Poliovirus and its three serotypes: Difference between revisions
| Line 35: | Line 35: | ||
In the pre-vaccination era, the three serotypes were relatively equal in their frequency. This indicates that it was not until the introduction of the OPV that the type 1 virus became the most widespread, the type 2 virus became no longer endemic, and the type 3 virus became intermediately distributed [7]. Serotype 2 of the poliovirus was declared globally eradicated in 1999. | In the pre-vaccination era, the three serotypes were relatively equal in their frequency. This indicates that it was not until the introduction of the OPV that the type 1 virus became the most widespread, the type 2 virus became no longer endemic, and the type 3 virus became intermediately distributed [7]. Serotype 2 of the poliovirus was declared globally eradicated in 1999. | ||
<br> | <br> | ||
[[Image:OPV droplets better.jpg|thumb|300px|right|A child receiving an oral polio vaccine. This image is provided by the 1988 Pan American Health Organization (PAHO) and the World Health Organization (WHO). ID: 13195 URL: http://phil.cdc.gov/Phil/download.asp]] | |||
<br> | |||
A child receiving an oral polio vaccine. This image is provided by the 1988 Pan American Health Organization (PAHO) and the World Health Organization (WHO). ID: 13195 URL: http://phil.cdc.gov/Phil/download.asp | |||
==The three serotypes== | ==The three serotypes== | ||
Revision as of 20:22, 14 March 2014
The world has been battling the continuous spread of poliovirus and its associated disease poliomyelitis for a long time, with the United States officially declaring the Global Eradication Initiative against Polio in 1988. Throughout the past 26 years of eradication effort, various patterns have been observed in the spread and pathogenesis of the poliovirus. One interesting pattern is that, of the three serotypes of the virus, serotype 2 (PV2) was eradicated in 1999, while the other two serotypes (PV1 and PV3) remain endemic.
Poliovirus structure and pathogenesis
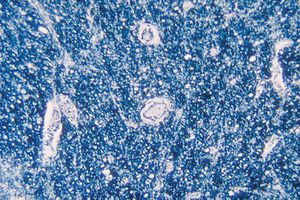
The poliovirus (PV) is a type of enterovirus, meaning it enters through the oropharynx (mouth and nasal cavities) and then replicates in the submucosal tissues of the pharynx and the gastrointestinal tract. The virus continues to be excreted from the stool for several weeks after replication begins [1]. The average incubation time for the PV is 7-14 days. During this time the virus enters the lymphoid tissues, can enter… It is a small virus (27-30 nm) that does not have an envelope but has capsids that surround its single-stranded, positive-sense RNA genome, which is about 7,500 nucleotides long [3]. The capsid is made up of 60 copies of four structural proteins: VP1, VP2, VP3, and VP4 [8]. The surfaces of structural proteins VP1, VP2, and VP3 contain antigenic sites (epitopes) to facilitate the antibody binding to the virus to neutralize it. The fourth protein, VP4, is located completely inside the capsid and plays no known role in inducing antibodies. VP1 has the most exposed surface of all the proteins, and therefore plays an important role in the immune response of all three poliovirus serotypes [4]. All three serotypes bind to the same cell-surface receptor, CD155 [2]. This receptor is present only in human cells, hence there are no other reservoirs for poliovirus.
Poliomyelitis is caused by the poliovirus, which enters the human body through the mouth or nose (oropharynx), multiplies in the tissues of the pharynx and gastrointestinal tract, and is then absorbed and spread through the circulatory and lymphatic system³[12]. Primary, or minor, transient viremia (entrance of the virus into the blood stream) occurs in most infected individuals, allowing it to spread to reticuloendothelial tissue (connective tissues, spleen, liver, lungs, bone marrow, and lymph nodes), while causing no symptoms. A secondary occurrence of viremia occurs in 4-8% of individulas, and causes minor illness, including headache, sore throat, and fever. In rare cases, less than 1%, the viremia is persistent enough that the virus can enter the central nervous system (CNS)(8)[13]. The precise mechanism by which this occurs is unknown, but one of the propose methods is entrance through the blood-brain-barrier. It remains unknown how exactly the virus breeches the blood-brain barrier, but it is thought that it travels on nerve fibers, independent of its receptor. It has also been proposed that if mononuclear phagocytes can permit viral replication, they would act as carriers for the virus to enter the CNS⁴[14]. Once inside the CNS, it characteristically causes lesions in motor neurons of the anterior horn of the cervical and lumbar regions of the spinal cord. This damage is shown in Figure…. In more severe cases, lesions are also observed in the intermediate and posterior gray columns and in sensory spinal ganglia. Most areas of the brain are unaffected, but in the brain stem, the motor and sensory nuclei of cranial nerves are affected, as well as the precentral gyrus, which is the primary motor cortex. A second prevalent theory that has been empirically supported by studies with mice indicates that the virus enters the CNS through retrograde axonal transport from muscle to spinal cord (FIG. 5 illustrates (8)). The variation of the degree to which the virus causes physical symptoms has been one of the problems in the effort to eradicate poliovirus globally.
At right is a sample image insertion. It works for any image uploaded anywhere to MicrobeWiki. The insertion code consists of:
Double brackets: [[
Filename: Ebola virus 1.jpeg
Thumbnail status: |thumb|
Pixel size: |300px|
Placement on page: |right|
Legend/credit: Electron micrograph of the Ebola Zaire virus. This was the first photo ever taken of the virus, on 10/13/1976. By Dr. F.A. Murphy, now at U.C. Davis, then at the CDC.
Closed double brackets: ]]
Other examples:
Bold
Italic
Subscript: H2O
Superscript: Fe3+
Overall paper length should be 3,000 words, with at least 3 figures with data.
The eradication effort
President Roosevelt, who contracted poliomyelitis himself in 1921, initiated a campaign to develop a vaccine during the height of the presence of poliomyelitis in the United States in 1953, This campaign was successful 2 years later in 1955 when Dr. Jonas Salk officially developed the first, inactivated, injectable polio vaccine²[10]. He did so by using the known technique of growing the virus in the kidney cells of monkeys, then isolating it and inactivating it with formaldehyde⁷[11]. In 1961, Dr. Albert Sabin developed an attenuated, live, oral vaccine.
In the pre-vaccination era, the three serotypes were relatively equal in their frequency. This indicates that it was not until the introduction of the OPV that the type 1 virus became the most widespread, the type 2 virus became no longer endemic, and the type 3 virus became intermediately distributed [7]. Serotype 2 of the poliovirus was declared globally eradicated in 1999.

The three serotypes
Include some current research in each topic, with at least one figure showing data.
Further Reading
[Sample link] Ebola Hemorrhagic Fever—Centers for Disease Control and Prevention, Special Pathogens Branch
References
Edited by (your name here), a student of Nora Sullivan in BIOL168L (Microbiology) in The Keck Science Department of the Claremont Colleges Spring 2014.
