Cholera

Etiology/Bacteriology
Taxonomy
Domain: Bacteria | Phylum: Proteobacteria | Class: Gamma Proteobacteria | Family: Vibrionaceae | Order: Vibrionales | Genus: Vibrio | Species: Vibrio cholerae
|
NCBI: Taxonomy Genome: Vibrio cholerae |
Description
Cholera is a water and food borne disease caused by enteric pathogen Vibrio cholerae. It is most prevalent in underdeveloped countries with poor or no water sanitation techniques. It affects 3-5 million people per year and kills about 100,000 to 120,000 people among those affected. Cholera is only detrimental if left untreated, with the ability to kill an infected person within hours. It has a short incubation period ranging from a couple of hours to 5 days. It works by using an A-B toxin mechanism to invade host cells and replicate. Symptoms include dehydration from diarrhea and vomiting. Onset of cholera can be identified by its distinctive "rice water stool" although some cases may remain asymptomatic. Treatment includes rehydration via oral salts and intravenous hydration in moderate to severe cases. Antibiotics are prescribed for severe cases to prevent the spread of the pathogen [9]. Transmission is due to interaction or ingestion of fecal contaminated waters or seafood that harbors V. cholerae. Preventative measures include adequate hygiene, water sanitation, safe food preparation, and avoiding undercooked seafood. The Sari Filtration technique can be applied to adequately filter water of zooplankton and copepods that carry V. cholerae. The host response allows for immunological memory to protect against reinfection [13].
Pathogenesis
Transmission
The first recorded outbreak of cholera occurred in India in 1817, near the mouth of the Ganges River [5]. Vibrio cholerae naturally attach to the chitinous exoskeleton of zooplankton in fresh, brackish rivers and coastal salt water. Due to this mechanism, cholera outbreaks often coincide with zooplankton blooms [6]. The transmission of V. cholerae usually occurs through water and food contaminated with zooplankton or fecal matter. Because the pathogen is ingested, it is also transmitted through oral-fecal transmission. The transmission of V. cholerae is often related to the inadequate sanitation and water treatment procedures of an area [7].”

Infectious dose, incubation, and colonization
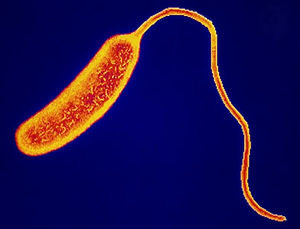
V. cholerae lacks the acid resistance genes found in many other intestinal pathogens and therefore has a high infectious dose. One must ingest over one million microbes in order to contract cholera because many of the bacteria will die in the stomach due to its highly acidic environment. The incubation period is dependent upon how many organisms successfully passed through the stomach into the small intestine where V. cholerae can colonize. Therefore, the incubation period before showing symptoms ranges from a few hours to five days, typically taking two days before causing symptoms. Once in the small intestine, studies show that some of the bacteria use their flagella to swim towards the epithelial cells and adhere in the crypts of the intestine using a toxin-coregulated pilus to keep from being flushed out [8].
Epidemiology
Cholera outbreaks typically occur in areas with inadequate sanitation and poor water treatment, which leads to drinking water contaminated with fecal matter . Individuals living in poorer areas without access to proper sanitation or water sources are at higher risk of infection. Consequently, Cholera outbreaks can become a serious threat in displacement camps, slums, and disaster zones when few sources of water are available. Water resources are often contaminated with Vibrio cholerae after natural disasters such as a floods, hurricanes, and Tsunamis. Cholera epidemics have been a a major concern during the recovery period following a natural disaster, much like the 2008 hurricane in Haiti [9].
Epidemiological studies of cholera typically focus on determining the common contaminated water source. John Snow first established this method of evaluation when studying London neighborhood water sources after an outbreak in 1854. In fact, much of what we now know about cholera came from John Snow's study on the communication of cholera [10] Often referred to as the first epidemiological study, Snow visited the infected neighborhoods, asking people about their habits, and marking infected homes on a map. From his conversations and speculation as to the transmission of the infection, Snow deduced the site of initial contamination to be a well located on Broad Street, a common water source for the infected neighborhoods. [11]
Virulence factors
The virulence factors of V. cholerae include toxin co-regulated pillus, cholera toxin, and motility. All of these factors contribute to the pathogenicity of the bacteria. Without one or more of these factors, V. cholerae would lose much of its ability to infect and cause symptoms in the host.
