Visceral Leishmaniasis (Kala azar)

Etiology/Bacteriology
Taxonomy
| Domain = [[Eukaryota]
| Phylum = Euglenozoa
| Class = Zoomastigophora
| Order = Kinetplastida
| Family = Trypanosomatidae
| Genus = ''Leishmania''
| species = donovani, infantum, and chagasi
Description
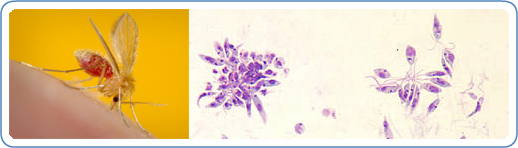
Visceral leishmaniasis is caused by the species Leishmania donovani and L. infantum/L. chagasi. These species are obligate intracellular protozoan parasites. This parasite resides in a sand fly vector. There are several different kinds of leishmaniasis. The most common types are cutaneous and visceral. Cutaneous leishmaniasis causes skin sores, while visceral leishmaniasis affects internal organs. The main internal organs it affects are the spleen, bone marrow, and liver. People who become infected with visceral leishmaniasis generally suffer from high fevers, weight loss, and enlarged liver and spleen. Visceral leishmaniasis is generally found in countries with tropic and subtropic climates. This disease is rarely seen in the United States. [1]
Pathogenesis
Transmission/Reservoirs
Visceral leishmaniasis is most commonly transmitted through the bite of an infected female phlebotomine sand fly. The infected stage of visceral leishmaniasis is called promastigotes. Less common forms of transmission include blood transfusions, contaminated needles, and from pregnant mother to her child. This does not form until two to eight months after the person has been bitten by an infected sand fly. Phelobotomine sandflies feed on the blood humans and animals, which allows them to develop their eggs. If a female phlebotomine sand fly bites an infected animal or human the next person who receives a bite from the sand-fly will be infected and develop into visceral leishmaniasis. Infected people are generally required to maintain the transmission of visceral leishmaniasis, but in some parts of the world this is not the case. Some areas are considered to be anthroponotic meaning that the transmission is from human to stand fly back to human. [2] [3]
CDC
Infectious Dose
The infectious dose is unknown. However, the number of parasites transmitted by an infected sand fly can influence the immune response. The higher the infectious dose the stronger the immune response which limits the spread of the parasite. This helps protect the patients visceral organs from infection. [4]
Incubation
The incubation period can be within months and as long as years. The average being around four to six months. [2]
Colonization
After being bitten by an infected sand fly, the promastigotes are phagocytized by host macrophages. The parasite is now able to turn the macrophage into amastigotes. Amastigotes is the tissue stage. After the parasite is in the tissue stage, it can proliferate to infect other mononuclear phagocytic cells in different tissues. The main organs infected include spleen, liver, and bone marrow. If left untreated it is a life threatening disease. [2]
Epidemiology
There are approximately 200,000 to 400.000 cases of visceral leishmaniasis every year. There are over 20,000 deaths annually. Over 90% of visceral leishmaniasis cases occur in the India, Bangladesh, Nepal, Sudan, South Sudan, Ethiopia and Brazil. Visceral leishmaniasis is not commonly found in the United States. If visceral leishmaniasis is found in the United States the person who contracted it traveled to other places where visceral leishmaniasis is common. The host range includes humans, wild rodents, and domesticated dogs. This disease in humans is reduced in areas where dog populations have been dramatically reduced. [2]
Virulence Factors
The exact virulence factors of visceral leishmaniasis are not completely understood. There is evidence that shoes that the virulence factors of visceral leishmaniasis include glicoinositolphospholipids (GIPLs), proteophosphoglycan (PPG), lipophosphoglycan (LPG), and the 11 kDa kinetoplastid membrane protein (KMP-11). This evidence comes from looking at the interactions between visceral leishmaniasis and the host immune system. Visceral leishmaniasis is able to enter macrophages by inhibiting protein kinase and nitric oxide synthase. Another potentially important virulence factor is proteinases. Proteinases are enzymes that are able to degrade proteins and peptides. [5]
Clinical Features
The clinical features of visceral leishmaniasis vary between adults and children. The most obvious sign of visceral leishmaniasis is the swelling/enlargement of the spleen. In the first two weeks to two months an adult will generally exhibit a fever along with symptoms of fatigue, weakness, and loss of appetite. As the patient weakens the disease becomes worse. Other symptoms of systematic visceral leishmaniasis can include a fever that continues for weeks and even be in cycles, night sweats, stomach pains, thinning hair, and graying of the skin. Visceral leishmaniasis can cause anemia, leukopenia, even and thromobocyopenia. If a child is infected with visceral leishmaniasis a child will most likely experience symptoms of cough, diarrhea, fever, and/or vomiting. [2] [6]

Diagnosis
In order to diagnosis visceral leishmaniasis, a sample from bone marrow of the infected patient is necessary. The bone marrow then can be examined under a microscope or in special cultures. Another way visceral leishmaniasis can be detected is through a blood test. This type of test can detect antibodies that the host immune system makes to defend itself against the pathogen. A quick way to detect visceral leishmaniasis is by polymerase chain reaction (PCR). Other ways of detecting visceral leishmaniasis by coagulation studies, liver function test, and peripheral blood smears. [7]
Treatment
A person infected with visceral leishmaniasis should consult with a infectious disease specialist. In order to achieve the best care, the treat should be individualized. There is no available vaccine for visceral leishmaniasis. If visceral leishmaniasis is left untreated it is almost always fatal. There are two foods and drug administration approved drugs. One is liposomal amphotericin B (AmBisome) and the other is an antimonial compound called pentostam. [2]
Prevention
There is no vaccines available to prevent people from visceral leishmaniasis It is important for people to avoid outdoor activities, especially in the evening and night, because this is when sandflies are most active. When outdoors in areas where visceral leishmaniasis is endemic, one should minimize the amount of exposed skin. It is important to wear long-sleeved. In the evening, it is highly recommended to use a sleeping net to keep the sandflies out and other potentially harmful vectors. Insect repellent is another way to help prevent contracting visceral leishmaniasis. [2]
Host Immune Response
Visceral leishmaniasis is characterized by certain organ immune responses. The liver is the sight of an acute infection that contains little tissue damage and less likely to be reinfected. The spleen on the other hand becomes very swollen and is a site where the parasite likes to reside. The infection impairs the T-cell mediated immune response by decreeing T helper 1 cytokine production. Both CD4+ and CD8+ T cells are activated and both T helper 1 and 2 responses are triggered. The CD4+ T cells are crucial factors in controlling the hepatic visceral leishmaniasis growth during the primary infection. The CD8+ T cells are important for quick resolution of the infection in the liver. Both CD4+ and CD8+ are crucial for having the best chance at fighting off the pathogen. [8]
References
- Leishmaniasis. Medline Plus.
- Parasites – Leishmaniasis. Center for Disease Control and Prevention. 2013 Jan. 10. Web.
- Kala Azar. Medecins Sans Frontieres. 2013 May 2nd.
- Leishmania spp. MSDS online. 2001 March.
- Silva-Almeida M., Pereira B., Ribeiro-Guimaraesand M., and Alves C. Proteinases as Virulence Factors in ‘Leishmania’ spp. Infection in mammals
- Leishmaniasis. PubMed Health. 2013 Sept. 1st.
- Strak C. Leishmaniasis. Medscape.
- Stanley A. and Engwerda C. G. Balancing Immunity and Pathology in Visceral Leishmaniasis. Immunology Cell Biology.
Created by Taylor Caswell
Student of Dr. Tyrrell Conway, University of Oklahoma
