Tuberculosis in Children in Developing Countries: Difference between revisions
No edit summary |
|||
| Line 1: | Line 1: | ||
{{Curated}} | |||
Edited by Stephanie White | Edited by Stephanie White | ||
==Introduction== | ==Introduction== | ||
Latest revision as of 19:55, 11 August 2010
Edited by Stephanie White
Introduction
Today, tuberculosis is responsible for the death of more young people than any other communicable disease [7]. It is estimated that two children die of a tuberculosis infection every minute [7]. Most Tuberculosis cases are found in low-income regions like Southeast Asia and Africa. Southeast Asia has one of the highest incidence rates of Tuberculosis and contains nearly 34% of all cases worldwide [5]. It is also estimated that in every 100,00 people living in Sub-Saharan Africa 350 are living with Tuberculosis [5]. One factor that contributes to a higher incidence of Tuberculosis cases in low-income countries is HIV and AIDS. Tuberculosis is one of the most deadly opportunistic infections that a person with HIV or AIDS can acquire [5]. Since the immune system of these individuals is compromised, tuberculosis is a common and deadly condition [5]. In most cases, Tuberculosis in children can be traced back to an adult host [3]. The presence of Tuberculosis in children is an important indicator of the overall status of health in a particular country. In many developed nations, Tuberculosis can be treated fairly easily with antibiotics. However, emerging strains of multi-drug resistant stands of Tuberculosis pose a major treat to the health of all populations, especially children. Public health strategies are crucial to controlling Tuberculosis because access in developing countries to effective antibiotics is limited. Children react different to Tuberculosis because their immune systems are still in a developmental state [6]. It is crucial that Tuberculosis in children is carefully controlled in developing countries so that a drug resistant strain does not cause another major worldwide epidemic.
Tuberculosis Infection and Transmission
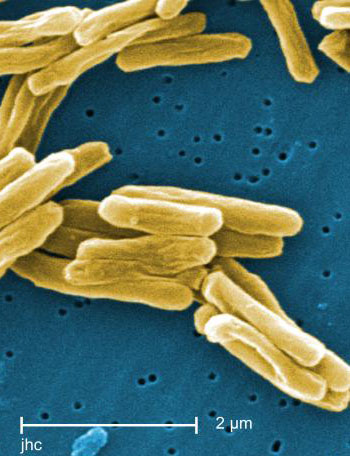
Tuberculosis is caused by the bacteria Mycobacterium tuberculosis and is a highly contagious disease. Individuals contract the infection by inhaling tuberculosis bacilli in the air [5]. This bacterium is released through coughing, sneezing, breathing, and talking [5]. Tuberculosis bacteria can remain dormant in the lungs for an extended period of time but never develop into the disease. It is estimated that only 5 to 10% of cases will progress to be infectious or to Tuberculosis disease [5]. Tuberculosis affects children much differently than adults. When a child is infected, they have fewer bacteria in their lungs than an adult with the disease [8]. As a result, it is uncommon for children to infect other individuals with tuberculosis. The microbiology of myocardium tuberculosis makes it very difficult to treat. Since tuberculosis is a gram-positive bacterium, it has a very thick cell wall [8]. Antibiotics must be used for several months in order to break through the thick cell walls and kill the bacteria [8]. When an individual contracts tuberculosis, the body has natural defense mechanisms to combat the infections. Chemicals known as cytokines are released to activate macrophages to kill the tuberculosis bacteria [8]. CD4 cells are also very important for the body to fight this type of infection. HIV destroys CD4 cells, which makes it very easy for and HIV positive individual to contract tuberculosis [8].
There are four main stages in a tuberculosis infection in a child. First, in the primary infection phase, the bacterium invades the cells of the lungs and either spreads or remains latent in the lungs [8]. If the body is able to initiate an immune response, t cells will fight the bacteria in the asymptomatic healing phase. However, in most cases the immune response is not strong enough and the infection moves to the hilar lymph nodes creating symptomatic primary tuberculosis [8]. The next phase of a tuberculosis infection occurs 4 to 5 weeks after the primary infection and is known as symptomatic primary tuberculosis [8]. In this stage, the tuberculosis bacterium causes pleural effusions, pneumonia, and lobar collapse [8]. Depending on the state of the immune system in a child, the tuberculosis can also cause military tuberculosis or tuberculous meningitis [8]. The final stage of the disease is tuberculosis after primary infection [8]. During this period, children are usually free of symptoms but it is still possible for bacteria to be present in the body and cause another tuberculosis infection [8].