Motility
V. cholerae have flagella, which make them motile. This flagella allows the bacteria to swim through the lumen of the small intestine in search of nutrient rich cells and places to adhere to the epithelial cells that make up the lining of the small intestine, specifically the crypts of the small intestine. This motility could also be an important factor in the bacteria breaking through the mucosal layer that coats the inside of the small intestine [8].
Adherence

The virulence factor that contributes to the adherence of V. cholerae in the small intestine Toxin Co-regulated Pilus (TCP). The expression of TCP is linked with the production of Cholera Toxin (CT). The TCP is a Type IV pili, which are found on all gram-negative bacteria [16]. It is possible that V. cholerae could use this immune response to establish its own niche in the small intestine, similar to Salmonella, but scientists are not entirely sure. These pili are located on the polar ends of the cell and likely contribute to colonization via direct adherence to the epithelial cells lining the small intestine or through other pilus-mediated bacterial interactions. The host cell receptors for TCP have yet to be identified, and the mechanism for attachment is still largely unknown [17].
Toxin Mechanism
Cholera toxin is an A-B toxin secreted by V. cholerae that causes the host cell to expel large amounts of water and ions. The toxin is made up of five identical B subunits linked to one A subunit. The B subunits bind to monosialosyl ganglioside present on the surface of intestinal mucosal cells, allowing the A subunit to enter the cell. Once inside the cell, the A subunit stimulates heightened formation of cAMP by transferring an ADP-ribosal moiety of NAD to a protein that regulates the adenylate cyclase system [17]. The regulation protein inactivates the system when GTP is hydrolyzed. The A subunit essentially keeps GTP hydrolysis from occurring by affecting other proteins.
The high level of cAMP in the cell activates mucosal membrane pumps to push Cl- ions into the lumen of the small intestine. This creates an ionic gradient between the host cell and the lumen. This gradient causes the cell to expel large amounts of water and positively charged ions (electrolytes) into the lumen to counteract the negative charge of the Cl- ions [17]. The water and electrolytes expelled are replaced by the bloodstream and subsequently pumped out of the cell once more. This can lead to severe dehydration in the host if left untreated.
Clinical features
Symptoms
Most cholera infections are asymptomatic in nature. Only 5-10% of those infected will display the severe symptoms that are characteristic of cholera [23]. Cholera can still be spread from asymptomatic carriers, as the bacteria will be shed for 7-14 days [24]. The typical symptoms of cholera include diarrhea, nausea and vomiting, and dehydration. The most serious of these symptoms is the diarrhea, which leads to dehydration.
The diarrhea associated with cholera is very distinct and often called "rice water stool" because of its pale, milky white appearance, which is what water looks like after having washed rice with it. Fluid loss from this symptom can reach up to one quart an hour. This outflow of fluid and electrolytes accompanied with vomiting can lead to severe dehydration and electrolyte imbalance in those infected. The symptoms of severe dehydration as stated by Mayo Clinic include irritability, lethargy, sunken eyes, a dry mouth, extreme thirst, dry and shriveled skin that's slow to bounce back when pinched into a fold, little or no urine output, low blood pressure, and an irregular heartbeat (arrhythmia). Electrolyte imbalance can lead to muscle cramps due to lack of salts in muscle tissue and shock, which is one of the most severe symptoms of dehydration and electrolyte imbalance. This drop of blood pressure and oxygen in the body will lead to hypovolemic shock and subsequently death in a matter of minutes.
In addition to the symptoms listed above, children with cholera may experience drowsiness, fever, convolutions, and even a coma.
Morbidity and Mortality
In 2011, there were 589,854 reported cases of cholera around the world with 7,816 reported deaths. The case fatality rate (CFR) in 2011 was 1.33% [25]. Forty-two of those cases were reported in the United States with no fatalities while 361,162 cases were reported on Hispaniola Island with 3,205 deaths. The outbreak in Haiti accounted for 61% of the total infections that year, and the deaths accounted for 41% of the total deaths caused by cholera in 2011. These numbers help show the link between cholera infection and its relationship to the access of clean drinking water.
