Variant Surface Glycoproteins (VSGs) of Trypanosomes
Trypanosomes
By Kelly Wahl
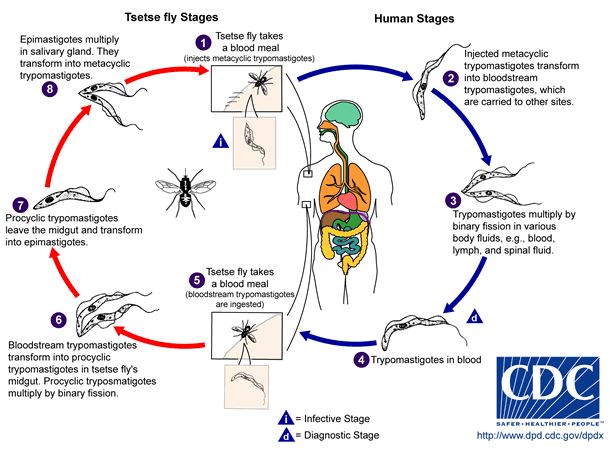
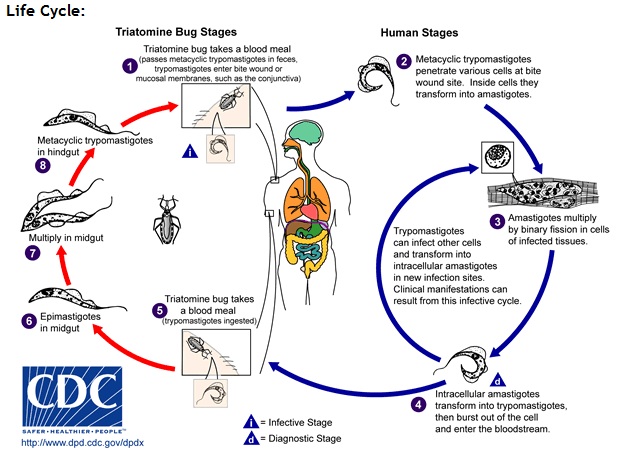
Trypanosomes are single-celled flagellated eukaryotic parasites causing trypanosomiasis in humans and livestock or as it is more commonly known as, sleeping sickness in Africa, and Chagas disease in the Americas. These parasites are usually introduced into the body via an arthropod vector. The tsetse fly (subgenus Glossina morsitans), transmits the strains Trypanosoma brucei gambiense (95% of reported cases and found exclusively in West Africa) and Trypanosoma brucei rhodesiense (5% of reported cases, only seen in East Africa) responsible for sleeping sickness through its bite(figure 2). Oddly the geographic range of these two strains does not overlap [3]. In central and South America the kissing bug (subfamily Triatominae) spreads Trypanosoma cruzi when its feces enter the body through the mucosal membranes, or broken skin (bite marks or scratches)(figure 3). Besides T. brucei, and T. cruzi, there are many other strains of trypanosomes that affect mainly domesticated animals like; cows, camels, horses, donkey but can also cause disease in deer, and antelope.
These parasites fall under the order Kinetoplastidia and are related to another important parasite, Leishmania. Kinetoplasts are called such because of the kinetoplast at the base of their flagellum. A kinetoplast is a mitochondrion with coiled mitochondrial and genomic DNA. The kinetoplast changes size and shape throughout the parasites life cycle and is the target site of some anti-parasitic drugs such as ethidium. Kinetoplasts broke off from the common eukaryotic ancestor fairly early on and consequently transcription of their genome is unique and the target of potential drugs [2, 11].
Trypanosome Infection; Sleeping Sickness, and Chagas Disease
Sleeping Sickness
Stage one of T. brucei infection is the haemolymphatic stage. Where parasites circulate and multiply by binary fission in the blood and lymph systems. Clinical infection with T. b. rhodesiense often begins as a sore called a chancre and is followed a week or two of headaches, fevers, muscle pain, joint pain and possibly a rash. Patients may also show Winterbottom’s sign; enlarged, tender lymph nodes in the neck. T. b. gambiense infection shows the same symptoms but they are not as severe and last for a longer period of time [3, 4].
