User:Cenizalevine1
Introduction
Human treponemal diseases, including the sexually transmitted infection syphilis, have existed as early as the fifteenth century. The exact origins of syphilis are unknown– there is considerable debate as to whether Christopher Columbus spread syphilis to different parts of the world on his voyages, or if syphilis was already present in different parts of the world before his travels. In the early twentieth century, two scientists named Schaudinn and Hoffman identified the bacterium that causes syphilis, and they named it Treponema Pallidum.
Genome
Phylum: Spirochaets
Order: Spirochaetales
Family: Spirochaetaceae
Subspecies and the infection it causes:
- Pallidum: syphilis
- Endemicum: bejel (endemic syphilis)
- Carateum: pinta
- Pertenue: yaws
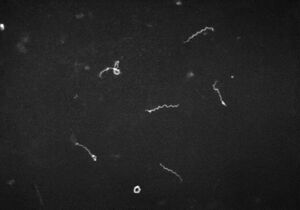
Genome sequencing: T. pallidum cannot be visualized by bright-field microscopy, and scientists have had difficulties culturing it in a lab. For this reason, much of our information on T. pallidum comes from dark-field, fluorescence, and electron microscopy, genome sequencing (4). The genome of the Nichols strain of T. pallidum was sequenced in 1998, and then resequenced in 2013. The results showed that T. pallidum has a circular chromosome of approximately 1,139,000 base pairs and over one thousand open reading frames. The average gene length of each gene is 1,023 base pairs (3). The genome of T. Pallidum is smaller compared to other prokaryotic genomes– it has only a fourth of the base pairs of E. Coli (1). The T. pallidum genome is small because it has evolved to stop producing enzymes for the tricarboxylic TCA cycle. The TCA cycle converts sugar into water and carbon dioxide. Since T. pallidum does not have that ability, it relies on a host for amino acid production (4).
Metabolism: T. Pallidum’s ability to synthesize its own materials is limited; its genome does not have many of the enzymes required for biosynthesis (1)(3). Therefore, it relies on transporter proteins that can take nutrients from its host and environment. 5% of T. Pallidum’s ORFs code for eighteen transporters (1). Survival outside of the host is very limited. T. Pallidum is capable of glycolysis to produce ATP, though its glycolytic pathway is slightly modified from other bacteria. T. pallidum uses a phosphofructokinase instead of an ATP-dependent enzyme– which saves T. Pallidum ATP.
In vitro fertilization: For almost a century, researchers struggled to cultivate T. pallidum in vitro. Long term in vitro was finally achieved in 2017. The Nichols strain of T. pallidum can be cultured in vitro indefinitely in rabbits, or co-cultured in vitro with rabbit cells, provided it is supplied with the right amount of oxygen and carbon dioxide. After examining the genome of T. pallidum in rabbits compared to its genome in vitro, researchers found very minimal changes to the overall genome. However, transcription levels varied significantly, suggesting that T. pallidum can react to its surroundings in limited contexts (5). Notably, transporter proteins and flagellar proteins were expressed at similar levels in vitro and in rabbits, suggesting that such capabilities are not affected by the external environment (3).
Gene expression: Gene expression varies widely across the chromosome, but transcription was found to be highest in an area responsible for a ribosomal protein operon (3). Other genes that were highly expressed in T. pallidum included genes for proteins associated with metabolism, motility, and the cell envelope (3)(5). Such genes are what allow T. pallidum to be highly virulent.
Virulence factors
The outer membrane is a major factor that contributes to T. pallidum’s virulence. Its outer membrane lacks lipopolysaccharide (LPS), which is often found in gram-negative bacteria. The lipoproteins that T. pallidum does have are often below the surface of the cell. In general, T. pallidum does not have many pathogen-associated molecular patterns (PAMPs) on its surface. TprK allows the few outer membrane proteins of its genome to have varying antigens. For these reasons, T. pallidum can repeatedly enter and infect a host multiple times before being identified as a threat.
T. pallidum has a flexuous, flat-wave morphology that allows it to more easily penetrate and go deep into the tissue. This increases the space and opportunities that T. pallidum has to infect the host.
Adherence to the host cell and binding to the extracellular matrix is necessary for transmission. T. pallidum is able to complete that function because it has many adhesins, including fibronectin-binding proteins, laminin-binding proteins, and BamA, which puts outer membrane proteins into the outer membrane.
T. pallidum is very motile, and that is what allows it to enter and infect host cells. The Nichols genome has thirty-six genes relating to flagellar structure and function, expressed across four different operons.
Infection and Treatment
Stages of Infection
Primary syphilis: This period lasts about 2-4 weeks and is associated with a chancre– an ulcer at the site of the infection. It is small (about a center in diameter), hard and painless. After a few weeks it will heal and scar over, because the macrophages cause the treponemas to undergo phagocytosis. Once the chancre has healed, the syphilis is considered to be in a latent stage. The infected person may be asymptomatic for up to five years.
Secondary syphilis: defined by a rash over the whole body, particularly around the palms of the hand and feet; the rash will eventually crust over. The which rash resembles the rashes of other illnesses (giving syphilis its nickname as the “great imitator.”) The rash is caused by “bacterial intrusion in blood and lymph nodes.” Other symptoms of secondary syphilis include pyrexia, body pains, fatigue, fever and sore throat. At this point, the patient can still respond to antibiotics. If untreated, 70% of infected persons will enter the latent period; the other 30% will progress to tertiary syphilis.
Tertiary syphilis: This stage is associated with cardiovascular symptoms, such as aneurysms, and neurological symptoms, such as seizures, blindness, and meningitis. At this stage the patient may have gummas– necrotic granulomatous lesions– on their skin and bones. In some cases the patient will die.
Latent stage: The infected person is asymptomatic but can still test positive on serological tests. The latent stage is considered early within one year of infection, and it is considered late past one year of infection.
Include some current research, with at least one figure showing data.
Diagnosis and Screening:
Direct detection: To diagnose patients with syphilis, doctors will often use dark-field microscopy to identify the presence of T. pallidum directly. The method is fairly effective, though there are limits. The accuracy of the diagnosis depends on the lesions and the skill of the microscopist, and there are certain areas of the body that dark-field microscopy cannot examine. Direct fluorescent antibody tests and nucleic-acid amplification tests can also be used to detect T. pallidum, but they are more often used in research labs.
Serological Test for Syphilis (STS): Such tests are affordable, easy to obtain, and give results quickly. However, they are known for false positives and are not sensitive to primary or tertiary syphilis. For this reason, it is common practice in the U.S. to use multiple STSs to confirm a syphilis diagnosis– one non-treponemal test and one treponemal STS.
history of treatment
Section 3
Include some current research, with at least one figure showing data.
Section 4
Conclusion
References
Authored for BIOL 238 Microbiology, taught by Joan Slonczewski, 2023, Kenyon College