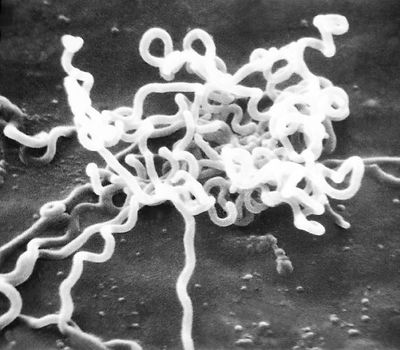
Treponema Pallidum

Etiology/Bacteriology
Taxonomy
Domain: Bacteria
Phylum: Spirochaetes
Order: Spirochaetales
Family: Spirochaetaceae
Genus: Treponema
Species: T. pallidum
Description
Treponema pallidum is a motile, spirochaete bacterium that has subspecies that can cause treponemal diseases such as syphilis, pinta, bejel, and yaws. syphilis is caused by the subspecies T. pallidum pallidum. Pinta is caused by T. pallidum carateum. Bejel is caused by T. pallidum endemicum. Finally, yaws is caused by T. pallidum pertenue. The four subspecies of T. pallidum are morphologically and serologically identical, but their course of action and transmission differs from one another. Even though T. pallidum can cause all four of these diseases, the most serious and concerning of these is syphilis. T. pallidum is a small bacterium that cannot be seen via Gram stain because it is too thin. However, it can be viewed by using dyes like Dieterle Stain [1]. It can also be detected by serology tests. syphilis is transmitted venereally while the other T. pallidum diseases are not. There were reported cases of syphilis-like symptoms dating back to the 14th and 15th centuries with a possible origin being Europe. The symptoms appear in 3 stages and include sores, rashes, latent periods, nervous system damage and eventually death[1].
History
There are reported cases of syphilis-like symptoms that date back to the 13th-14th century in Europe[2]. However, the first treponemal diseases are theorized to have originated in East Africa. The disease is said to have migrated from Africa into Asia, Europe, and North America possibly due to the slave trade[3]. Another theory is that the disease started in Europe and from there spread to Africa, Asia, and North America. It is said that a European explorer named Vasco da Gama carried the disease to Calcutta in 1498 and from there it spread to Africa and then Asia by 1520[4]. There is also a possibility that syphilis cases were reported as a mistake because before 1500 there was not a distinction between syphilis and leprosy[5]. However, it is important to remember that these are all just theories and there is no definitive answer for where or when syphilis emerged. It wasn't until 1905 that the bacterium that causes syphilis was discovered by German researches. From 1932 until 1972 the Tuskegee study was conducted in order to watch the progression of the disease. By 1943 Penicillin was widely used to combat this disease. However, during World War II there was a large outbreak of syphilis cases in the U.S. where over 500,000 cases were reported per year[6][7].
Pathogenesis
Transmission
Syphilis is transmitted venereally via direct contact with primary or secondary sores (chancres)[8]. This can include anal, vaginal, or, oral contact with an infected person. syphilis can also be transmitted congenitally from mother to child through the placenta during pregnancy. syphilis cannot be transferred by toilet seats, swimming pools, door knobs, eating utensils, sharing clothes, etc. because it is oxygen sensitive[9][10].
Colonization
Syphilis can only naturally grow in human hosts[7]. It can attach to a wide variety of cells such as epithelial, endothelial, and fibroblastlike cells. Syphilis enters the body through a breach in the skin or mucous membranes. It can move to the blood stream, spinal fluid, and to other internal organs very rapidly via its internal flagella. This diffusion can be seen in the secondary stage of infection when the body is covered in a rash as a result of infection with the disease[10]. T. pallidum attaches to cells by using adhesion molecules to "cap" the host cells.The extracellular matrix is involved in mediating the attachment of T. pallidum to the fibronectin-coated coverslips of the host cells[7].
