Prevotella nigrescens

The mouth is the home of a diverse, abundant and complex microbial community. This highly diverse microflora community resides on the various surfaces of the normal mouth. Rather than a passive relationship with the host, these resident microflora play a positive role in normal development of the host. A dynamic equilibrium exists between the normal microflora and the innate host immune system. The host immune system is highly efficient and constantly monitors microflora levels in order to prevent these normally benign resident microflora from invading oral tissues. When certain microflora colonize and increase, they trigger an over-aggressive response from the immune system and increase the incidence of many diseases including but not limited to oral infections. One specific type of bacteria that is part of the normal oral flora but leads to disease when it infects the local tissue is Prevotella nigrescens. (Figure 1)
Prevotella nigrescens (P. nigrescens), a member of the Prevotella species found in normal oral flora, was first discovered within a group of bacteria termed Bacteroides intermedius.[1] The fact that there was heterogeneity within this species, Bacterioides intermedius, had been recognized for some time. This discrepancy led to further biochemical and chemical studies that revealed two serotypes within Bacterioides intermedius one of which was Prevotella intermedia. It was upon characterization of the newly discovered Prevotella intermedia that revealed yet another profile within this assumed homogenous species, which is what we now know as Prevotella nigrescens.
Studies focused on the characterization of these two distinct strains revealed that both P. intermedia and P. nigrescens play a role in the pathogenesis of periodontal disease. Periodontal disease is a synonym for periodontitis. Periodontitis is a set of inflammatory diseases affecting the tissue that surround and support teeth. P. nigrescens causes periodontitis by colonizing on the tooth surface and triggering an overly aggressive immune response, which is perceived as inflammation of oral tissue. More recently, P. nigrescens has also been found to be associated with signs of carotid atherosclerosis even in patients without periodontitis and with endodontic infections.[2] [3]
As more information on the pathogenesis properties of P. nigrescens was uncovered, there was a demand to find a treatment. Under this pressure a potential alternative treatment, to antibiotics, for P. nigrescens was found in the use of bee glue.[4]
Previous studies suggest that P. intermedia is more often found in periodontal sites whereas P. nigrescens is more frequently found in healthy gingivae. However, P. nigrescens have been implicated as a major periodontal pathogen as well. It is important to note the site specificity and pathogenicity of P. nigrescens remains unclear, suggesting that it is yet early to draw conclusions from the current findings.[3] [4] Overall, the majority of studies up to date show that there are increased levels of P. nigrescens in oral diseases and therefore implicating P. nigrescens as an oral pathogen but further research remains to be conducted to confirm these findings.
Discovery
P. nigrescens was initially assumed to be a genotype of P. intermedia.[1] P. intermedia (formerly Bacteroides intermedius) is a gram-negative, obligate anaerobic rod. It is often isolated from subgingival plaque of humans with periodontal disease and from other oral and non-oral infections.[18] [19] Studies previously showed that there were two different types of P. intermedia.[20] Since there was a suggested association between only one genotype of P. intermedia and periodontal disease, there was a strong need for reliable tests to differentiate between the two proposed species. Now we know that both P. intermedia and P. nigrescens are implicated in the pathogenesis of periodontitis. But at the time, the importance of differentiating between the two strains was for diagnosis purposes.
Differentiation from P. intermedia
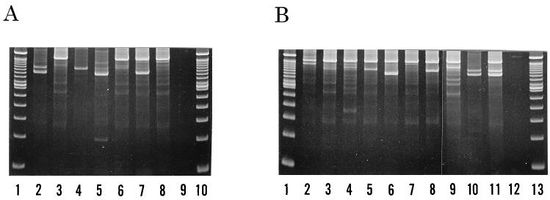
Identification of samples as either P. intermedia or P. nigrescens were made based on multilocus enzyme electrophoretic profiles, surface biotinylation, and PCR ribotyping to name a few assays. Sodium dodecyl-polyacrylamide gel electrophoresis (SDS-PAGE) of whole cell samples show that P. nigrescens have 31 and 38 kDa proteins that are not present in P. intermedia.[5]
In multiple studies, sodium dodecyl-polyacrylamide gel electrophoresis (SDS-PAGE) of whole cell samples showed that P. nigrescens have 31 and 38 kDa proteins that are not present in P. intermedia.[5] [22]
Multilocus enzyme electrophoresis is based on the principle that mutations in genes encoding bacterial metabolic enzymes can be detected by differences in electrophoretic migration patterns of the enzymes.[21] The use of malate dehydrogenase and glutamate dehydrogenase resulted in unambiguous separation of the two DNA, P. intermedia and P. nigrescens. P. nigrescens strains usually produced only one slowly migrating band while the P. intermedia strains produced either of two fast-migrating bands corresponding to the alleles coding for malate and glutamate dehydrogenase respectively.[22]
Further characterization by surface biotinylation of cells from P. nigrescens revealed that the 31 kDa protein, visualized on the SDS-PAGE, is on the surface of the protein. Although no further research has been done on the 38 kDa protein, this protein may be of further help to distinguish both species as it stained strongly only in P. nigrescens.
