The Human Gut
By Mia Tran
Overview
The human gut, also known as the gastrointestinal (GI) tract, consisting of all the organs that allow for humans to consume, digest, and expel food, and is highly populated by a diverse range of microbiota that serves many crucial processes in maintaining human health, such as digestion, fighting infection, and production of key vitamins and antioxidants.[1] The microbes occupying the gut ranges to the order of 1017[2] and consists primarily of bacteria, but also includes a variety of protozoa, archaea, prokaryotes, and viruses.[3]
Description of Physical and Biogeochemical Environment
The physical environment of the GI tract consists of an interface ranging from 250-400 square meters in an adult human.[4] The distribution of microbiota within this interface depends greatly on various gradients existing in the gut, such as nutrient and chemical gradients.[4] Microbes tend to sit either in the lumen or mucosa, and very rarely penetrates the bowel wall, as most microbes that achieve this tend to be pathogenic.[1]
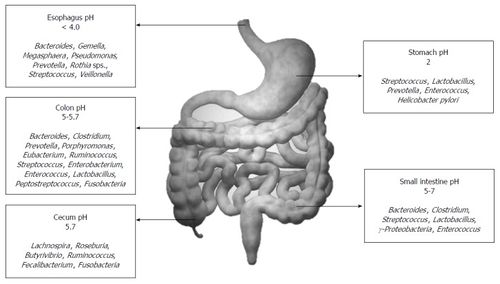
The biogeochemical landscape of the gut various from organ to organ. The small intestine, the first organ in the tract following the stomach, is characterized by low pH, high oxygen, and an abundance of antimicrobials.[4] These conditions allow for limiting microbe growth, just so facultative anaerobes begin to settle to the mucus lining of the intestine, making way for an environment conducive for obligate anaerobes.[4] In the colon, or large intestine, there is a much more densely populated and diverse microbiota.[4] Communities of bacteroides, streptococci, and clostridia can outnumber facultative anaerobes up to a ratio of 1000:1.[1] The pH gradient and corresponding microbial communities are summarized in the figure to the right.[5]
Overview of History and Microbial Ecology
Leading up to the formal study of the gut microbiota, breakthroughs in culturing anaerobes in 1944[6] and using a faecal transplant to treat a Clostridioides difficile infection in 1958[7] were some first breakthroughs in the field. The study of microflora in the human gut formally began in 1960s, where much of the initial research began with experiments using germ-free animals,[8] and studying the composition and count of microbes.[2] At the time, most of the work being done focused on strains that could be cultured. With technological developments in sequencing, scientists in the 1990s were able to identify and classify the makeup of the human microbiota more accurately than they were before when culture was the only method of exploration.[4][9] Since then, research exploded during the 2000s and 2010s due to the development of "omics" technology that allowed scientists to learn about communities that could not be cultured in the lab.[10]
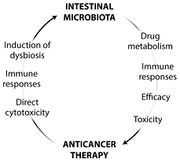
Current research centers around pushing these "omics" methods and applying knowledge of the gut microbiome to human health.[11] As of late, cancer related research shows that the composition of gut microbiota can affect the efficacy of certain cancer treatments, and vice versa.[12] This bidirectional relationship is summarized in the figure to the left.[12] Much research has been conducted on how to manipulate the gut microbiota to aid in cancer therapy.[11]
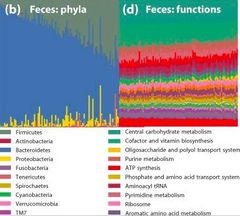
When examining the diversity of the human GI tract from culture based techniques, it was thought that all adult humans share a common “core” microbiota. However, with developments beyond culture-based studies, it has been revealed that the human microbiome is so diverse across populations and times that the concept of a core ceases to exist.[13] In the average human stool sample, up to 400 species can be found, giving a rough estimate at species richness.[1] Despite extensive species diversity between individuals over space and time, there was significant functional redundancy between parts of the GI tract. This means that there are quite similar functional profiles across individuals, showcased in the figure to the right.[13]
Acquisition of the Gut Microbiome at Birth and Infancy
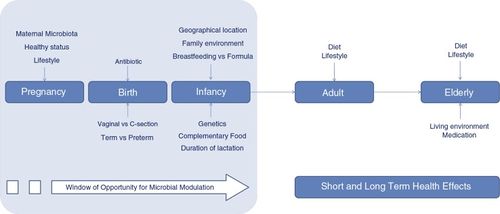
An individual's gut microbiome is first acquired at birth, not before. Babies are sterile within the womb, but at the moment of birth are exposed to bacteria from placenta tissue, umbilical blood, amniotic fluid, skin, and other membranes.[14] Natural and cesarean births can have different impacts on the acquired microbiome of the babies, as infants delivered vaginally will pick up microbes from the mother's vagina, and infants delivered through cesarean section will acquire microbes common to the mother's skin.[15]