Incubation and Infectious dose
As seen in guinea pigs, the infectious dose of Treponema pallidum is anywhere between 10 to 1,000,000 organisms. However the mean number seems to be about 100 organisms to cause infection[11]. The incubation period is unusually long taking about 30-33 hours for T. pallidum to double in vivo. In a culture it takes anywhere from 30-50 hours to double. Symptoms for the primary stage of this disease can occur between 10-90 days after contact with the bacteria[7][12]. The secondary symptoms occur 2 weeks to 12 weeks after contact, the latent period is about 1 year after infection. There are three types of tertiary stage symptoms that can occur with the first being cardiac occurring 10-30 years after infection. Neurosyphilis symptoms can be seen 2-20 years after infection and Gumma can be seen 1-46 years after infection (with the mode being 15 years). There are also two types of congenital syphilis symptoms; early (onset to two years), or late (persistence to greater than two years)[13].
Virulence Factors
Syphilis has a few very important virulence factors. One factor in particular it its corkscrew shape. It's shape gives it the ability to maneuver through gel-like material which is necessary when traveling through the genital and oral cavities. This allows syphilis to enter in areas many other disease causing bacteria could not[10]. Syphilis produces many lipoproteins which induces the expression of inflammatory mediators when recognized by TLR's. Treponema has three proteins with fibronectin adhesion molecules. The three molecules are named for where they were discovered in the genome sequence. Tp0155 binds to matrix fibronectin which suggests that it is functional in the blood stream. The next molecule, Tp0483, binds to both soluble and matrix fibronectin which suggests it is functional in tissues. Tp0751 is the last molecule and it binds specifically to laminin which means it can bind to laminin coated coverslips. The different protein molecules could suggest all the different types of tissues syphilis can invade and use to diffuse throughout the body. Syphilis also contains an endoflagellum located between the cytoplasmic membrane and the outer membrane. The fact that this flagella is internal makes it hard for the host immune system to completely attack the organism. The flagella is made up of several protein filaments and it is theorized that those proteins are what the immune system recognizes rather than an external flagella. Syphilis has methyl-accepting chemotaxis transmembrane proteins (MCPs) and cytoplasmic chemotaxis proteins (Che) which help it to perform chemotaxis. MCP's may have a high affinity to glucose and histidine whereas Che helps syphilis respond to nutrient gradients so it can move from tissues into the bloodstream. Syphilis has also been known to induce the production of matrix metalloproteinase-1 (MMP-1) which breaks down collagen in dermal cells. This could be how syphilis is able to penetrate tissues[7]. Syphilis also has a very slow generation time that could help keep the immune system from recognizing its presence. The slow generation time and the low infectious dose may keep the organism hidden (latent) until it is triggered to grow faster and cause symptoms[7]. The outer membrane proteins of T. pallidum are rare in nature and have been the target of many research studies because antibodies cannot easily bind to them. For this reason it is a very difficult and slow process for the antibodies to bind the bacteria. There is a surface protein on T. pallidum called TprK that is said to be able to down regulate old forms of the proteins and simultaneously up regulate new mutations of the protein. The purpose of this process is that the immune system does not recognize the new protein so a new infection can occur creating chronic infection of the disease.TprK is highly antigenic and able to mutate quickly to avoid being recognized by the host immune response to help it produce a chronic infection. Also the fact that when exposed to syphilis one is exposed to multiple different strains with different TprK proteins makes it difficult for the immune system to recognize each one and attack it accordingly.
Clinical features
Incidence and Mortality
According to the World Health Organization, it is estimated that there are 12 million new cases of syphilis introduced each year. In the United States syphilis is the third most common bacterial STD[14]. The CDC estimates that 55,400 new people are infected with syphilis each year. Of the 55,400 people, approximately 14,000 of those infections were received when the partner was in the primary or secondary stages of the disease. In 2010-2011 the total number of cases of syphilis infections increased by 0.4%. In 2011 in the United States the south accounted for 44.5% of all syphilis infections and the subset of the population with the highest number of people infected with syphilis was men ages 20-29, accounting for almost 50 people per 100,000[8]. Even though the rates increased slightly in 2011, the overall trend of cases is decreasing among all groups except for men who have sex with men(MSM). This profile of people now accounts for almost 75% of all primary and secondary cases of syphilis per year. African Americans also make up the largest race of people infected with this disease[8].
