Tea Tree Oil Treatment of MRSA
Methicillin-resistant Staphyloccocus aureus (MRSA) is a public health problem. The prevalence of MRSA as a pathogen in hospitals and other community settings underscores the importance of eradicating the carriers. As MRSA is not susceptible to commonly used antibiotics, alternative antimicrobial agents are being sought for its eradication. One area of interest involves the use of plant essential oils. Studies indicate the effectiveness of tea tree oil as a treatment for infections of drug-resistant bacteria, including MRSA.
Introduction
Staphyloccocus aureus, more commonly known as staph bacteria or MRSA, is a Gram-positive coccus-shaped anaerobic bacterium pictured in Figure 1.1 MRSA is a type of staph bacteria that is resistant to beta-lactam antibiotics, such as penicillin, amoxicillin, oxacillin, and methicillin. MRSA often colonizes on the skin or nostrils of healthy individuals, and is relatively harmless at these sites.1 If S. aureus enters the body (e.g., wounds, cuts), it may cause infections. In such instances, the MRSA infection may range from mild (e.g., pimples) to life-threatening (e.g., infection of bloodstream, joints, or bones). MRSA is spread through contact and most commonly contracted in public settings, namely hospitals.
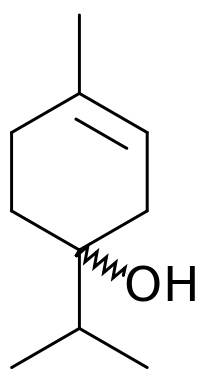
Tea tree oil (TTO) is the essential oil derived through steam distillation from the Australian native plant Melaleuca alternifolia. Tea tree oil has been used for centuries as a topical antiseptic. TTO is believed to have antibacterial, antifungal, antiviral, and anti-inflammatory properties.2 Although historical anecdotes endorse TTO's medicinal properties, few clinical studies have been conducted to support such claims. Clinical studies, however few, indicate that tea tree oil can treat the skin infection caused by MRSA. Tea tree oil's anti-microbial properties are attributed to its composition of a chemical class known as terpenes, specifically terpinen-4-ol.2 Tea tree oil's bacteriocidal and bacteriostatic effects make this plant extract a plausible addition or supplement to a MRSA treatment plan.
Tea Tree Oil Composition and Chemistry
Commercially available tea tree oil (TTO) is a composition of nearly 100 chemical compounds determined by gas chromatography-mass spectrometry.1 TTO is primarily composed of a class of chemicals called terpenes. Specifically, monoterpenes, sesquiterpenes, and other terpene alcohols dominate this composition. Terpenes are volatile, aromatic hydrocarbons and are typically soluble with nonpolar solvents.2 While research indicates that terpene alcohols are generally effective anti-microbial agents, terpinen-4-ol is the specific terpenic compound believed primarily responsible for TTO's anti-microbial activity.2
TTO composition is internationally regulated and may be commercially available in various chemotypes, including the terpinen-4-ol chemotype where terpinen-4-ol comprises between 30 to 40% of TTO's commercial composition.2 International regulation of TTO's chemical properties calls for this relatively high composition of terpinen-4-ol in commercial production due to its historical medicinal properties. Other terpenic compounds in TTO include 1,8-cineole, terpinolene, and α-terpineol.3 These compounds also have medicinal properties that are less reputable than those of terpinen-4-ol.
Treatment and Effectiveness
Efforts to validate the therapeutic properties of tea tree oil (TTO) have yielded in vitro (i.e. laboratory) and clinical studies with results showing eradicated and reduced MRSA infection, respectively. The demonstrated effectiveness of TTO treatment after infection has led to preliminary research regarding TTO application as a way to prevent MRSA infection. While TTO displays in vitro and clinical efficiency, TTO has not been demonstrated to prevent initial MRSA colonization. These studies support the claims upheld by traditional healers that TTO is an effective antimicrobial agent.
In Vitro Treatment
The efficacy of tea tree oil (TTO) against MRSA has been demonstrated in laboratory studies using cultured S. aureus samples. One in vitro study by May et al. showed that MRSA was eradicated after 6 hours of continuous exposure to 5% TTO. These results imply that TTO is able to eradicate MRSA and has strong health implications for clinical usage.
May et al. conducted in vitro experiments to explore the TTO's bactericidal activity in laboratory-grown cultures of MRSA.citation To the MRSA culture, standard TTO was added to a final concentration of 5%, which is the typical TTO concentration found in commercial products. The MRSA culture was inoculated for 6 hours with 5% TTO. Colony counts were performed throughout this period to determine if TTO had killed any colonies. May found that 99.9% of the MRSA isolate was killed by 4 hours and that all was killed by 6 hours.citation This finding demonstrates TTO's potency against MRSA and suggests that TTO's antimicrobial properties make this a good agent to control MRSA and reduce its transmission among humans.
Clinical Treatment
The demonstrated efficiency of TTO in eradicating laboratory isolated MRSA cultures led to clinical testing with human patients using products enhanced with TTO.