After birth, the composition of microbiota is quickly changing and developing.[15] The infant's diet of breastmilk or formula, as well as various environmental factors can shift the communities in its gut during the first few years of life. It is common for there to be initially low diversity, as the Proteobacteria and Actinobacteria phyla dominate, and facultative anaerobes populate the infant gut to shape the environment for other anaerobes. As the child matures, usually after the first year, the gut experiences higher diversity dominated by the phyla Firmicutes and Bacteroidetes.[14]
Factors Changing the Composition of Gut Microbiota During Adulthood
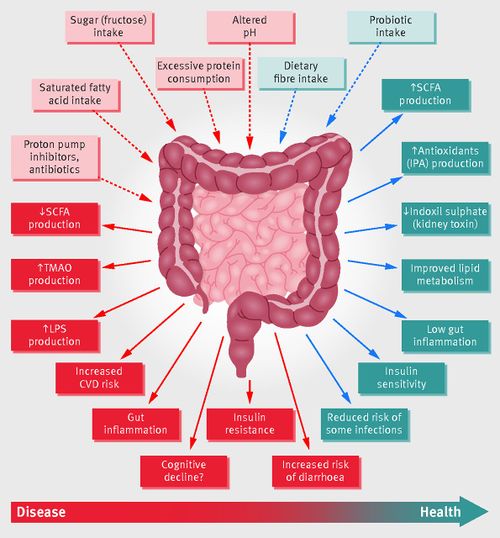
A number of factors can influence the composition of gut microbiota in an adult. The most influential is diet; studies examining factors such as location or seasonality usually will lead back to diet altering the gut microbiome. Adults with diets rich in fruits, vegetables, and fiber were found to have more diverse microbiomes.[5] The use of antibiotics has also shown to have potential effects on the GI tract's microbiome. Antibiotics can affect the gut in the short and long term; since the gut microbiome is quite resilient, short term use of antibiotics can wipe out some microbial populations, but some individuals are able to recover quickly. However, in some individuals, we can see that even short term use can alter diversity and population proportions for up to years afterwards.[5][16] Studies on germ free mice have shown a correlation between antibiotic treatments to incidence of type 1 diabetes, and in children a positive correlation between exposure to antibiotics and the development of asthma later in life; this indicates that antibiotics may impact gut communities so extensively, it affects the immune system significantly enough for long-term health conditions like diabetes and asthma to occur.[16]
Use of probiotics and prebiotics, which are small doses of microorganisms that can benefit health and supplementary nutrients, respectively, are thought to add to communities that are considered "good" microbes.[5] Though many of these products have been readily available to the general public, further research should be conducted to confirm the real effectiveness of using probiotics.[5][13] Finally, studies between adult monozygotic and dizygotic twins show that they have equally similar microbiomes, indicating the influence of the general environment of upbringing rather than genetics can be attributed to microbial makeup.[13]
Dysbiosis: Health Impacts of Disrupted Microflora
A healthy gut microbiota can look different among different individuals. Major shifts in the composition of communities in one individual is known a dysbiosis, which is a condition that can lead to various types of health issues.[17] There exists much literature on bacterial communities, but the spotlight has recently gone to fungi, viruses, and archaea.[17] One of those most studied health impacts due to dysbiosis is obesity; studies of germ free mice shows that transplants of microbes from obese mice show a lack of expression of genes that encode for leptin, a hormones that inhibits hunger.[18] Obese people have been found to have an increased amount of Firmicutes and decreased populations of Bacteroides.[19] As described in earlier sections, other immune-related health problems such as asthma, diabetes, and allergies have links to imbalances in the human GI tract microbiome.[18]
Another major health problem that may arise from dysbiosis is IBS (inflammatory bowel syndrome) and Crohn's disease, which are intestinal disorders directly linked to the gut microbiome. This is a result of a general decrease in microbial populations within the gut, as well as a change in composition due to decreases in Firmucutes, increases in Bacteroids, and increases in facultative anaerobes.[18] Interestingly, there have also been connections between dysbiosis of the gut microbiota to certain mental disorders, such as depression and anxiety. Studies have shown that patients diagnosed with major depressive disorder produced stool samples with increased levels of Bacteroides, Protobacteria, and Actinobacteria, and lowered Firmicutes populations, while patients diagnosed with generalized anxiety disorder show reduced populations of five genera.[20] These findings demonstrate a relationship between gut inflammation and increased immune system activity as a response to stress response.[18][20]