The second stage of infection is neurological. The parasites have crossed the blood-brain barrier and are now multiplying in the central nervous system. classic symptoms include rapid weight loss, impaired motor skills, seizures, confusion, and changes in personality. A disrupted circadian rhythm is the source of this disease’s name. Patients lie awake at night but sleeps during the day. Without treatment T. b. rhodesiense infection progress to coma and death within a few months. Often times T. b. rhodesiense infection moves so quickly that malnutrition, heart failure, and pneumonia cause death before the neurological problems ever manifest themselves. The progression of T. b. gambiense infection takes much longer and a person can take years to show neurological symptoms. The different clinical manifestations of the two strains stems from differences in the two strains stimulation of the immune system [3].
Chagas Disease
Chagas disease is similar to sleeping sickness in many ways. There is an acute stage when the parasite is circulating in the bloodstream and the initial site of infection swells and a patient may or may not present with signs of infection such as a fever. One of the classic signs of acute Chagas infection is Romana’s sign, the swelling of the area around the eye where the conjunctiva (mucosal tissue around the eye) or a site near the eye was the point of infection. Serious symptoms are rare in this stage of infection but possible. They include heart failure, chest pain, seizures, or paralysis.
Unlike sleeping sickness, Chagas disease only progresses to the chronic form of the disease in 20 to 30% or people infected. The remaining 70 to 80% of people infected remain asymptomatic for life and may or may never know they are infected. As the parasite replicates in the target tissues; cardiac muscle and digestive smooth muscle those infected show a variety of cardiac problems such as irregular heartbeat, blood flow disorders, issues with heart muscle function, and blood clots. As well as problems with the digestive tract such as ulcers [4].
Treatment
Symptomatic trypanosome infection is usually fatal if left untreated. While there is no vaccine or prophylactic drugs to prevent T. brucei infection there are drugs available for treatment of asymptomatic, acute, and chronic infections. The earlier the diagnosis is made the easier it is to manage symptoms with less toxic drugs that target the parasite outside of the central nervous system. once the infection has become symptomatic, stronger drugs with much higher toxicity must be used to cross the blood-brain barrier and attack the parasite in the CNS. If the infection has progressed to this point it is likely that a lengthy hospital stay is required to clear up infection. There is a need for new drugs to combat this disease because the toxicity associated with some of the drugs currently used to treat the infection are almost as bad as the infection itself.
Why Are Trypanosomes of Public health and Economic Interest?
African trypanosomiasis is of public health and economic importance for a number of reasons. Besides affecting humans other strains of trypanosomes also infect domesticated cattle making cattle sick with disease called Nagana. The inability to raise cattle because of trypanosome infection in sub-Saharan African further contributes to malnutrition in the area. Animals also serve as reservoirs to the T. b. rhodesiense strain making it difficult to eradicate the parasite in an area with infected cattle.
These parasites are only found within the tsetse flies’ geographic range, sub-Saharan Africa and have devastating economic effects on the people in that area because of the length and nature of trypanosomiasis. Those who rely on farming, fishing, and hunting are most at risk to be bitten by an infected tsetse fly and are also commonly the breadwinners in poor, rural populations [4]. While the WHO only reports about 10,000 new cases a year this number is most likely a gross underestimate of the true number of cases and other estimates put the number around 100,000 although others still caution that these numbers are underestimated when close to 50,000,000 are at risk [2,3,4].
Both African trypanosomiasis and Chagas disease are considered neglected tropical diseases under which a projected 534,000 deaths a year and account for millions of year of functional life lost due to disability or years of life lost due to ill health. Those affected are primarily low and middle income countries in areas where the disease is most prevalent. Under international public health, trypanosomiasis is important because of the number of lives lost and emerging rural economies stunted by this disease [13]. Domestically, Chagas presents a threat to blood and organ transplant recipients. It is estimated that there are more than 300,000 people living with T. cruzi infections in the U.S. Although natural transmission through triatomines found in North America is possible it is very rare and iatrogenic (through blood or organ transplants) exposure represents the greatest risk of route of domestic exposure [12].
In this increasingly globalized world diseases that once hid in the jungles of South America and the plains of sub-Saharan Africa have ended up on the doorstep of industrialized nations. Although trypanosomiasis is still considered a third-world disease infections are continually diagnosed in the first world and represent a real risk to anyone that can get on a plane and travel to an affected area.
Transmission and Life Cycle
Transmission
Although the most common route of infection is for T. brucei, and T. cruzi are run-ins with the arthropods Glossina morsitans and Triatominae . These parasites can be passed from mother to child during pregnancy. Blood transfusion and sex can also spread these parasites but this is very rare [3, 4].
Life cycle
Over the course of its lifetime a trypanosome cycles through five different morphological stages between arthropod vector and mammalian host. These different forms allow these parasites to live in very different host environments; from the gut of an insect to the central nervous system of a human [1].