It is unknown how many people die from syphilis each year due to the variable nature of the disease and the many different complications that can arise from it. Some complications can include aneurisms, dementia, blindness, arthritis, damage to internal organs, paralysis, etc. If these complications are left untreated it is possible for them to become severe enough to cause death. The percentage of people that have complications are as follows: 16% Gumma syphilis, 10% Cardiovascular syphilis, and 6% Neurosyphilis. It is also said that from a study conducted 113 people died from STD's, 105 of them as a result from these late stage complications of syphilis[12].
Symptoms
The symptoms of syphilis occur in three stages after infection.
Primary Stage

The primary stage is categorized by a single to multiple localized sores/chancres on the genitals. The chancres appear to be firm, red, and painless making them sometimes difficult to notice. The chancre will appear at the site syphilis entered the body 10-90 days after exposure. It will remain for about three to six weeks before seeming to heal and disappear on its own even without treatment. At this point of the person has not been treated they will enter into the secondary stage of infection[13[8].
Secondary Stage

The secondary stage is characterized by a rash present on the body either on the palms of the hands or the bottom of the feet. The rash appears as redish brown or red, rough, spots and typically does not itch[8]. A rash can also appear on other parts of the body and could have a different appearance, or the rash may be so faint that it could go undetected. The secondary symptoms can start while a chancre is still present or it could appear weeks after the chancre has "healed"[15]. Other symptoms of the secondary stage include fever, headache, patchy hair loss, sore throat, muscle fatigue, and weight loss. All of these symptoms will subside on their own whether they are treated or not. If the symptoms are not treated the person will further progress into the latent and late stages of syphilis.
Latent Stage
The latent stage is a hidden stage. It is a period where no symptoms of the disease are present. This stage can last for years before returning and progressing into the tertiary stage or the disease may never return[15]. There are 2 stages to latent syphilis. The early latent period is less than one year since infection occurred and is able to be transmitted to new hosts. The late latent period is at least one year after being infected and is no longer infectious. Because there are no symptoms during the latent stage the only way to test for syphilis is through serology tests[13].
Tertiary Stage

Of all the people that become infected with syphilis, 15-30% of them will have complications and enter into the tertiary stage. There are three subcategories of complications that can arise from tertiary syphilis; Gummatous syphilis, Cardiovascular syphilis, and Neurosyphilis. Gummatous syphilis is characterized by lesions that are in the skeletal system, skin, mucous membranes, other organs. Although these lesions do not typically result in death, if they occur on the brain, heart, etc. they can cause very serious complications. Cardiovascular syphilis destroys the elastic tissue in the aorta. This can result in aneurysms or valve insufficiency. Neurosyphilis is a central nervous system disease that can cause motor and sensory inhibitions, signs and symptoms of meningitis, dementia, paralysis, blindness, numbness, etc. It is possible for people to have neurosyphilis and be asymptomatic [16].
Diagnosis
Syphilis tests detect the antibodies that ones body will produce in response to infection with the disease. These tests are used to first screen for the disease and later confirm it[17]. Venereal disease research laboratory test (VDLR) is a test that detects for antibodies, such as IgG, in the blood or spinal fluid[18]. Because this antibody can be produced for other diseases besides just syphilis it may not be completely accurate. This test is also not accurate in the very early or advanced stages of the disease. Rapid plasma reagin test (RPR) also detects the presence of antibodies. Enzyme immunoassay test (EIA)is a new blood test that tests for antibodies. Fluorescent treponemal antibody absorption test (FTA-ABS) can test for the presence of antibodies and the bacteria itself if used 3-4 weeks after infection. The test can be run on blood or spinal fluid. Treponema pallidum particle agglutination assay (TPPA)is used in addition to other tests in order to confirm the presence of antibodies and the bacteria in the blood. Dark field microscopy can be used to take a bacterial sample from an open wound or chancre and used to examine under a microscope to detect syphilis at an early stage. Microhemagglutination assay (MHA-TP) is used to confirm positive results from other tests[17].
