Y. enterocolitica: Difference between revisions
No edit summary |
|||
| (36 intermediate revisions by 8 users not shown) | |||
| Line 1: | Line 1: | ||
{{Conway}} | |||
{{ | [[File:Y. enterocolitica.jpg|1000px|thumb|right| <i>Yersinia enterocolitica</i>. From:http://www.nbbcfood.info/foodmatters/foodsafetyatoz/images/30fsmyersinia.jpg]] | ||
[[File:Y. enterocolitica.jpg|1000px|thumb|right| | |||
==Etiology/Bacteriology== | ==Etiology/Bacteriology== | ||
===Taxonomy=== | ===Taxonomy=== | ||
| Domain = [[Bacteria]] | | Domain = [[Bacteria]] | ||
| Phylum = [[Proteobacteria]] | | Phylum = [[Proteobacteria]] | ||
| Class = | | Class = Gammaproteobacteria | ||
| Order = [[Enterobacteriales]] | | Order = [[Enterobacteriales]] | ||
| Family = | | Family = Enterobacteriaceae | ||
| Genus = [[Yersinia]] | | Genus = [[Yersinia]] | ||
| species = <i>Y. enterocolitica</i> | | species = <i>Y. enterocolitica</i> | ||
| Line 19: | Line 16: | ||
===Description=== | ===Description=== | ||
<i>Yersinia enterocolitica </i> is a Gram negative coccobacillus-shaped, facultative anaerobe that is motile at temperatures ranging from 22 to 30°C. This bacterium is not part of the human microbiota, but has been isolated from clinical specimens along with many other animals including pigs, cattle, birds, and domestic animals [[#References|[ | <i>Yersinia enterocolitica </i> is a Gram negative coccobacillus-shaped, facultative anaerobe that is motile at temperatures ranging from 22 to 30°C. This bacterium is not part of the human microbiota, but has been isolated from clinical specimens along with many other animals including pigs, cattle, birds, and domestic animals [[#References|[1]]]. <i>Y. enterocolitica </i> is psychrotrophic, meaning it can flourish in lower temperatures, even below 4°C. Therefore, it can survive freezing and inhabit frozen foods for a long period of time [[#References|[2]]]. There are several different serotypes of <i>Yersinia enterocolitica </i> classified by the surface antigens they share, which are then further categorized according to which O-antigen they express on their surface. Only certain types of this bacterium are human pathogens. Infections from <i>Yersinia enterocolitica </i> are common year-round, but have an optimum infection period in fall and winter. Certain types of infections occur in different geographical areas. For example, serotypes O:3 and O:9 are responsible for outbreaks in Europe, while O:8 is found in the United States, and O:5 and O:27 are found in Canada and Japan [[#References|[3]]]. <i>Yersinia enterocolitica </i> is a common cause of food-borne gastrointestinal diseases in moderate and subtropical climates around the world. An infection may present itself as enteritis, terminal ileitis, pseudo appendicitis, or mesenteric lyphadenitis, which is inflammation of the mesenteric lymph nodes [[#References|[4]]]. As a zoonotic pathogen,<i>Y. enterocolitica </i> can infect the host after ingestion of contaminated food or water. Although host gastric acid act as a substantial barrier to prevent infection from the pathogen, <i>Y. enterocolitica </i> utilizes plasmids during pathogenesis to overcome this barrier. These plasmids include an outer membrane protein, YadA, that is used for adhesion and can resist phagocytosis by host cell with the help of Yops proteins [[#References|[2]]]. Yersiniosis, a disease caused by this microorganism, has symptoms including abdominal pain, fever and diarrhea that occurs in 80% of cases. Patients usually recover within three weeks of infection without the use of antimicrobials, unless it becomes chronic entercolitis. This disease may last a few months; however, fatalities from <i> Yersinia entercolitica </i> are extremely rare. Infections caused by this pathogen can be easily prevented using proper sterilization techniques when handling food, practicing proper hygiene, and avoiding raw milk or undercooked pork products [[#References|[2]]]. | ||
==Pathogenesis== | ==Pathogenesis== | ||