Diagnosis
Diagnosing children for tuberculosis is very difficult because the test for tuberculosis can yield false results. When a child is first suspected of having tuberculosis he or she is given a chest radiograph [8]. However, this procedure is not completely effective in diagnosing tuberculosis because it is difficult to distinguish between other respiratory infections such as pneumonia [8]. A child can then give a sputum sample to be analyzed for the presence of tuberculosis but due to the low bacterial load, this test often fails in children. On average, tuberculosis bacteria in a child’s sputum can only be detected in 10 to 15% of cases while the bacteria can be confirmed in 60% of adult cases [8]. As a result, more advanced diagnostic tests must be given to correctly identify a tuberculosis infection. It is common for physicians in low-income countries to rely on symptoms for their tuberculosis diagnosis because more advanced test are too expensive [1]. Since the diagnosis of tuberculosis in children is inaccurate, many treatment centers will not accept their cases. When children do not receive a specific treatment plan (DOTS), they rely on any tuberculosis drugs that their families can acquire and afford [1]. This situation is very dangerous for the child and the health of a community because when a child does not receive proper treatment for a tuberculosis infection, it is more likely that a multidrug-resistant strain will emerge [1]. It is crucial that public health institutions implement a strategy for the diagnosis and treatment of tuberculosis in children so that drug resistant cases do not develop and put the entire community at risk.
Treatment
Treatment for tuberculosis infections is very important due to the lengthy time required to fully kill the bacteria. The drug combinations used to treat tuberculosis in adults are also used in children in smaller doses [8]. Most antibiotic combinations are able to destroy 90% of the bacteria within the first two weeks of treatment [8]. However, the drugs must be taken for a full 6 months in order to ensure that the remaining 10% of tuberculosis bacteria is killed [8]. Due to the extensive treatment period, it is common for patients to abandon their treatment plans. This is extremely dangerous because the bacteria can become resistant to antibiotics and require more extensive and experimental treatment. Directly observed therapy (DOTS) is used to treat patients with multidrug-resistant tuberculosis. DOTS is effective because a health professional observes a patient taking their antibiotic everyday to ensure adherence to the treatment regimen [8]. However, DOTS treatment plans can be very expensive so they are not realistic for a number of developing countries. Today, there are also vaccines that are available for children to prevent tuberculosis. The BCG vaccine contains a live stain of tuberculosis and is the most commonly used vaccine in children [8]. However, the vaccine has varied levels of protection and is not effective in specific geographic regions including India [8]. Vitamin D has also shown to be an important factor in the prevention and treatment of tuberculosis in children. Increasing vitamin D intake can naturally increase a child’s defense against mycobacteria [8].
Public Health Strategies and Case Studies
Include some current research in each section.
Recent research in Africa has confirmed the likelihood that a child will contract pulmonary Tuberculosis if an adult in the household carries the disease. The children were studied in South Africa where there is a low average economic income and high prevalence of Tuberculosis [2]. Initially, 53% of the 125 children were infected with the bacteria but only 11% had developed Tuberculosis disease. [2]. After the 30 month period the number infected with Tuberculosis stayed fairly constant at 54% while the number with the disease rose to 24% [2]. The results proved that children have a 76% chance of being infected with Tuberculosis if they live with an adult with a smear positive Tuberculosis case [2]. During this particular study, treatments for Tuberculosis infection were also studied. The children who had never been treated for a Tuberculosis infection were given a chemoprophylaxis, which is a preventative treatment for Tuberculosis [2]. If a child had received previous chemoprophylaxis treatments, he or she was given a different 4 to 5 drug combination to treat the tuberculosis. The chemoprophylaxis treatment required the child’s parents or caregivers to take them to the clinic 5 days per week for treatment and observed therapy [2]. This kind of treatment proved to be successful because of the 41 children that received chemoprophylaxis treatment, 29 children tested negative for tuberculosis [2]. Public health organizations and workers should promote funding for preventative medications for children because they were effective in protecting children who were continually exposed to tuberculosis. However there are a number of limitations for developing countries in preventing tuberculosis infections. In order for treatment to be effective, parents or caregivers must bring their children to a clinic very frequently which is often difficult due limitations such as type of employment and transportation availability. In addition, many of the drugs required for preventative chemoprophylaxis are quite expensive and their use in developing nations would require funding from a higher income country or non-governmental organization.