P. intermedia and P. nigrescens also differ in localization. P. nigrescens was almost three times more frequently isolated from infected root canals than P. intermedia.[3] This discovery emphasized the importance of differentiating between the two strains. Considering that the two strains of bacteria were found it is reasonable to say that they play different roles in the pathogenesis, if at all, of periodontitis.
However, identifying the two strains using methods such as SDS-PAGE, multilocus enzyme electrophoresis, ribotyping, and arbitrarily primer PCR (AP-PCR) are either time-consuming or have low levels of reproducibility. A recently developed method, PCR ribotyping, is expected to amplify the 16S and 23S spacer regions of bacterial rRNA genes by PCR.[6] [15] It generates simple banding patterns that allows comparison between separate PCR amplifications. Since PCR ribotyping amplicons smaller than 600bp were poorly reproduced, higher discriminatory assays were run by using a combination of PCR ribotyping and AP-PCR fingerprinting. The combination assay identified seven types within the P. intermedia strain and ten types within the P. nigrescens strain, all of which were differentiable by a combination of their band patterns and DNA fingerprints. (Figure 2)
In short, these results demonstrate unequivocally that strains previously placed in P. intermedia are actually members of two genetic groups.
Cellular morphology and biochemistry
P. nigrescens are black-pigmented Bacteroides that ferment carbohydrates. They are gram-negative, non-sporing, obligatory anaerobic, rod-shaped bacterium of the genus Prevotella that is commonly found in oral flora.
Since P. nigrescens are obligate anaerobes, all experiments involved in its characterization must be run under strictly anaerobic conditions. Cells grown in broth cultures are 0.3 to 0.7 µm wide by 1 to 2 µm. On agar, colonies are 0.5 to 2 mm in diameter, circular, low convex and smooth. On blood agar, the colonies are brown to black suggesting weakly hemolytic, and sometimes alpha-hemolytic, properties. Pigmentation is mainly towards the outer edges whereas the center remains creamy to dark brown. Strains grown on blood agar also exhibit red fluorescence under long-wave UV radiation (365nm).[1]
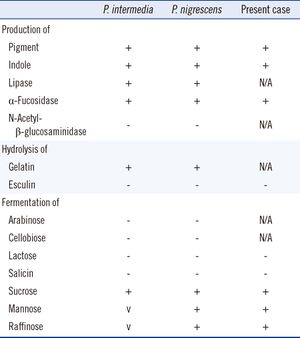
P. nigrescens uses mixed fermentation in anaerobic living conditions, breaking down dextrin, glucose, maltose, and sucrose. In the process of fermentation, they produce acetic, isobutryic, isovaleric, and succinic acids. Characterization using the API ZYM system revealed that P. nigrescens reacted with acid and alkaline phosphatases, phosphoamides, and β-glucosidases. The system showed weak reactions with butyrate esterase and caprylate esterase lipase. (Figure 3) The principal respiratory quinones are unsaturatedmenaquinones. The G+C content of the DNA is 40 to 44 mol%.[1]
Role in Disease
Periodontitis
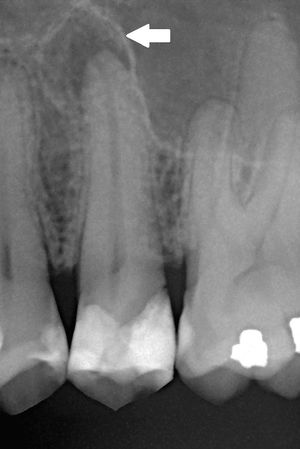
Periodontitis, or periodontal disease, is inflammation around the tooth. It is a serious gum infection that eventually leads to progressive loss of soft tissue and bone that supports the tooth if left untreated. (Figure 4) Microorganisms, such as P. nigrescens, adhere to the surface of the tooth and multiply. They then trigger the immune system, which leads to the syndromes such as inflammation and bleeding of the gums. Studies suggest that the root of P. nigrescens pathogenicity lies in that it seems to promote the release of inflammatory mediators.[10] [11]
P. nigrescens is part of the orange complex that forms in subgingival and supragingival plaque. The orange complex is a network of a few specific species of bacteria (Eubacterium nodatum, Peptostreptococcus micros, species from the genera Fusobacterium, Prevotella, and Campylobacter) in dental plaque that exist in communities of enclosed matrix relating to one another in a specific fashion. The purpose of forming these communities is to promote growth and survival of the bacteria. There are four different complexes: red, orange, yellow and green. Formation of each complex is associated with a stage of periodontal condition. For instance, members of the orange complex are associated with gingivitis and presence of gingival bleeding. The red complex is the last to colonize out of the four and is associated with chronic periodontitis such that it is the most commonly used periodontal diagnosis by testing for elevated levels of members of the complex.[7] Gingivitis usually refers to gum inflammation while periodontitis refers to gum disease. As such P. nigrescens is strongly related to bacteria of the red complex, which is the most commonly used periodontal diagnosis by testing for elevated levels of members of the complex. Therefore P. nigrescens are considered periodontal pathogens.[8] Much evidence supporting its pathogenic role comes from quantitative cultural studies, which is the comparison of certain pathogen levels in diseased sites to healthy sites.[9]