Diagnosis
As the excrement of infection with V. cholerae is so distinct, diagnosis can be made upon obtaining and culturing a stool sample. Typical clinical manifestations, such as the "rice water" stool and vomiting, as well as recent consumption of a contaminated water or food source, can lead to investigation into cholera by the physician. A rectal swab or fecal sample when cultured will correctly indicate the source of the infection [14]. Cholera diarrhea is often self-limiting, as the species is not native to the normal human microbiota and will be expelled after several days [9].

Treatment
Cholera is not detrimental if treatment is administered promptly. Replacing lost fluids and electrolytes by oral or intravenous hydration is of utmost importance in addition to oral rehydration salts (ORS). The use of zinc supplements is also beneficial to reduce the frequency of diarrhea in children [9] [21]. Antibiotics are only prescribed to patients with severe dehydration. The first choice of antibiotic is doxycycline; tetracycline and azithromycin are also preferred. Erythromycin is approved for use in pregnant women and children. Antibiotics work to reduce the frequency of diarrhea, which also reduces the number of V. cholerae that leave the body via defecation; thus, the transmission of the disease is also reduced [18].
Prevention
Transmission of cholera does not occur upon contact with an infected individual, but from contact or ingestion of fecal contaminated food and water containing V. cholerae. It remains a major public health issue in third world countries with underdeveloped sanitation systems. Multidisciplinary approaches are used to prevent the spread of disease. Preventative measures include: Practicing proper hygiene, home water sanitation methods, safe food preparation techniques, and the implementation of a community based strategy approach [9] [19] [20].
Water sanitation: Water should be boiled for a minimum minute before use and treated with chlorine, iodine, or household bleach as recommended by the WHO. Add 8 drops of bleach for every gallon of water and wait 30 minutes before use.
Proper hygiene: One should wash their hands before food preparation, after caring for an ill person, and after using the lavatory. If soap is not available, scrub hands with sand or ash and rinse off with safe water. If toilets are not available, defecate in a plastic bag and bury feces at least 30 meters away from any body of water.
Food preparation: Eat only fruits and vegetables that are covered with a skin that can be peeled by hand, as well as cooking food thoroughly, especially seafood.
Oral vaccination: Vaccination is available in many countries except in the United States. The leading vaccines for cholera are Dukoral and ShanChol, WHO prequalified and licensed vaccines that are distributed around the world. Use of the cholera vaccine is not intended to completely dislodge the disease or for travelers because it offers protection for a short period of time. Thus, preventative measures should be practiced.
The cloth filtration or the Sari Filtration technique:

V. cholerae attaches to zooplankton and copepods in water; thus by reducing the number of carriers in water directly reduces the number of pathogenic bacteria that get transmitted upon filtration. It is a simple, low cost, low maintenance technique that requires minimal effort to filter large quantities of water. The method involves using an old sari or cotton cloth that is folded four times, then wrapped tightly around the mouth of a water vessel. While water is drained from the vessel into another clean vessel, the zooplankton and copepods attach to the sari cloth, allowing only filtered water to pass through. Sufficient maintenance techniques include: Washing the cloth and sun drying it for a few hours; the use of a disinfectant is advised during the monsoon season [22].
Immune Response
Host Response
The human mucosal immune system is thought to act against cholera infection by the development of immunological memory to the pathogen. In studies of vaccination of humans with a strain of V. cholerae, localized and peripheral immune responses differed from initial infection, suggesting memory of the adaptive immune response induces a response to reinfection. Vaccination proved to invoke antibody responses in the intestine, as well as stimulate mucosal immunological memory. IgA antibodies were found in the highest proportion locally, suggesting IgA as the dominant isotype in intestinal tissue. In addition, in the research subjects who were not vaccinated yet were exposed a second time to V. cholerae, IFN-y secretion dramatically increased. The same was found in all but one individual in the vaccination group after a second round of vaccination, thus determining the vaccine stimulated a similar response [13].
Typically, antibody responses to infection may require large amounts of the bacteria, and the response can be short-lived. With cholera, however, the toxin is so potent that it seems to stimulate a stronger antibody response. Thus, protection from disease return in cholera can last for several years, compared to the few months associated with other infections with coproantibody stimulation [13]. Immunity to cholera has both antitoxin and antibacterial components. Both aspects of the host response appear to be necessary for immunity. One study shows that vibriocidal antibody titer presence alone is not an indication of protection against reinfection with the disease. Additionally, several pathogenic strains exist, and antibody protection against one strain does not confer protection against an alternate strain [14].
