A Review of Guillain-Barre Syndrome
Introduction
By Cassandra Lis

Guillain-Barré syndrome (GBS) is a rare disorder characterized by neuropathy that has a mortality rate of 4% to 7%.[1] The effects of Guillain-Barré syndrome are the most common cause of quadriparesis, or muscle weakness in all four limbs, in the world (1-2 cases per 100,000 people). Before 1979, the most common cause of quadriparesis was polio, but the introduction of the vaccine eradicated polio in the US and the rest of the world outside of Pakistan, Afghanistan, and Nigeria.[2] The underlying cause of GBS is believed to be the immune system attacking the nerves, so symptoms relating to nerve degeneration are normally the symptoms that are first noticed. Some of the symptoms of this disorder are weakness in legs, unsteady walking, feeling achy, shooting pain, high pulse, and labored breathing (See Figure 1). The most common first symptom is weakness and tingling in the lower extremities which later spreads to the upper body.
There are four main types of Guillain-Barré syndrome: acute inflammatory demyelinating polyradiculoneuropathy, Miller Fisher syndrome, Acute motor axonal neuropathy, and acute motor-sensory axonal neuropathy. Acute inflammatory demyelinating polyradiculoneuropathy (AIDP) is the type of Guillain-Barré that is most common in Europe and North America and people in these regions use GBS and AIDP interchangeably.[3] AIDP has three phases as it progresses, the first being rapidly worsening muscle weakness. After this stage, the muscle weakness becomes stable but other symptoms like cardiac disruptions or gastric dysmotility may occur.[3] In the final stage, these symptoms gradually fade away. However, many people experience weakness or pain for years after the syndrome.[3]
Miller Fisher syndrome (MFS) has a different characterization than AIDP. This syndrome is associated with unsteady ambulation, areflexia (loss of reflexes), and ophthalmoplegia (weakness of eye muscles).[4] MFS shares characteristics with Bickerstaff brainstem encephalitis, which impacts the central nervous system more than MFS does. People who have had MFS normally recover within a few months, but there are also numerous patients who display other forms of GBS in addition to the MFS. In these overlapping cases, respiratory failure is also a common side effect.[4]
Acute motor axonal neuropathy (AMAN) is less common in western countries, but accounts for 30% to 50% of Guillain-Barré syndrome cases in both Asia and Latin America.[5]This form of GBS is more severe in its onset of weakness and poor reflexes than AIDP. Many patients with this form of GBS need assistance with respiration, which is achieved through the use of a ventilator.[5] AMAN onset is often associated with enteritis caused by Campylobacter jejuni. Recovery in AMAN differs from the other forms of GBS because it can occur much quicker. However, if the person has severe axonal degeneration, the recovery process is longer.[5]
Acute motor-sensory axonal neuropathy (AMSAN) is similar to AMAN in both its proposed pathological mechanism and symptoms. However, this disease is very severe, so the recovery process is very difficult and it does not have a good prognosis.[6] This is because the illness affects the sensory nerves and roots, which causes motor and sensory dysfunction.[6]
Guillain-Barré syndrome has many different causes, and the majority of them are bacterial or viral in nature. Campylobacter jejuni, influenza virus, cytomegalovirus, Epstein-Barr virus, Zika virus, Hepatitis A/B/C/E, HIV, mycoplasma pneumonia, surgery, Hodgkin’s lymphoma, vaccinations (very rarely), and COVID-19 infections are all believed to trigger the syndrome.[7] Although these can trigger Guillain-Barré syndrome, the actual underlying cause of this disorder is unknown. It does not spread between people and it is not a heritable illness.[7] The specific mechanisms of the disease are currently being investigated and are of high interest in the medical community.