TTO may be added to commercial products, such as body wash, skin cream, and nasal ointment due to its antimicrobial properties. Such products can be incorporated into a daily regimen to treat MRSA. The clinical efficacy of TTO body wash and creams as a decolonization agent for MRSA has been supported by Caelli et al. and Dryden et al.. TTO treatment has been demonstrated by both researchers to be at least as effective as the conventional treatment regimen against MRSA infection. These studies indicate that inclusion of TTO treatment may enhance a MRSA eradication regimen.
Caelli et al. compared the effectiveness of TTO treatment to that of standard treatments against MRSA, as measured by post-treatment MRSA concentrations on the skin and within the nose.4 In their clinical study, 30 MRSA-infected adult hospital inpatients were randomly assigned to receive either the standard treatment (2% antibiotic nasal ointment and triclosan body wash) or tea tree oil regimen (4% TTO nasal ointment and 5% TTO body wash) for three days. Compared to the standard treatment, the tea tree oil topical regimen reduced or eradicated MRSA infection in more subjects. Despite this optimistic finding, the small sample size prevented this result from being statistically significant. In conclusion, Caelli suggested that TTO treatment was just as effective at eradicating MRSA as the standard medical treatment.
Dryden et al. conducted a similar study regarding TTO's effectiveness against MRSA-related skin infection.6 Dryden's clinical study, which involved 236 MRSA patients, found that tea tree soaps and creams cleared MRSA from superficial skin sites and wounds in more patients than the standard skin treatment of chlorhexidine or silver sulphadiazine.6 They found that the daily application of 5% TTO body wash and 10% TTO cream was more effective than standard treatment at clearing skin lesions and variations in skin texture or color associated with MRSA infection, but did not eradicate the MRSA infection entirely. Of note, they also deemed TTO to be sufficiently effective, safe, and well-tolerated to be considered part of a MRSA eradication regimen.
Although research suggests the efficacy of TTO against MRSA, more clinical studies would have to be performed in order to comprehensively assess TTO's effects on MRSA patients.
Prevention
The promising research regarding TTO's ability to eradicate MRSA from infected individuals prompted investigation of TTO application as a means of preventing MRSA. Since TTO was found to effectively treat patients after the onset of MRSA infection, researchers wanted to find out whether regular TTO application could prevent MRSA colonization in individuals with no prior MRSA colonization or infection.
Research by Blackwood et al. indicates that, although TTO is an effective medical treatment after MRSA infection, daily TTO application does not prevent new MRSA colonization.5 Since MRSA colonization, which may lead to life-threatening infection, is more probable in well-populated settings among individuals with weak immune systems, Blackwood's key study was conducted with 391 critically ill adults belonging to two intensive care units (ICU).5 These patients had no history of MRSA colonization. Blackwood sought to determine whether the daily use of either TTO body wash or Johnson's Baby Softwash (standard care) had a lower incidence of MRSA colonization. A randomized regimen of either standard care body wash or TTO (5%) body wash was assigned to each patient. Patients continued treatment until they reached one of the study endpoints: detection of hospital-acquired MRSA, ICU discharge, or death. Blackwood reported that the TTO regimen did not significantly reduce new MRSA colonization in ICU patients. The researchers could not recommend TTO body wash as a means of MRSA prevention. These findings indicate that TTO's most beneficial clinical use lie in its ability to eliminate MRSA after infection.
Antimicrobial Activity: Cytoplasmic Membrane Damage
The target of TTO's antimicrobial activity, and the primary reason for its laboratory and clinical effectiveness, is reported to be the S. aureus cell membrane. The bacterial cell membrane, which physically separates the cell's internal environment from the external environment, is selectively permeable to organic molecules and ions and regulates the movement of water and other substances in and out of the cell.7 The researchers Cox et al and Carson et al, who examined the cytoplasmic membrane damage caused by TTO, proposed that TTO compromises the cell membrane permeability and osmoregulation, thus resulting in cell lysis, or lethality.
Cox et al found that exposure of MRSA to the minimum inhibitory concentration (MIC) of TTO altered cell membrane structure.7 The MIC is the lowest concentration of antimicrobial - in this case, TTO - that will inhibit microbial growth. Cox accumulated evidence of cell membrane damage from a propidium iodide uptake assay and potassium ion leakage measurements. As expected, cells that were not exposed to TTO displayed an intact cell membrane. Propidium iodide, a fluorescent nucleic acid staining solution, did not penetrate cells that were not exposed to TTO. Likewise, cells not exposed to TTO showed little potassium ion leakage. Essentially, physiologically normal S. aureus cells would not uptake propidium iodide or leak potassium ions.
From the experiment, Cox et al found that TTO exposure resulted in propidium iodide uptake and potassium ion leakage, signs of a damaged cytoplasmic membrane.7 In particular, they observed that exposing cell suspensions of MRSA to the minimal inhibitory concentration of 0.25% (v/v) tea tree oil for 30 minutes increased cell permeability to propidium iodide relative to the controls. They also demonstrated that 30 minutes of exposure to TTO caused up to 20% cellular loss of potassium ions. They proposed that TTO components diffused through the cell wall and disrupted the phospholipid regions of cell membrane structures. The ensuing passage of propidium iodide and potassium ions indicated severe cytoplasmic membrane damage.