In a recent quantitative cultural study, it was discovered that P. nigrescens is found more frequently in subgingival plaque of patients with periodontitis than in the subgingivae of healthy patients.[1] These subgingival sites were classified as either active, inactive or healthy using a number of widely accepted clinical criteria such as probing depth, bleeding on probing and or pus.[9] Researchers found a correlation between increased colonization of P. nigrescens and periodontitis.[1] Another group found that up to 70% of patients with localized and generalized forms of onset periodontitis had detectable levels of P. nigrescens in their subgingival plaque, further confirming the correlation between P. nigrescens and periodontitis.[11]
However, more research needs to be conducted in order to truly accept P. nigrescens as a putative periodontal pathogen for periodontal disease. Contradictory data showed that 9 of 21 subjects (15 periodontitis patients and 6 healthy volunteers) harbored more than one genotype of P. nigrescens. Several different types were found occupying different sites around the same tooth.[9] This data seems to suggest that no specific relationship existed between disease status and colonization of same or different types of P. nigrescens. The reliability of this data should be carefully considered as the selected cohort is on the smaller side.
Carotid atherosclerosis
Carotid atherosclerosis is also known as arteriosclerotic vascular disease. It is marked by the thick of artery walls in the heart, which is a result of invasion and accumulation of white blood cells. However, the developmental process of this disease is not well studied. It has been suggested that inflammatory processes in the endothelial cells of the vessel walls initiate the onset of disease.[13] Diagnosis involves ultrasound scanning and calculated intima media area (cIMA) measurements.
Several studies published in the past two decades have implicated oral diseases, periodontitis in particular, as risk factors for the development of cardiovascular diseases.[2] Cardiovascular disease (CVD) is a class of disease that involves the heart or blood vessels. A few examples of CVD include coronary thrombosis, stroke and atherosclerosis. The way through which periodontitis contributes is by increasing the systemic inflammatory burden and pathogenic processes that are known to lead to atherosclerosis.[14] More recently, a direct association was established between the localization of P. nigrescens in the oral cavity and atherosclerosis.[2]
P. nigrescens is characterized as a periodontal pathogen. It contributes to the infection and inflammation of periodontal tissue. However, periodontal pathogens alone are not sufficient in the pathogenesis of periodontitis so P. nigrescens has been observed in healthy oral flora. One explanation for the unexpected presence of P. nigrescens in healthy flora may be that pathogenesis has not occurred yet, but the presence of P. nigrescens foreshadows the onset of disease. In support of this explanation, a recent study showed an association of increased cIMA with the presence of P. nigrescens.[2] In this case it was hypothesized that the atherosclerosis development is due to P. nigrescens being released from periodontal lesions into circulation. There, it affects the arterial wall by virulence compounds (such as lipopolysaccharides), invades epithelial cells, inducing mechanisms that are detrimental to the host cells and thus causing an accumulation of white blood cells leading ultimately to carotid atherosclerosis.[2]
Treatment
P. nigrescens and its role in periodontitis were discovered relatively recently thus the majority of current treatments for periodontitis are not targeted towards P. nigrescens. P. nigrescens is a promising target, however, and ongoing research is investigating the merits of treatments revolving around it.