Current research is finding that several medicines are also associated with the onset of forms of GBS. For example, a 2019 case study finds that rivaroxaban, also known as xarelto, may be associated with GBS.[2] Rivaroxaban is a commonly used anticoagulant, which prevents deep vein thrombosis, strokes, and heart attacks. The patient in the case study had a history of diabetes, and they developed quadriparesis after 5 days of treatment with rivaroxaban. Nerve conduction studies found that there was a reduction in amplitude for both the tibial and right peroneal nerves.[2] There was also reduced sensory nerve action potential in the right ulnar nerve. These findings indicated that the patient was experiencing demyelinating neuropathy. The surprising finding about this patient was that there were no recent records of infection or vaccinations, which indicated that something new or unknown caused the onset of GBS.[2] Rivaroxaban was stopped and the patient was treated with intravenous immunoglobulin and neurorehabilitation to combat the GBS. He was able to walk after 2 months of stopping the rivaroxaban. The reason why rivaroxaban causes GBS is unknown, but it is likely that there was an allergic reaction to the drug or a neurotoxin effect that caused demyelination.[2]
Pathological Mechanisms

The specific pathological mechanisms of Guillain-Barré syndrome are currently being investigated in order to determine what potential ways physicians can combat the illness. One of the ways that researchers are investigating the mechanisms is by determining what specific infections or illnesses are associated with the onset of GBS. A 2016 study found, using blood samples, that Zika virus was associated with the development of GBS.[8] Researchers discovered that none of the people with GBS were actively sick with Zika virus at the time of their admittance to the hospital, indicating that people who were actively contagious with Zika virus were not able to also acquire GBS.[8] The researchers were able to determine that the patients had recently had a Zika infection by the presence of IgM or IgG antibodies in ELISA assays. All of the patients were diagnosed with the AMAN type of GBS in this study. Less than 50% of people with GBS had an immune response against glycolipids, which is different from the reported cases of people with GBS after Campylobacter jejuni infections.[8]
Other research is investigating specifically how these infections cause GBS. AIDP is believed to be associated with macrophages invading the myelin sheaths and destroying the axons.[9][3] This is what occurs in autoimmune neuritis, which is caused by the T cells attacking myelin proteins P0, P2, and PMP22.[9] When this occurs in patients with AIDP, it is known as multifocal peripheral demyelination (See Figure 3). Another pathological characteristic of patients with AIDP is the slow remyelination of their peripheral nerves. AIDP is the most researched in terms of its pathological mechanisms due to its abundance compared with other types of GBS. MFS is associated with the presence of antiganglioside antibodies against gangliosides GQ1b, GD3, and GT1a.[9][4] AMAN is associated with antibodies against GM1, Gd1a, GaINAc-GD1a, and GD1b. AMAN is very strongly associated with C. jejuni infections, especially in the summer months.[9]

One in every 1,000 to 5,000 people with C. jejuni infections will develop a form of GBS in the next 2 months.[10] C. jejuni infections are believed to cause GBS through the production of antibodies that react with gangliosides. It is proposed that the lipo-oligosaccharides on the outer membrane of the C. jejuni cause the body to produce these antibodies (See Figure 4).[11] In patients with AMAN, the antibodies bind to the nodal axolemma, which can lead to detachment of myelin. This causes nerve conduction failure, which then creates the symptoms that patients with AMAN experience.[11]In patients with AIDP, however, the target of the antibodies is not known, but it is believed to be on the myelin sheath. The binding of the antibodies leads to the formation of the MAC, membrane attack complex, and the destruction of myelin by macrophages.[11]
Currently, more people are investigating COVID-19 and its relation to Guillain-Barré syndrome. An Italian 2020 study found that a woman developed GBS after having COVID-19.[12]Unlike the Zika study, this woman was actively sick with COVID-19 when she began presenting symptoms of GBS.[12] IVIg treatment (the typical treatment for patients with GBS, discussed later) was not effective for her. She required both intubation and ICU admission where she went into multi-organ failure and developed deep vein thrombosis in her leg.[12] It is important for researchers to continue to study both the mechanisms and the causes of GBS, as there have been over 30 million people who have of people in the US who have had COVID-19.[13] Because people can develop GBS from COVID-19, it is important for physicians to understand the unique symptoms of these patients and what the best way to treat them for both illnesses is.
Diagnosis
GBS is difficult to diagnose because many of the symptoms of GBS are similar to the symptoms of other disorders. This means that physicians often find that they must rule out many other diseases or illnesses before they are able to diagnose the patient with GBS. After physicians do a complete history and physical examination, they might draw complete blood counts and metabolic panels for labs as a quick way to eliminate other disorders. The specific diagnostic criteria for GBS include a progressive symmetrical weakness with decreased reflexes.[14] The peak of the symptoms must also occur within four weeks of the onset of the symptoms. Each type of GBS has differing symptoms, so the specific diagnosis of a patient is informed by the symptoms that they are experiencing.