===Transmission=== | ===Transmission=== | ||
<i>Yersinia enterocolitica </i>is found in meats (pork, beef, lamb, ect.), fish, and raw milk. Exact reason for food contamination is unknown [[#References|[ | <i>Yersinia enterocolitica </i>is found in meats (pork, beef, lamb, ect.), fish, and raw milk. Exact reason for food contamination is unknown [[#References|[5]]]. Human-to-human transmission is rare, however, incidences have been observed and reported. It is thought that an infected person suffering from diarrheal symptoms will transmit the disease to others if proper hand washing techniques are not followed [[#References|[6]]]. <i>Yersinia enterocolitica </i> infection results in yersiniosis—a zoonotic disease that occurs in humans, cattle, birds and pigs [[#References|[5]]]. Only a few strains cause infection in humans, and children are infected more often than adults. However, there are extreme cases in which <i>Y. enterocolitica</i> has been transmitted via blood transfusions. In such cases, transfusion acquired septicemia usually results from the infected blood serum [[#References|[6]]]. There are over 60 serotypes for <i>Yersinia enterocolitica </i>. The serotypes pathogenic to humans are O:3, O:5,27, O:8, O:9, and O:13 [[#References|[5,7]]]. [[File:Y. modeoftransmission.jpeg|1000px|thumb|right|Mode of Transmission of <i>Yersinia enterocolitica</i>. From:http://www.hindawi.com/journals/jpath/2011/429069.fig.001.jpg]] | ||
''Y. enterocolitica'' has various serotypes for different mammals and each strain has different virulence factors. Biotypes 2 to 5 are less virulent in mice yet account for a majority of human illnesses [11]. Bioserotype 4/O:3 accounts for around 90% of illnesses in the Eastern hemisphere, and is one of the two main strains found in pigs. As stated earlier, the bacteria are mainly foodborne pathogens, and transmitted through undercooked pork. Studies show that each biotype possesses similar mechanisms but different virulence in humans. | |||
===Infectious dose, incubation, and colonization=== | ===Infectious dose, incubation, and colonization=== | ||
According to the CDC, the infectious dose of <i>Yersinia enterocolitica </i> is currently unknown, however, the FDA estimates it is between 10<sup>4</sup> to 10<sup>6</sup> organisms. The infectious | According to the CDC, the infectious dose of <i>Yersinia enterocolitica </i> is currently unknown, however, the FDA estimates it is between 10<sup>4</sup> to 10<sup>6</sup> organisms. The infectious dose depend on the strain and host factors. It takes a lower dose of organisms to cause yersiniosis in young children and the elderly, who have weakened immune systems, compared to a healthy adult's immune system [[#References|[2]]]. Illness takes place between 24 and 48 hours after ingestion [[#References|[8]]]. Illness typically presents as diarrhea—sometimes bloody—low-grade fever, abdominal pain and vomiting, which is present in 15%-40% of cases [[#References|[7]]]. Yersiniosis is less common due to the improvement of food processing techniques, which eliminate the risk of infection [[#References|[8]]]. <i> Y. enterocolitica </i> efficiently colonizes the small intestine. After entering the host, bacteria adhere to the lumen and invade the epithelial lining, eventually going to the Peyer Patches where the microorganism proliferates [[#References|[7]]]. <i> Y. enterocolitica </i> colonization requires the transfer of the bacteria across the epithelial tissue barrier. | ||
''Yersinia enterocolitica'' attaches to epithelial cells by use of three proteins: per se, Inv promotes entry, YadA (plasma encoded protein) promotes adhesion for attachment, and Ail correlates with virulence because its only detected among pathogenic strains [12]. | |||
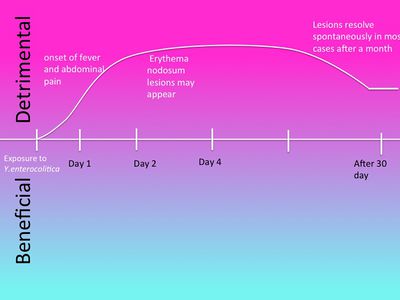
[[Image:DamageResponseFrameworkYentericolitica.jpg|thumb|400px|right|''Damage Response Framework of Yersiniosis caused by Yersinia enterocolitica[https://microbewiki.kenyon.edu/index.php/File:DamageResponseFrameworkYentericolitica.jpg]]] | |||