Bee Glue
The development of new therapies for treatment of oral cavity diseases is of great importance since the development of antibiotic resistance of certain microbes. One of these new treatments that have emerged is the use of propolis, more commonly known as bee glue.[4] (Figure 5)
The biological activities of bee glue include antibacterial, anti-fungal, anti-protozoan, antiviral, anti-tumoral, immunomodulation, anti-inflammatory and other therapeutic properties.[4] Currently, studies show some types of propolis are effective in treating gum infections and therefore inflammations due to P. nigrescens. Penicillin G, erythromycin, meropenem, metronidazole and tetracycline were found to inhibit 90% of the growth (MIC90) of P. intermedia and P. nigrescens strains at of 0.06, 0.13, 2.0, 4.0 and 4.0ug/mL respectively. P. intermedia and P. nigrescens were found to be susceptible to three ethanolic extract of propolis at 128ug/mL.[4] Preliminary studies have shown that propolis has active constituents including flavonoids that give it anti-inflammatory properties. Flavonoids are a class of plant secondary metabolites that have been proposed to have anti-inflammatory mechanisms including modulation of the arachidonic acid pathway, inhibition of gene transcription, protein expression and activity of inflammatory enzymes, as well as secretion of anti-inflammatory mediators.[16] Other active constituents found in bee glue also have properties that inhibit cell proliferation.
Propolis shows great promise as a non-invasive and natural treatment for gum disease. The Nation Institutes of Health rates propolis as "possibly" effective for treating certain conditions. However, gum disease does not yet fall under the umbrella of the conditions mentioned by the NIH. There is currently insufficient evidence to rate the consistency and effectiveness of propolis in treating gum disease due to colonization of P. nigrescens.[17]
Future directions
Majority of evidence suggests that P. nigrescens is periodontal pathogen. However, there is still contradictory data showing the presence of P. nigrescens in healthy oral flora. It is of significant importance to establish a cause-and-effect relationship between P. nigrescens and periodontitis so that it can be used as a marker for gum disease through more rigorous and long-term research.
Currently there is a disconnect between oral health and general health. The mouth is the gateway to the body and therefore is essential to good overall health. Data shows that there is a direct connection between the health of the mouth and that of the heart. This connection can change the way we diagnose heart disease and plan treatments. If P. nigrescens can be proven to be associated with periodontitis, which has already been shown to correlate to heart disease, then it could potentially be used as a diagnosis tool for heart disease. Microorganisms in the mouth such as P. nigrescens can also serve as a target for heart disease. The first step to achieving these goals, however, lies in raising awareness for the link between the mouth and heart.
References
1. Shah HN, Gharbia SE (1992). Biochemical and chemical studies on strains designated Prevotella intermedia and proposal of a new pigmented species, Prevotella nigrescens sp. nov. Int J Syst Bacteriol 42: 542–6.
2. Yakob M., Söder B., Meurman J. H., Jogestrand T., Nowak J., Söder P.-Ö. (2011). Prevotella nigrescens and Porphyromonas gingivalis are associated with signs of carotid atherosclerosis in subjects with and without periodontitis. Journal of Periodontal Research 46 (6): 749–755.
3. Saheer E.G, Markus H, Haroun N.S, Anja K, Kari L, Michelle A. P., Deirdre A. D. (1994) Characterization of Prevotella intermedia and Prevotella nigrescens Isolates From Periodontic and Endodontic Infections. Journal of Periodontology 65(1): 56-61
4. Santos, F. A., Bastos, E. M. A., Rodrigues, P. H., de Uzeda, M., de Carvalho, M. A. R., de Macedo Farias, L., Moreira, E. S. A. (2002). Susceptibility of Prevotella intermedia/Prevotella nigrescens (and Porphyromonas gingivalis) to propolis (bee glue) and other antimicrobial agents. Anaerobe, 8(1), 9-15.