The morphology of trypomastigotes within the mammalian body is distinctly different from the trypomastigotes found in insects because of differences in metabolic needs and the presence of variant surface glycoproteins (VSGs). These sugar-proteins are the secret weapon of trypanosomes that allow them to remain undetected by the immune system almost indefinitely. Ten million VSGs form homodimers with each other and stick out of the cell membrane like trees in a dense forest. Although VSGs amino acid sequences and attached sugars vary wildly from variant to variant their secondary and tertiary structures are highly conserved. In a way, VSGs are similar to the T cell receptors found on the surface of T cells in the immune system. Allelic exclusion ensures that only one VSG is expressed at a time. This monotypic surface coat is recognizable to B cells independent of signals B cells to differentiate. Even though the B cells are able to attack a particular VSG variant of the circulating trypomastigotes population there are always members of the population that have already silenced expression of that particular VSG and begun expressing a new VSG that has yet to be seen by the immune system [9].
In the midgut of the tsetse fly procyclic trypomastigotes proliferate and move to the salivary gland where they become morphologically distinct epimastigotes. After three weeks from the initial introduction of the trypanosomes into the midgut of the tsetse fly there are mature non-dividing metacyclic epimastigotes with VSGs ready for another round of mammalian infection. When the metacyclic epimastigotes enter the mammalian body through the bite of the fly they differentiate into “slender” form and travel in the lymph and blood systems reproducing by binary fission in almost all organs of the body. Some of these dividing slender forms become “stumpy” and stop dividing. Although the stumpy form is no longer dividing within the host this form can survive in the fly midgut where it differentiates into the procyclic form and complete the cycle of infection [1, 2].
While T. brucei multiplies in the extracellular space between cells, T. cruzi actually hides intracellularly and does not undergo the same antigenetic switching of VSGs. Instead it induces host cells to phagocytose it and escapes from the lysozyme into the cytoplasm before it is digested. A special protein is secreted that is only activated at low pH helps the parasite escape [2].
Variant Surface Glycoproteins (VSGs)
VSGs
Variant surface glycoproteins (VSGs) are sugar-proteins that coat the surface of trypomastigotes. There are at least 200 active VSG alleles and more than 1000 silent alleles and psuedogenes. Active genes can recombine with silent genes to form new unique active genes. This process is called antigenetic switching and allows the blood-stream, slender form of the parasite to continually change its “appearance” to the immune system and remain undetected through the course of infection. While the immune system eventually detects and makes antibodies to a particular VSG it cannot make antibodies to every type of VSG present on the surface of all the different circulating trypomastigotes. The immune response continually selects for the expression of new VSG variants. It is a case of the Red Queen’s race only the parasite eventually wins because it has more possible VSG variants than the immune system could ever catch before parasite proliferation in vital organs causes death. VSGs can also actively modulate various components of the immune system to further multiply throughout the body undetected. The mechanism that regulates this entire process is fairly unique but has been studied in yeast [1, 8, 9].
VSG expression
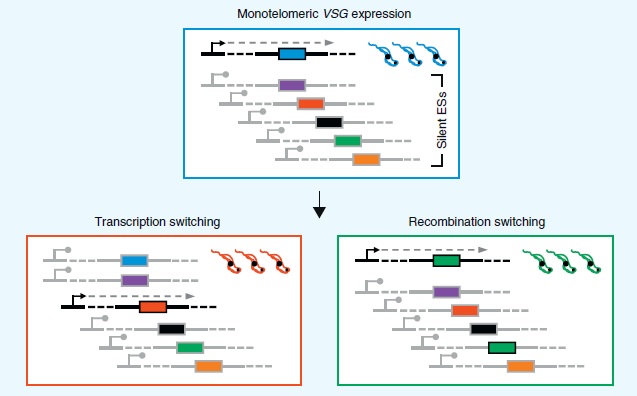
Only one of 10-20 VSG telomeric sites expression sites is available for transcription at a time while the rest are silenced. This strategy allows only one VSG coat with a given set of epitopes to be expressed at a time. The adaptive immune system eventually forms antibodies that bind to these epitopes and elicit an immune response but by the time this happens the parasite has silenced that expression site and begins expressing antigenetically different VSGs from another telomeric site. Oddly enough these expression sites are transcribed by RNA polymerase I. In eukaryotes RNA pol I is responsible only for the transcription of ribosomal RNA while RNA pol II is normally used for the transcription of other types of RNA [8].
