional methods were based on a zoonotic approach. The cattle parasite O. ochengi causes very similar symptoms in cattle as O. volvulus does in humans. This caused one of the common treatments to be vedgetation and fruit that the cattle tended to eat[12].
Merck & Mectizan Donation Program
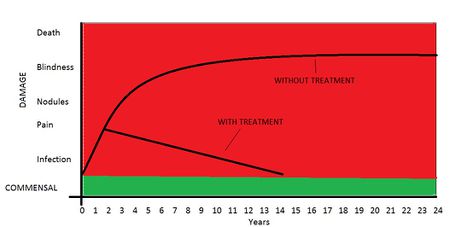
On October 21, 1987 Merck Pharmaceuticals announced a break through in the treatment of Onchocerciasis. The company announced that it had developed a drug virtually free of side effects(not necessarily true) that would stop the production of microfilariae, thus preventing blindness and other severe side effects of the disease[13]. The drug would also sterilize the existing filariae. This means that after approximately 15 years of treatment the patient would be parasite free. Merck then took the initiative and developed a program call the Mectizan Donation Program. Under this program any country affected by the disease that can show a financial need and the stability to distribute the drug appropriately will receive the drug for free[3]. This program is working under the World Health Organization and is responsible for almost completely eradicating the illness in the Americas. The Mectizan Donation Program is Merck's largest global donation initiative reaching more than 60 million people a year in Africa, Latin America, and Yemen[14].
Prevention
There have not been any drugs found that can protect against an infection from O. volvulus. Annual preventive treatment with ivermectin has displayed the ability to decrease transmission[2]. The best preventive measures are to prevent bits from the Simuliid vectors. Bug spray and avoiding large bodies of water during the mating season are good ideas in practice, but not always practical in everyday life of indigenous communities.
Host Immune Response
Damage Response Framework
References
1 Onchocerciasis. Center for Disease Control.
2 Pearson, Richard D. "Onchocerciasis"
3 Onchocerciasis or River Blindness. USAID.
4 Onchocerca volvulus. Pathogen Safety Data Sheet. Public Health Agency of Canada.
5 Udall, D. "Recent Updates on Onchocerciasis: Diagnosis and Treatment" Clinical and Infectious Diseases. Vol 44 Issue 1. 2007.
6 Goverman, D. Bass, J. Smith, S. "Onchocerciasis (River Blindness)" 2007.
7 Goldsmid, J Melrose, W. "Parasitic Infections of the Skin." The Australasian College of Tropical Medicine. 2005.
8 "Progress Towards the Elimination of Onchocerciasis in the Americas". 2013.CDC
9 Meri, T. et al. "Onchocerca volvulus microfilariae avoid complement attack by direct binding of factor H" 2002.
10 Mature Onchocerca volvulus. WHO
11 Atlas of Tropical and Extraordinary Disease. National Museum of Health and Science.
12 Ndjonka, D. et al. "Natural Products as a Source for Treating Neglected Parasitic Diseases." 2013.
13 "Merck Offers Free Distribution of New River Blindness Drug." 1987. New York Times.
14 The Merck Mectizan Donation Program-River Blindness. 2007
Created by Tyler Potter, student of Tyrrell Conway at the University of Oklahoma.