Key Microbial Players
As mentioned before, the majority of the microbes in the human gut are bacteria belonging to the Firmicutes and Bacteroidetes phyla. Other prominent groups include Actinobacteria, Proteobacteria, and Verrucomicrobia,[21] as well as methanogenic archaea, yeasts, a phages.[17] A majority of the bacteria cannot be cultured, which is why the development of technologies, such as 16S RNA sequencing, has allowed the scientific community to unlock more about the composition of the gut microflora.[21] It is important to note the discrepancies between culture and omics based research; much of the holistic understanding of the gut microbiota comes from more recent sequencing attempts.[21]
These key microbial players in the context of human gut environments can be grouped into enterotypes, which serve to divide and categorize humans by the primary composition of their gut microbiome, but are controversial due to discrepancies in methodology and results.[22] Initially, three primary groups were created: Bacteroides, Prevotella, and Ruminococcus. However, new research suggests that the Ruminococcus enterotype should grouped under Bacteroides.[22] Outside of the gut, Bacteroides can be pathological, but inside the gut they mediate carbohydrate metabolism. This enterotype is thought to be related to more animal-based foods and diets.[23] Prevotella is related to Bacteroides in the colon, and outside of the human gut commonly populates the rumen of cattle and sheep.[24] They function to break down plant cell walls as well as various proteins and peptides, and the enterotype relates to plant-based diets.[23]
Within the gut, these microbes as a collective are able to perform a variety of functions crucial to the human body. As described above, they largely function in general nutrient digestion; various populations can break down carbohydrates, proteins, and lipids, as well as complex molecules like fiber.[5][23] Enterohepatic circulation is mediated by these communities, which moves substances from the liver to bile, to the small intestine for absorption, then back to the liver; this overall serves the purpose of aiding digestion and absorption of substances like drugs and important acids.[1][23] Some key molecules, such as vitamins, can be secreted by certain strains of bacteria.[5] Additionally low levels of harmful bacteria, such as Clostridium difficile, can serve as an antimicrobial defense mechanism against foreign pathogens entering the GI tract, preventing infections.[1] Finally, there is increasing evidence that the some microbes in the gut can induce production of certain proteins and molecules that maintain the physical integrity of the organs within the GI tract.[5]
Conclusion
The human gut microbiome is a complex and reactive ecosystem that has quickly come to the attention of the scientific community for its close relationship in maintaining human health. The gut's microbial community is initially obtained and developed during birth and infancy, and affected over time through diet and environment. Though there is great species diversity within an individual and across populations, the human gut microbiome at large has functional redundancy, ensuring that all humans are able to digest foods, process drugs, secrete key vitamins and protect their own GI tract from foreign microbes and structural degradation.
Through great strides in technology, especially through the development of omics methods, today's research can look beyond culture based techniques to understand the parts of the gut microbiome that previously cannot be reached. As the composition of the gut microbiome is tied to several health conditions such as Crohn's disease, cancer, asthma, diabetes, obesity, depression, and anxiety, it is crucial that research moving forwards continues to apply new techniques and methodologies to better navigate treatments and lifestyle preventions that should be implemented to better human health.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Gorbach SL. "Microbiology of the Gastrointestinal Tract." In: Baron S, editor. Medical Microbiology. 4th edition. Galveston (TX): University of Texas Medical Branch at Galveston; 1996. Chapter 95.