There are two ways that VSGs are mono-telomerically expressed (only one site/one VSG is transcribed). Transcription switching is where an active telomeric site that was being actively transcribed is repressed and another active telomeric site that was silenced begins active transcription (figure 6). Recombination switching is the other way switch VSG expression. One of the thousand or so pseudogenes that cannot be transcribed on its own recombines with an active telomeric site so it can be expressed (figure 6). Active expression sites are flexible in their recombination. Psuedogenes are found in silent expression sites, the telomeres of chromosomes, and in subtelomeric VSG arrays. When recombining with active expression sites, either whole genes or segments of genes can be moved increasing the possible number of VSGs that can be expressed. The exact proteins involved and the mechanism by which they are able to recombine is still under study [8].
The mechanism that allows one telomeric expression site to be actively transcribed while the rest are silenced is generally known some of the details need to be worked out. It seems to involve the coiling and uncoiling of DNA from nucleosomes and other chromatin proteins. Nucleosomes are the spooling proteins that help structurally organize DNA and play a role in gene expression. Expression of certain genes is repressed when these proteins twist DNA up in such a way that RNA polymerase cannot physically bind the promoter region of the gene and begin transcription [8].
Expression site silencing requires at least six protein factors and operates by two different mechanism; short-range and long-range telomeric silencing. In short-range silencing, the modifications by the histone deacetylase SIR2rp1 is within 5 kbp of the expression site silence expression. HAT1 is the histone acetylase that reverses silencing and allows the histones to relax enough so active transcription can take place. Long-range silencing is controlled farther away from the expression site (about 50 kbp upstream) most likely through chromatin remodeling with a variety of histone deacetylases, acetylases, methylases, chromatin remodelers (assemblers and disassemblers of histones). The default for both of these mechanisms is silencing and almost all are required for growth. One of the factors being considered as a drug target is the deacetylase DAC3 [8].
While the mechanism of silencing expression itself is well understood the factors that control which genes are silenced or activated remains to be studied. Indeed it is amazing that with all of the potential VSG alleles available for transcription only one allele is transcribed at a time (monoallelic expression) [8].
Current Research
Expression of a Mosaic VSG Coat to Escape Early Detection by B-cells
Although only one VSG gene is expressed at a time the surface coat isn’t always made up of one VSG. Even though a new gene is being expressed the existing VSG coat doesn’t just disappear overnight. It takes about 48 hours for the VSG coat to completely switch from one variant to another. This lag period is due to the time is takes to transcribe, translate, and transport the new VSGs to the surface and get rid of residual mRNA and protein from the previous coat [9].
Recently Dubois et al. (2005) found that this 48 period of a mosaic VSG coat during antigenetic variation actually helps prevent B cells independent T cells from recognizing trypanosomes as new VSGs that are appearing on the surface of the cell amongst VSGs that have already been recognized by B cells. It is not until the surface coat again becomes monotypic with a single VSG present are B cells once again able to recognize the parasite and amount an immune response [9].
Athymic mice (lacking T-cells) were infected with a strain of T. b. rhodesiense that had been transformed to express two VSGs at the same time. Figure X shows dual VSG expression of transformed trypanosomes. Panel A of figure 7 shoes fluorescence labeled LouTat1 VSG while panel B shows labeled 117 VSG. Panel C shoes the overlay of both panels A and B, and panel D shows the same parasite under differential, interference, contrast microscopy independent of VSG labeling.
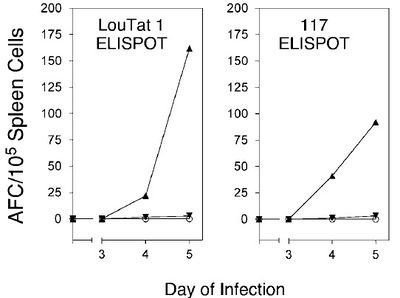
Wild-type trypanosomes could not be used because very few parasites in a given population are switching coats at any one time and dual expression of VSGs on the surface of cells is brief. An ELISPOT assay was done on B-cells from the spleen. They found that fewer B-cells were active and producing antibodies to either expressed VSG for the five says of infection. Figure 8 shows that the number of B-cells activated by VSG-co-expressing trypanosomes was near the level of B-cells activated in uninfected mice. It seems that B-cells are fooled by the insertion of variant VSGs in a monotypic coat during switching because the new VSGs breakup the pattern of identical epitopes that are required for B-cell activation independent of T cells [9].