Bacterial Evasion
As aforementioned, the human immune system relies heavily on IgA antibodies to suppress infection by V. cholerae [13]. In order to combat this response, V. cholerae appears to disguise itself from IgA receptors. By failing to secrete surface adhesion, a type IV mannose-sensitive hemagglutinin (MSHA) pilus, the pathogen is able to be unrecognized and thus can evade the host immune response. ToxT controls the down-regulation of MSHA in order to use gene repression as a mode of evasion [15].
References
1 "Stopping cholera with a sari". Down to Earth - Science and Environment Online. 2013, July 12.
2 " Kogan, Nicole. "Exploring World Involvement in Haiti". United Against Infectious Diseases. 2013, July 12.
3 "The Broad Street pump." Secret Cities. 2013, July 15.
4 News-Medical "Cholera Transmission". 2013.
5 Dominican Today. 2013, July 15.
6 Despommier D, Chen S. "Cholera". Medical Ecology. 2004.
7 Centers for Disease Control and Prevention (CDC). Cholera - Vibrio cholerae infection. General Information. "Where is Cholera Found". 2013, July 9.
8 Spagnuolo AM, DiRita V, Kirschner D. "A model for Vibrio cholerae colonization of the human intestine.". J Theor Biol. 2011, November 21; 289; pp. 247-258.
9 World Health Organization (WHO). Cholera - Fact sheet. 2012, July.
10 Snow, John. On the Mode of Communication of Cholera. Wilson and Ogilvy, London, 1849. Accessed for free on UCLA Department of Epidemiology website.
11 Summers, Judith. Soho - A History of London's Most Colourful Neighborhood, Bloomsbury, London, 1989, pp. 113-117. Accessed for free on UCLA Department of Epidemiology website.
12 Centers for Disease Control and Prevention (CDC). Cholera - Vibrio cholerae infection. "Diagnosis and detection". 2013, July 12.
13 Quidling, Marianne, et al. The Journal of Clinical Investigation (JCI). "Intestinal immune responses in humans. Oral cholera vaccination induces strong intestinal antibody responses and interferon-gamma production and evokes local immunological memory." 1991, July. 88(1). pp. 143-148.
14 Saha, Debasish, et al. Journal of Infectious Diseases. 2003, May. 189(12). pp. 2318-2322.
15 Hsiao, Ansel, et al. Proceedings of the National Academy of Sciences of the United States of America (PNAS). "Vibrio cholerae virulence regulator-coordinated evasion of host immunity". 2006, September 26. 103(39). pp. 14542-14547.
16 Bose N, Payne SM, Taylor RK. "Type 4 Pilus Biogenesis and Type II-Mediated Protein Secretion by Vibrio cholerae Occur Independently of the TonB-Facilitated Proton Motive Force" Journal of Bacteriology. 2002. vol 184.
17 Todar K, PhD. "Vibrio cholerae and Asiatic Cholera" Todar's Online Textbook of Bacteriology. 2008.
18 Centers for Disease Control and Prevention. Cholera- “Treatment.” 2013, July 9.
19 Centers for Disease Control and Prevention. Cholera- “Prevention & Control.” 2013, July 9.
20 Mayo Clinic. “Prevention.” 2012, July 12.
21 Bajait, Chaitali and Vijay Thawani. NCBI- “Role of zinc in pediatric diarrhea.” 2011, May.
22 Anwar Huq, Mohammed Yunus, Syed Salahuddin Sohel, Abbas Bhuiya, Michael Emch, Stephen P. Luby, Estelle Russek-Cohen, G. Balakrish Nair, R. Bradley Sack, and Rita R. Colwell. ASM- “Simple Sari Cloth Filitration of Water Is Sustainable and Continues To Protect Villagers from Cholera in Matlab, Bangladesh.” 2010, May 18.
23 Centers for Disease Control and Prevention (CDC). Cholera - Vibrio cholerae infection. "Illness and Symptoms". 2013, July 9.
24 Mayo Clinic. “Cholera: symptoms.” 2012, July 12.
25 World Health Organization. Weekly epidemiological record. "Cholera, 2011." 2012, August 3.
Created by Bhumi Patel, Dehra McGuire, and Gracen Conway, students of Tyrrell Conway at the University of Oklahoma.