- ↑ 2.0 2.1 Sender R., Fuchs S., and Milo R. "Revised Estimates for the Number of Human and Bacteria Cells in the Body." PLOS Biology 14(8): e1002533. 2016
- ↑ Kho Zhi Y., Lal Sunil K. "The Human Gut Microbiome – A Potential Controller of Wellness and Disease." Frontiers in Microbiology, Vol.9. 2018
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 Thursby, E., and Juge, N. "Introduction to the human gut microbiota" Biochemical Journal, Vol.474(11),1823-1836. 2017
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 Jandhyala, S.M., Talukdar, R., Subramanyam, C., Vuyyuru, H., Sasikala, M., and Reddy, D.N. "Role of the normal gut microbiota" World Journal of Gastroenterology : WJG, Vol.21(29), 8787-8803. 2015
- ↑ Clark, H. "Culturing anaerobes." Nature Research. 2019
- ↑ Stone, L. "Faecal microbiota transplantation for Clostridioides difficile infection." Nature Research. 2019
- ↑ Brunello, L. "Gut microbiota transfer experiments in germ-free animals." Nature Research. 2019
- ↑ Tang, L. "Sequence-based identification of human-associated microbiota." Nature Research. 2019
- ↑ [https://www-sciencedirect-com.turing.library.northwestern.edu/science/article/pii/S088240101530231X Hugon, P., Lagier, J.C., Colson, P., Bittar, F., and Raoult,D. "Repertoire of human gut microbes." Microbial Pathogenesis, Vol 106, 103-112. 2017]
- ↑ 11.0 11.1 Nature. "Human microbiota affects response to cancer therapy." Nature Research. 2019
- ↑ 12.0 12.1 [https://www-ncbi-nlm-nih-gov.turing.library.northwestern.edu/pmc/articles/PMC4690201/ Zitvogel, H. et al. "Cancer and the gut microbiota: An unexpected link." Science Translational Medicine, Vol 7(271). 2015]
- ↑ 13.0 13.1 13.2 13.3 [https://doi-org.turing.library.northwestern.edu/10.1038/nature11550 Lozupone, C., Stombaugh, J., Gordon, J. et al. "Diversity, stability and resilience of the human gut microbiota." Nature, Vol 489, 220-230. 2012]
- ↑ 14.0 14.1 Rodriguez, J.M. et al. "The composition of the gut microbiota throughout life, with an emphasis on early life." Microbial Ecology in Health and Disease, Vol 26. 2015
- ↑ 15.0 15.1 McBurney, M.I. et al. "Establishing What Constitutes a Healthy Human Gut Microbiome: State of the Science, Regulatory Considerations, and Future Directions." The Journal of Nutrition, Vol 149(11), 1882–1895. 2019
- ↑ 16.0 16.1 Cully, M. "Antibiotics alter the gut microbiome and host health." Nature. 2019
- ↑ 17.0 17.1 17.2 Mahnic, A. et al. "Distinct Types of Gut Microbiota Dysbiosis in Hospitalized Gastroenterological Patients Are Disease Non-related and Characterized With the Predominance of Either Enterobacteriaceae or Enterococcus." Frontiers in Microbiology. Vol 11. 2020
- ↑ 18.0 18.1 18.2 18.3 Carding, S. et al. "Dysbiosis of the gut microbiota in disease." Microbial Ecology in Health and Disease. Vol 26. 2015
- ↑ Castaner, O. et al. "The Gut Microbiome Profile in Obesity: A Systematic Review." International Journal of Endocrinology. Vol 2018. 2018
- ↑ 20.0 20.1 Pierce, J. M., and Alvina, K. "The role of inflammation and the gut microbiome in depression and anxiety." Journal of Neuroscience Research. Vol 97(10), 1223-1241. 2019
- ↑ 21.0 21.1 21.2 Tap, J. et al. "Towards the human intestinal microbiota phylogenetic core." Environmental Microbiology. Vol 11(1), 2574-2584. 2009
- ↑ 22.0 22.1 Cheng, M. and Ning, K. "Stereotypes About Enterotype: the Old and New Ideas." Genomics, Proteomics & Bioinformatics. Vol 17(1), 4-12. 2019
- ↑ 23.0 23.1 23.2 23.3 Wexler, H. M. "Bacteroides: the Good, the Bad, and the Nitty-Gritty." Clinical Microbiology Reviews. Vol 20(4), 593-621. 2007
- ↑ Flint, H. J. and Duncan, S. H. "Bacteroides and Prevotella." Encyclopedia of Food Microbiology (Second Edition). Academic Press, Oxford. 2014
Authored for Earth 373 Microbial Ecology, taught by Magdalena Osburn, 2020, NU Earth Page.