Trypanosomes Effects on Immune Function
Besides hiding from the immune system with an ever-changing VSG surface coat trypanosomes also manage to down-regulate the function of various components of the immune system. one example of down-regulated function is the decreased ability of white blood cells to process and present newly encountered antigens after trypanosome infection [10].
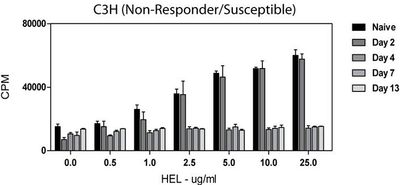
In 2009, Dagenais et al. showed that white blood cells taken from infected mice displayed a decreased ability to respond to newly encountered hen egg lysozyme (HEL) antigen ex vivo. This assay had to be done ex vivo in order to measure this type of activity in a controlled way. Extracted T-cells were irradiated and hybridized with hybridomas so cells could be grown in cell culture. The ability to process and present antigen was measured by the amount of interlukin-2 (IL-2) that was produced. After two days of infection radiolabeled thymidine was added to the hybridoma medium and the amount of IL-2 produced with incorporated radiolabeled thymidine was measure with a scintillation counter. A scintillation counter measures the amount of radiation in a sample as counts (or decays) per minute (CPM). IL-2 is an important cytokine that helps stimulate cytoxic T-cells and affects the process of T-cell immunologic memory, among other functions. Compared to naïve (uninfected) cells which displayed a dose-dependent response to the introduction of HEL. The relative amount of IL-2 produced by cells from infected animals did not change with concentration of HEL or day post infection (Figure 9)[10].
References
[1] Foster, W. F., and Slonczewski, J. L. (2010). Microbiology; An Evolving Science. New York: W.W. Norton & Company, Inc.
[2] Hunt, R. C. (2010, February 15). Parasitology-Chapter Three; Molecular Parasitology: Trypanosomes Eukaryotic cells with a different way of doing things. Retrieved April 16, 2011, from Microbiology and Immunity On-line: http://pathmicro.med.sc.edu/lecture/trypanosomiasis.htm
[3] Centers for Disease Control and Prevention (2010, November 2). Parasites - African Trypanosomiasis (also known as Sleeping Sickness) . Retrieved April 1, 2011, from the CDC: http://www.cdc.gov/parasites/sleepingsickness/
[4] World Health Organization (2011). Trypanosomiasis, African. Retrieved April 1, 2011, from the WHO: http://www.who.int/topics/trypanosomiasis_african/en/
[5] Pottinger, P. (2010, July 27). History of Chagas Disease. Retrieved April 20, 2011, from History of Infectious Diseases: http://idhistory.tumblr.com/
[6] Parasite Museum (2009, June 4). Trypanosoma brucei. Retrieved April 25, 2011, from Parasite Museum: http://www.parasitemuseum.com/trypanosome/
[7] (2007). A well fed tse tse fly. Retrieved April 25, 2011, from Tanzania 2007 Safari: http://www.accuratereloading.com/hr20071.html
[8] Horn, D., and McCulloch, R. Molecular mechanisms underlying the control of antigenic
variation in African trypanosomes. Current Opinion in Microbiology 2010. 13:700–705.
[9] Dubois, M. E., Demick, K. P., Mansfield, J. M. Trypanosomes expressing a mosaic variant surface glycoprotein coat escape early detection by the immune system. Infection and Immunity 2005. 2690-2697.
[10] Dagenais, T. R., Freeman, B. E., Freeman, Demick, K. M., Paulnock, D. M., Mansfield, J. M. Processing and presentation of variant surface glycoprotein molecules to T cells in African trypanosomiasis. J Immunol 2009. 183(5): 3344–3355.
[11] Rudenko, G. Epigenetics and transcriptional control in African trypanosomes. Essays Biochem.. 2010. 20;48(1):201-19.
[12] Centers for Disease Control and Prevention (2010, November 2). Parasites – American Trypanosomiasis (also known as Chagas Disease). Retrieved April 1, 2011, from the CDC: http://www.cdc.gov/parasites/chagas/
[13] Wikipedia (2011, April 11). Neglected tropical disease research and development. Retrieved April 16, 2011, from Wikipedia: http://en.wikipedia.org/wiki/Neglected_Tropical_Disease_Research_and_Development
Edited by student of Joan Slonczewski for BIOL 238 Microbiology, 2011, Kenyon College.