Multidrug-resistant tuberculosis in India is becoming a major global health issue because nearly 2 million new cases are detected each year [1]. Many adults have been carefully observed and given short course treatments known as DOTS (directly observed treatment)[1]. However, there has been little done in India to prevent and treat tuberculosis infection in children. It is likely that children in larger cities in India, such as Mumbai, live in overcrowded conditions and are frequently subjected to tuberculosis and multidrug -resistant strains of tuberculosis [1]. Since children often test negative for acid-fast bacilli, it is difficult for public health workers to determine how many are living with tuberculosis [1]. Economic limitations prevent children from receiving more diagnostic tests to determine if they have tuberculosis. Another factor that is affecting the development of multidrug-resistant tuberculosis in children is AIDS. HIV and AIDS make any individual more likely to acquire a tuberculosis infection [1]. Researchers have found that most individuals are not able to purchase antiretroviral therapy for their children but may be able to afford a combination of drugs that help fight tuberculosis [1]. The most common drug mixture includes isoniazid, rifampicin, pyrazinamide, and ethambutol [1]. This treatment option will help prevent tuberculosis from developing in children with HIV or AIDS, but will not protect them from multidrug-resistant tuberculosis [1]. Other public health strategies for the prevention of tuberculosis in children involve steps to reduce the maternal transmission of HIV [ 1]. If the number of pediatric cases of HIV could be reduced, a child’s likelihood of developing tuberculosis would be greatly reduced.
Conclusion
The prevention and treatment of tuberculosis in children is an important global health issue in all countries, especially low-income countries. Tuberculosis infections in children are much more difficult to diagnose but they are much less contagious due to the low bacterial load present in the lungs. In almost all cases, children contract a tuberculosis infection from an adult in their community. There are several factors that could help reduce the global incidence of tuberculosis in children. First, new researchers could work to develop new forms of testing to correctly identify the presence of mycobacterium tuberculosis in children. This would make it possible for children to receive appropriate treatment for their illness and prevent the emergence of a multidrug-resistant strain. In addition, public health initiatives that aim to reduce the prevalence of HIV and AIDS will affect tuberculosis cases. Since tuberculosis is an opportunistic infection, reducing the incidence of HIV will directly reduce the incidence of tuberculosis. Global eradication of tuberculosis in children is possible but it will require the commitment of governments, communities, patients and public health officials.
References
[1] "Children and Multi-drug Resistant Tuberculosis in Mumbai (Bombay), India" Centers for Disease Control and Prevention
[2] Schaaf, Simon H., Robert P. Gie, Magdalene Kennedy, Nulda Beyers, Peter B. Hesseling and Peter R. Donald. " Evaluation of Young Children with Adult Multidrug Resistant Tuberculosis: A 30 Month Followup" 2002;109;765-771Pediatrics.
[3] Shingadia D, Novelli V. "Diagnosis and treatment of tuberculosis in children" Department of Academic Child Health, St Barthlomews and The London Medical and Dental School, Queen Mary, University of London, UK
[4] "Tuberculosis" Baylor School of Medicine.
[5] "Tuberculosis" World Health Organization
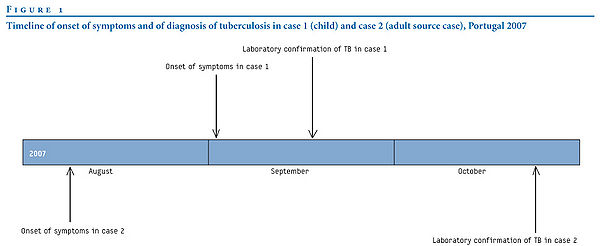
[6] "TUBERCULOSIS IN A CHILD – SEARCH FOR THE INFECTED ADULT NEARBY" Eurosurveillance
[7] "TB in Children" TB Alert
[8] "Tuberculosis in Children" Student BMJ Archive
[9] "Tuberculosis" Foundation for Innovative New Diagnostics
Edited by student of Joan Slonczewski for BIOL 191 Microbiology, 2009, Kenyon College.