5. Fernández-Canigia L, Cejas D, Gutkind G, Radice M. (2015) Detection and genetic characterization of β-lactamases in Prevotella intermedia and Prevotella nigrescens isolated from oral cavity infections and peritonsillar abscesses. Anaerobe. 2015 Jan 23;33C:8-13.
6. Fukui K, Kato N, Kato H, Watanabe K, Tatematsu N (1999). Incidence of Prevotella intermedia and Prevotella nigrescens carriage among family members with subclinical periodontal disease. Journal of Clinical Microbiology 37 (10): 3141–5.
7. Newman , M.G (2011). Carranza's Clinical Periodontology, 11th Edition. Saunders Book Company: p.245
8. Stingu C.S., Schaumann R., Jentsch H., Eschrich K., Brosteanu O., Rodloff A.C (2013). Association of periodontitis with increased colonization by Prevotella nigrescens. Journal of Investigative and Clinical Dentistry 4 (1): 20–25.
9. Teanpaisan R, Douglas CW, Eley AR, Walsh TF (1996) Clonality of Porphyromonas gingivalis, Prevotella intermedia and Prevotella nigrescens isolated from periodontally diseased and healthy sites. Journal of Periodontal Research 31(6): 423-432
10. Mullally BH, Dace B, Shelburne CE, Wolff LF, Coulter WA. (2000) Prevalence of periodontal pathogens in localized and generalized forms of early-onset periodontitis. J Periodontal Res 35: 232–41.
11. Kikkert R, Laine ML, Aarden LA, van Winkelhoff AJ (2007). Activation of toll-like receptors 2 and 4 by Gram negative periodontal bacteria. Oral Microbiol Immunol 22: 145–51.
12. Airila-Mansson S, Soder B, Kari K, Meurman JH (2006). Influence of combinations of bacteria on the levels of prostaglandin E2, interleukin-1ß, and granulocyte elastase in gingival crevicular fluid and on the severity of periodontal disease. J Periodontol 77: 1025–31.
13. Williams KJ, Tabas, I (1995) The Response-to-Retention Hypothesis of Early Atherogenesis Arteriosclerosis, thrombosis, and vascular biology 15 (5): 551–61.
14. Tonetti Ms (2009) Periodontitis and risk for atherosclerosis: an update on intervention trials J Clin Periodontol 36: 15-19.
15. Yang JJ, Kwon TY, Seo MJ, Nam YS, Han CS, Lee HJ. (2013) 16S Ribosomal RNA Identification of Prevotella nigrescens from a Case of Cellulitis. Ann Lab Med 3(5):379-382.
16. Martinez-Micaelo N, González-Abuín N, Ardèvol A, Pinent M, Blay MT (2012). Procyanidins and inflammation: Molecular targets and health implications. BioFactors 38 (4): 257–265.
17. Propolis:MedlinePlus Supplements. U.S. National Library of Medicine. (2012)
18. Haffajee, A. D., and S. S. Socransky (1994) Microbial etiological agents of destructive periodontal diseases. Periodontology 2000 5:78-111.
19. Moore, W. E. C., and L. V. H. Moore (1994) The bacteria of periodontal diseases. Periodontology 2000 5: 66-77.
20. Johnson, J. L., and L. V. Holdeman (1983) Bacteroides intermedius comb. nov. and descriptions of Bucteroides corporis sp. nov. and Bacteroides levii sp. nov. Int. J. Syst. Bacteriol. 33:15-25.
21. Selander RK, Caugant DA, Ochman H, Musser JM, Gilmour MN, Whittam TS (1986) Methods of multilocus enzyme electrophoresis for bacterial population genetics and systematics. Appl Environ Microbiol. 51(5):873-84.
22. Frandsen, E.V., Poulsen, K., Kilian, M (1995) Confirmation of the species Prevotella intermedia and Prevotella nigrescens. 45(3):429-35
Edited by Nancy Zhu, a student of Suzanne Kern in BIOL168L (Microbiology) in The Keck Science Department of the Claremont Colleges Spring 2015.