Treatment
The current treatment for syphilis is Penicillin or alternative drugs if you are allergic. If treatment starts in an early stage of detection, one dose of Penicillin is normally enough to control and kill the bacteria. Side effects of receiving a Penicillin shot are fever, chills, nausea, headache, and body aches. These symptoms should only last for one day[15]. Women should always be tested for syphilis when they become pregnant to keep the baby from becoming infected with the disease[19]. Penicillin began to be widely administered in 1947 for the treatment of syphilis. Long before the days of Penicillin from the 1400's to the 1600's Mercury was used in an ointment form and rubbed into the skin chancres. The next chemical used specifically for syphilis was Potassium Iodide in the 1840's. This chemical was highly effective in treating the later stages of syphilis infections whereas Mercury was only moderately effective on late stages. Potassium Iodide helped pave the way for Salvarson. Salvarson, also known as the Magic Bullet, was compound number 606 that Paul Ehrlich created to cure syphilis. It was an arsenic mixture that was aimed at killing the bacteria and not the host. This idea of creating a "Magic Bullet" is still with researchers today when experimenting with new drugs[20].
Prevention
There is no vaccine available for syphilis because it is a bacterial infection. In order to prevent yourself and others from becoming infected with the disease there are simple steps you can take. Remain abstinent because without sexual contact the disease cannot spread. If you are having sex with someone who is infected with the disease, or even just as a precaution, use a condom. The condom is only helpful in preventing the spread of the disease if it fully covers the sores. Also, have a monogamous relationship to prevent the disease from spreading to more people[15].
Host Immune Response
The host immune system has difficulty responding to treponemal bacteria unless they are not in one piece. In other words, as long as the treponema are whole they are nonantigenic. The outer membrane proteins of T. pallidum are rare in nature so antibodies cannot easily bind to them. For this reason it is a very difficult and slow process for the antibodies to opsinize the bacteria. Because T. pallidum does not have cytotoxins, LPS, or other common virulence factors it is very likely that the physical characteristics seen with a syphilis infection are due to the immune system's inflammatory response. At the time of bacterial invasion phagocytic cells swarm to the area of infection to control it and try to kill it. In the lesions many CD4 and CD8 co-receptors are found. The co-receptors signal for T cells to move to the area of infection. T cells have the ability to secrete granzyme B and perforin which are lytic mediators. These lytic mediators are one way in which tissue is degraded to continue to form lesions in the skin. It is possible that because syphilis will continue to infect a person without proper treatment it means that the phagocytic cells cannot adequately control the infection. Dendritic cells are specific phagocytic cells that engulf pathogens at the site of infection. T. pallidum becomes engulfed by these cells and is then taken to the lymph nodes where they activate T cells. This could be how syphilis is able to quickly spread throughout the entire body[7].
References
(1)http://www.princeton.edu/~achaney/tmve/wiki100k/docs/Treponema_pallidum.html
(2)http://www.news-medical.net/health/Syphilis-History.aspx
(3)http://cid.oxfordjournals.org/content/40/10/1454.full
(4)http://www.infoplease.com/cig/dangerous-diseases-epidemics/syphilis-sexual-scourge-long-history.html
(5)http://archive.archaeology.org/9701/newsbriefs/syphilis.html
(6)http://www.intheknowzone.com/sexual-health-topics/syphilis/history-of-syphilis.html
(7)http://cmr.asm.org/content/19/1/29.full
(8)http://www.cdc.gov/std/syphilis/stdfact-syphilis.htm
(9)http://www.webmd.com/sexual-conditions/guide/syphilis
(10)http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1360276/
(11)http://www.ncbi.nlm.nih.gov/pmc/articles/PMC257764/
(12)http://emedicine.medscape.com/article/229461-overview#a0104
(13)http://www.gov.mb.ca/health/publichealth/cdc/protocol/syphilis.pdf
(14)http://www.virtualmedicalcentre.com/diseases/syphilis/119#Statistics
(15)http://www.mayoclinic.com/health/syphilis/DS00374/DSECTION=symptoms
(16)http://health.nytimes.com/health/guides/disease/neurosyphilis/
(17)http://www.webmd.com/sexual-conditions/syphilis-tests
(18)http://onlinelibrary.wiley.com/doi/10.1002/ana.410110107/abstract
(19)http://www.cdc.gov/std/pregnancy/stdfact-pregnancy.htm
(20)http://www.allsands.com/health/advice/syphilishisto_zkq_gn.htm
Created by Rachael Acosta, student of Tyrrell Conway at the University of Oklahoma.