One of the ways that physicians diagnose GBS is through a spinal tap. In a spinal tap, fluid is drawn from the spinal canal. The fluid is then tested by other means in order to determine if the patient has GBS. In the fluid, physicians look for increases in protein with a normal white blood cell count.[15] This is known as albuminocytologic dissociation and is found in 9 of 10 GBS patients. If the patient has elevated lymphocyte counts, this might indicate other issues like sarcoidosis or Lyme disease neuropathy.[15]

Another way that GBS may be detected is through nerve conduction studies. This is a study where electrodes are placed on the skin above the nerves and small shocks are passed through the different electrodes. This measures the speed of the nerve signals as the shocks travel from nerve to nerve.[1] These are especially useful because they allow physicians to differentiate between the different types of GBS.[15] Physicians are able to distinguish between the different types because AIDP is characterized by conduction slowing, conduction blocks, and abnormal temporal dispersion but patients with AMAN have reduced compound muscle action potential amplitudes.[16] Electromyography is another study that uses electrodes that can also help to diagnose someone with GBS. In this study, electrodes are inserted into the muscles in order to measure nerve activity at that specific muscle.[1]
One of the specific ways that diagnosing patients with Guillain-Barré syndrome can be complicated is because about 8% of patients present with paraparesis, which is the paralysis or weakness of both legs.[17] This can make diagnosis difficult because previous criteria state that progressive quadriparesis is typical of GBS. Guillain-Barré syndrome is an extremely complicated condition that affects people in different ways. For this reason, better diagnostic methods are needed in order for physicians to be able to readily recognize and treat patients with GBS, especially when treating children. Only ⅓ of children receive a correct diagnosis of GBS upon admission to the hospital. Children with GBS are often misdiagnosed with conditions like meningitis, coxitis, or malaise.[18] Misdiagnosis is extremely harmful and can result in people being intubated as a result of not receiving treatment quickly enough.
Researchers are investigating diagnosing patients with Guillain-Barré syndrome through testing for antiganglioside antibodies. The exact role of antiganglioside antibodies in the pathogenesis of GBS is being investigated, but researchers believe that the presence of anti-GQ1b, anti-GM1, and anti-GD1a IgG antibodies could be used in the diagnosis of GBS.[19][20] Many antibodies are present when a patient has other diseases, but these three antibodies appear to be more specific to GBS (See Figure 5). Therefore, these could potentially be used in making future diagnoses, especially as antibody detection methods are becoming more accurate and sensitive.
Treatment
Guillain-Barré syndrome has no cure but there are different treatments to manage the condition. One of the treatments is known as plasmapheresis, which is plasma exchange. This is when the plasma is removed from the patient’s body and separated from the blood cells. The blood cells are then infused back into the body and the body makes more plasma to replenish what was lost. The reason why this treatment works is because it removes antibodies from the plasma that were inducing the Guillain-Barré syndrome.[7]Another treatment, known as immunoglobulin therapy, is used to give people with Guillain-Barré syndrome healthy antibodies to replace the antibodies that can be causing the GBS.[1] Both of these treatments have the same effectivity if they are started within two weeks of onset of symptoms (See Figure 6). There is also no benefit for the patient to receive both plasmapheresis and immunoglobulin therapy.[7]

IVIg has become the favored treatment option for high-income countries because it has less side effects and does not require special medical equipment.[11] IVIg, however, is much more expensive than plasmapheresis, which is one of the reasons why plasmapheresis is still used. Plasmapheresis may also be more effective in treating AMAN than treating patients with AIDP.[21]It is largely unknown whether the different types of GBS should be treated differently, especially because little research has been done to examine how physicians should treat MFS.[22] There has also been no large-scale controlled studies to examine how children with Guillain-Barré syndrome should be treated. Because of this, children with GBS are treated with the same methods adults are, IVIg and plasmapheresis.[23]
Researchers are also investigating novel treatments for Guillain-Barré syndrome. For example, a 2007 study examined using mycophenolate mofetil (MM) in addition to IVIg (intravenous immunoglobulin) and methylprednisolone (MP) to treat GBS.[24] However, the outcomes with the addition of MM were not better than the treatment group that was treated with IVIg and MP.[24] Corticosteroids have also proven ineffective in treating patients with Guillain-Barré syndrome.[25] New medicinal treatments are needed because approximately 10% of patients treated with IVIg deteriorate after improvement. This is known as treatment-related fluctuation. Patients who experience this are still recommended to receive retreatment with IVIg, as there are limited options in terms of other treatments.[26]