Carson, C. et al demonstrated cytoplasmic membrane damage through increased susceptibility to NaCl, loss of cytoplasmic material, and the formation of mesosomes (i.e. abnormal invaginations of the cell membrane) in MRSA that was treated by TTO or one of its components: terpinen-4-ol, α-terpineol, 1,8-cineole.8 MRSA cells treated with TTO or its components were found to be more susceptible to salt solution or sodium chloride (NaCl), a bacterial cell toxin. This evidence led Carson et al to propose that the treatment compromised the S. aureus cell membrane's ability to exclude NaCl. Electron microscopy of MRSA cells treated with terpinen-4-ol showed mesosome formation that was not observed in untreated cells. Mesosomes, invaginations of the cytoplasmic membrane, along with loss of cytoplasmic material, suggested that the TTO and its components compromised the S. aureus membrane.
Both Cox et al and Carson et al performed different experiments to demonstrate TTO's devastating effect on the S. aureus cytoplasmic membrane. While much of TTO's mechanism remains unexplored, these studies indicate that TTO targets the cytoplasmic membrane.
Susceptibility to Antibiotic Resistance after TTO Exposure
There is concern that commercial TTO preparations, which may vary in its components' concentrations, provide users more opportunity to apply sub-lethal concentrations and lead to reduced antimicrobial susceptibility. McMahon et al and McMahon et al (2008) suggest that exposure of MRSA to sub-lethal TTO concentrations, defined as half of the minimal inhibitory concentration (MIC), makes MRSA less susceptible to antibiotics.9, 10 Recent research indicates otherwise. Hammer et al and Thomsen et al suggest that while the MIC for antibiotics might increase post-TTO habituation, such results are statistically not significant.11, 12 They allege that habitation of MRSA in sub-lethal TTO concentration does not significantly reduce its susceptibility to antibiotics.
Two studies by the McMahon Lab suggested that exposure of MRSA to sub-lethal concentration of TTO was associated with decreased susceptibility to antibiotics.9, 10 McMahon et al supported these claims by demonstrating that the effective MIC of TTO-habituated MRSA for 7 out of 10 tested antibiotics increased at least 2-fold from the baseline after a 72 h habituation to sub-lethal TTO concentrations. They suggested that, even though TTO was an effective treatment for MRSA at relatively low concentrations (0.25%-0.50%), repeated TTO use at sub-lethal concentrations could reduce susceptibility to antibiotics.
Hammer et al and Thomsen et al later performed a similar investigation, but reported a different outcome. Despite using similar parameters as in the McMahon Lab's experiments, they were unable to reproduce the published results.11, 12 Instead, they found minor increases and decreases in MIC after TTO habituation. Hammer et al and Thomsen et al disputed the McMahon Lab's results and strongly claimed that tea tree oil did not induce resistance to itself or other antimicrobials.
Conclusion
Discovering alternative therapy for the treatment of MRSA is very important as antibiotic resistance becomes more prevalent. MRSA's increasing resistance to mupirocin, the primary antibiotic in standard MRSA eradication treatments, has been noted by Dryden.6 Since TTO shows no sign of inducing antibiotic susceptibility in MRSA upon treatment, one alternative treatment is the use of tea tree oil as an antimicrobial.
TTO's chemical composition of terpenic derivatives contributes to its antimicrobial activity. Its primary terpenic component, terpinen-4-ol, has been investigated as an antimicrobial agent.2 Carson, C. et al also demonstrated the antimicrobial activity of 1,8-cineole and α-terpineol, two other terpenic derivatives found in TTO.4
A TTO regimen has been found to be at least as effective as standard MRSA treatment in eradicating MRSA. This is grounds for supplementing a MRSA treatment plan with TTO product, such as body wash, nasal ointment, or skin cream.
The mechanism of TTO's cidal effects is reported to damage the S. aureus cytoplasmic membrane, thus allowing for the unnatural passage of substances.
Exposure to sub-lethal concentrations of TTO has also been reported to increase resistance to antibiotics.9, 10 However, these results have been disputed and requires further investigation.11, 12
Current research focuses on TTO's mechanism of action, safety, and effect on antimicrobial susceptibility. Though cytoplasmic membrane damage is believed to be the major bactericidal effect, the mechanism is still largely unexplored. Other research examines commercial tea tree oil's cytotoxicity if applied topically to human skin.citation Such investigation would determine the safety of applying TTO on a regular basis and hopefully, the optimal strength of tea tree oil for MRSA eradication. Ongoing research also investigates whether or not exposure to sub-inhibitory concentrations of TTO will lead to reduced antimicrobial susceptibility.
References
1. National Health Service (NHS). "MRSA Infection" NHS Choices 23/09/2011 Published. Web. 21/03/2013 Accessed. <http://www.nhs.uk/conditions/MRSA/Pages/Introduction.aspx>
Edited by Karen Leung, a student of Nora Sullivan in BIOL187S (Microbial Life) in The Keck Science Department of the Claremont Colleges Spring 2013.