Some of the other medicines that are given to the patients are meant to combat the side effects of being immobile for long periods of time. For example, many patients receive anticoagulants in order to prevent blood clots.[1] They might also receive intravenous pain medicine in order to alleviate the pain that is associated with Guillain-Barré syndrome.[1] In addition, 25% of patients with GBS need to be intubated.[11] As the patients are recovering from GBS, many are also forced to utilize adaptive devices like wheelchairs and braces. In addition to the assistive devices, many people also undergo physical therapy in order to relearn how to walk or perform certain movements.[1]
There are many residual effects of Guillain-Barré syndrome, and these largely impact the lives of people who have survived the disease. Some of the major residual effects are reduced strength, fatigue, and pain.[11] Other residual issues like tachycardia, hypertension, gastrointestinal dysfunction, and bladder dysfunction have also been observed in patients who have recovered from GBS.[27]
Controversies with Vaccines
Although GBS is very rare, people are still concerned about acquiring this illness as a side effect of vaccines. This is because in 1976, there was an increase in GBS cases after receiving the swine flu vaccine.[28] However, the risk of acquiring GBS after the swine flu vaccine was about 1 case for every 100,000 people who got the 1976 swine flu vaccine. The reason why this occurred is unknown. The CDC monitors the number of people with Guillain-Barré syndrome during flu season in order to see if there is a larger association between GBS and the flu vaccine. Each year, the risk of developing Guillain-Barré syndrome from an influenza vaccine is between 1 to 2 people per one million vaccinated. However, it is much more likely that a person could develop GBS after getting the flu compared with the vaccine. On the CDC information sheet for the influenza vaccine, Guillain-Barré syndrome is mentioned as a potential side effect of the vaccine, and it is recommended that a person who previously had GBS speak with their healthcare provider before receiving the vaccine.[29]
Risks of vaccination are very important to consider because many people use these potential side effects as justification for not receiving vaccinations. According to a 2020 study, the number of anti-vaxxers, people who oppose receiving vaccines, has increased by at least 7.8 million people since 2019.[30]This was determined using the presence of social media accounts and followers of social media that spread anti-vaccination sentiments. In addition, approximately 1 in 6 British people were unlikely to get vaccinated against COVID-19. Currently, the world needs to vaccinate as many people as possible to create herd immunity and prevent the spread of COVID-19 and protect people against harmful mutants that are beginning to develop.
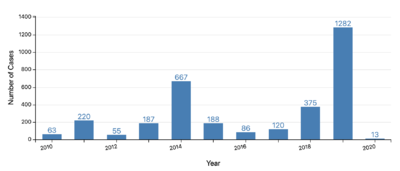
Anti-vaxxers spread misinformation about the likelihood of developing GBS and other conditions after vaccination in order to scare other people into not receiving vaccines. This is very harmful to everyone because there are many people who are unable to receive either due to allergies like latex or religious reasons. One of the religious reasons that Muslim people, for example, do not receive some vaccinations is because they contain gelatin, which is a pork product. When anti-vaxxers refuse to vaccinate their children, they are disrupting the herd immunity that scientists have developed by vaccinating the majority of the population. This is done to protect people who are unable to receive vaccinations. If more parents refuse to vaccinate their children, then the people who are unable to be vaccinated will be at higher risk of developing the illness. For example, in the US there were 1282 cases of measles in 2019, which was a large increase from the previous year (see Figure 7).[31] The number of cases went down in 2020, but this was likely due to people wearing masks and social distancing because of COVID-19. In order to protect vulnerable populations, everyone who is eligible should be vaccinated. Scientists can promote vaccinations by making the information about them easily accessible to people who did not study science.
Conclusion
Guillain-Barré syndrome is a rare disorder that is characterized by muscle weakness and loss of reflexes. The pathological mechanisms of the different types of these diseases are being investigated, but there are still many questions that need to be explored about different aspects of the disease. It is treated with plasmapheresis and immunoglobulin therapy, but more effective methods of treatment are required. Nerve regeneration is another area that is of interest in order to treat patients who have long term effects from Guillain-Barré syndrome.
In order to better treat patients with Guillain-Barré syndrome, more research is needed in both the potential medicinal therapies and the pathological mechanisms of the disease. Once scientists better understand how Guillain-Barré is caused, they will be better able to treat the disease. It is also necessary that scientists learn the mechanisms of GBS because of the severe consequences of the disorder-- 25% of patients require intubation and 20% are unable to walk after 6 months.[11] Physicians also need better diagnostic criteria for diagnosing the illness. The sooner physicians are able to diagnose and treat a patient with GBS, the sooner the patient’s pain and symptoms can be alleviated. In addition, it might prevent the disease from progressing to the point that the patient requires intubation. If scientists are able to better understand what causes Guillain-Barré syndrome and treatments become more efficient, this could assuage the fears of people who refuse to be vaccinated.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Guillain-Barre syndrome. (2020, September 17). Retrieved April 01, 2021.
- ↑ 2.0 2.1 2.2 2.3 2.4 Karri, M., Ramasamy, B., & Perumal, S. (2019). Rivaroxaban: A possible cause of guillain–barre syndrome. Annals of Indian Academy of Neurology, 22(2), 242-244. doi:10.4103/aian.aian_331_18.
- ↑ 3.0 3.1 3.2 3.3 Orphanet: Acute inflammatory demyelinating polyradiculoneuropathy. (n.d.). Retrieved April 07, 2021.
- ↑ 4.0 4.1 4.2 Orphanet: Miller Fisher syndrome. (n.d.). Retrieved April 07, 2021.
- ↑ 5.0 5.1 5.2 Orphanet: Acute Motor Axonal neuropathy. (n.d.). Retrieved April 07, 2021.
- ↑ 6.0 6.1 Orphanet: Acute motor and sensory Axonal neuropathy. (n.d.). Retrieved April 07, 2021.
- ↑ 7.0 7.1 7.2 7.3 Guillain-Barre Syndrome. (n.d.). Retrieved April 07, 2021.
- ↑ 8.0 8.1 8.2 [Cao-Lormeau, V., Blake, A., Mons, S., Lastère, S., Roche, C., Vanhomwegen, J., . . . Ghawché, F. (2016). Guillain-Barré syndrome outbreak associated with Zika virus infection in French Polynesia. The Lancet, 387(10027), 1483-1590. doi:10.1097/01.ogx.0000489564.35748.52
- ↑ 9.0 9.1 9.2 9.3 Hughes, R. A., & Cornblath, D. R. (2005). Guillain-Barré syndrome. The Lancet, 366(9497), 1653-1666. doi:10.1016/s0140-6736(05)67665-9.
- ↑ Tam, C., Rodrigues, L., Petersen, I., Islam, A., Hayward, A., & O’Brien, S. (2006). Incidence of Guillain‐Barré syndrome among Patients withCampylobacterInfection: A general Practice research Database Study. The Journal of Infectious Diseases, 194(1), 95-97. doi:10.1086/504294
- ↑ 11.0 11.1 11.2 11.3 11.4 11.5 11.6 Van den Berg, B., Walgaard, C., Drenthen, J., Fokke, C., Jacobs, B. C., & Van Doorn, P. A. (2014). Guillain–Barré syndrome: PATHOGENESIS, diagnosis, treatment and prognosis. Nature Reviews Neurology, 10(8), 469-482. doi:10.1038/nrneurol.2014.121
- ↑ 12.0 12.1 12.2 Ottaviani, D., Boso, F., Tranquillini, E., Gapeni, I., Pedrotti, G., Cozzio, S., . . . Giometto, B. (2020). Early Guillain-Barré syndrome in CORONAVIRUS disease 2019 (COVID-19): A case report from an ITALIAN COVID-HOSPITAL. Neurological Sciences, 41(6), 1351-1354. doi:10.1007/s10072-020-04449-8.
- ↑ CDC COVID Data Tracker. (n.d.). Retrieved April 07, 2021.
- ↑ Anne, and Gretchen Dickson. Guillain-Barre Syndrome. American Family Physician, vol. 87, no. 3, Feb. 2013, pp. 191–97.
- ↑ 15.0 15.1 15.2 Olshansky, Adel. Diagnosis and Treatment of Guillain-Barre Syndrome. AMA Journal of Ethics, vol. 9, no. 8, American Medical Association, Aug. 2007, pp. 552–54. journalofethics.ama-assn.org, doi:10.1001/virtualmentor.2007.9.8.cprl1-0708.
- ↑ Rath, J., Schober, B., Zulehner, G., Grisold, A., Krenn, M., Cetin, H., & Zimprich, F. (2021). Nerve conduction studies in guillain-barré syndrome: Influence of timing and value of repeated measurements. Journal of the Neurological Sciences, 420, 117267. doi:10.1016/j.jns.2020.117267
- ↑ Fokke, C., Van den Berg, B., Drenthen, J., Walgaard, C., Van Doorn, P. A., & Jacobs, B. C. (2013). Diagnosis of Guillain-Barre syndrome and validation of Brighton criteria. Brain, 137(1), 33-43. doi:10.1093/brain/awt285
- ↑ Roodbol, J., De Wit, M. C., Walgaard, C., De Hoog, M., Catsman-Berrevoets, C. E., & Jacobs, B. C. (2011). Recognizing Guillain-Barre syndrome in preschool children. Neurology, 76(9), 807-810. doi:10.1212/wnl.0b013e31820e7b62
- ↑ Chiba, A., Kusunoki, S., Shimizu, T., & Kanazawa, I. (1992). Serum IgG antibody to ganglioside GQ1b is a Possible marker of Miller Fisher syndrome. Annals of Neurology, 31(6), 677-679. doi:10.1002/ana.410310619
- ↑ Yuki, N., Ho, T., Tagawa, Y., Koga, M., Li, C., Hirata, K., & Griffin, J. (1999). Autoantibodies to GM1b And GALNAC-GD1A: Relationship to Campylobacter JEJUNI infection and Acute Motor Axonal neuropathy in China. Journal of the Neurological Sciences, 164(2), 134-138. doi:10.1016/s0022-510x(99)00056-8.
- ↑ Dada, M. A., & Kaplan, A. A. (2004). Plasmapheresis treatment in guillain-barre syndrome: Potential benefit over ivig in patients with axonal involvement. Therapeutic Apheresis and Dialysis, 8(5), 409-412. doi:10.1111/j.1526-0968.2004.00183.
- ↑ Overell, J. R., Hseih, S., Odaka, M., Yuki, N., & Willison, H. J. (2007). Treatment for fisher syndrome, BICKERSTAFF'S brainstem encephalitis and related disorders. Cochrane Database of Systematic Reviews. doi:10.1002/14651858.cd004761
- ↑ Ryan, M. M. (2005). Guillain-Barre syndrome in childhood. Journal of Paediatrics and Child Health, 41(5-6), 237-241. doi:10.1111/j.1440-1754.2005.00602.
- ↑ 24.0 24.1 Treatment of guillain-barré syndrome with high-dose immune globulins combined with methylprednisolone: A pilot study. (1994). Annals of Neurology, 35(6), 749-752. doi:10.1002/ana.410350618
- ↑ Hughes, R. A., Brassington, R., Gunn, A. A., & Van Doorn, P. A. (2016). Corticosteroids for GUILLAIN-BARRÉ SYNDROME. Cochrane Database of Systematic Reviews. doi:10.1002/14651858.cd001446.pub5
- ↑ Kleyweg, R. P., & Van der Meche, F. G. (1991). Treatment related fluctuations in guillain-barre syndrome after high-dose immunoglobulins or plasma-exchange. Journal of Neurology, Neurosurgery & Psychiatry, 54(11), 957-960. doi:10.1136/jnnp.54.11.957
- ↑ Ruts, L., Drenthen, J., Jongen, J. L., Hop, W. C., Visser, G. H., Jacobs, B. C., & Van Doorn, P. A. (2010). Pain in GUILLAIN-BARRE syndrome: A long-term follow-up study. Neurology, 75(16), 1439-1447. doi:10.1212/wnl.0b013e3181f88345
- ↑ GBS (GUILLAIN-BARRÉ syndrome) and vaccines. (2020, August 14). Retrieved April 01, 2021.
- ↑ Influenza (Flu) Vaccine (Inactivated or Recombinant): What you need to know. (2019, October 15).
- ↑ Burki, T. (2020). The online anti-vaccine movement in the age of covid-19. The Lancet Digital Health, 2(10).doi:10.1016/s2589-7500(20)30227-2.
- ↑ Measles cases and outbreaks. (2021, March 08). Retrieved April 01, 2021.
Authored for BIOL 238 Microbiology, taught by Joan Slonczewski, 2021, Kenyon College.