===Virulence Factors=== | ===Virulence Factors=== | ||
There are 3 invasive proteins—Ail, YadA and invasin that are produced by <i>Yersinia entercolitica </i>[[#References|[ | There are 3 invasive proteins—Ail, YadA and invasin that are produced by <i>Yersinia entercolitica </i>[[#References|[7]]]. These proteins promote adherence and invasion of microfold cells, which are found in the follicle-associated epithelium of Peyer's patches. Microfold cells, or M cells, are a type of antigen-sampling intestinal epithelial cells. | ||
====Enterotoxicity==== | ====Enterotoxicity==== | ||
The toxin Yst | The toxin Yst, included on the genes ystA and ystB, is a membrane-acting virulence factor. It is a heat-stable enterotoxin that is important in causing diarrhea in the host, however, it is only present in virulent strains of <i> Y. enterocolitica </i>. It stimulates the cGMP synthesis in the intestinal lining, which leads to an overall effect of fluid loss due to a lack of fluid absorption [[#References|[9]]]. The enterotoxin produced by <i> Y. enterocolitica </i> is similar to that of <i> Escherichia coli </i>. Nevertheless, the enterotoxin only plays a minor role in pathogenesis, because diarrheal symptoms have been observed in the absence of the enterotoxin [[#References|[7]]] . The outer membrane antigens are associated with bacterial resistance to opsonization and phagocytosis by neutrophils [[#References|[7]]]. | ||
====Iron and Pathogenicity==== | |||
<i> Y. enterocolitica </i> is unable to chelate iron. Despite not being able to produce siderophores-- <i> Y. enterocolitica </i> can utilize siderophores produced by other bacteria [[#References|[ | <i> Y. enterocolitica </i> is unable to chelate iron. Despite not being able to produce siderophores-- <i> Y. enterocolitica </i> can utilize siderophores produced by other bacteria [[#References|[7]]]. This pathogen contains the plasmid PYV encoding virulence genes that affect pathogenesis. Included in these virulence genes it YadA (Yersinia adhesion A), which is an outer-membrane protein that is expressed by the organism. Also included is the type III secretory system guided by Yops proteins that offer <i> Y. enterocolitica </i> a way to resist phagocytosis and immune responses by the host [[#References|[2]]]. | ||
==Epidemiology== | ==Epidemiology== | ||
The most susceptible | The populations most susceptible to <i> Y. enterocolitica </i> are small children, the elderly, and immuno-suppressed hosts [[#References|[8]]] . 75% of patients with this disease are between the age of 5-15 years [[#References|[7]]]. Most isolates of the disease are type O:3 and O:9 serotypes found in Canada and Europe. In the US it is estimated that approximately 5% of enteric bacterial infections are in children under the age of 5.The CDC reports 17,000 cases of infection in the United States annually [[#References|[5]]]. This disease is much more common in Northern Europe, Scandinavia, and Japan. | ||
==Clinical Features== | ==Clinical Features== | ||
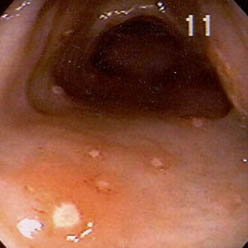
<i> Yersinia enterocolitica </i> | <i> Yersinia enterocolitica </i> typically causes diarrhea in all manifestations of the infection, with occasional more severe cases containing blood in the stools [[#References|[7]]]. The disease may present differently when comparing adult and adolescent cases. Pediatric cases are characterized by fever, abdominal pain, and more commonly present with bloody diarrhea than in adults [[#References|[8]]]. The most common presentation of <i> Y. enterocolitica </i> in children is enterocolitis. The symptoms include watery and mucoid diarrhea, fever, colicky abdominal pain, and stools containing a high number of white blood cells. Adults characterize their infection symptoms as being diarrhea, localized lower right quadrant abdominal pain, vomiting, and low-grade fever [[#References|[7]]]. Often the infection will clear without the aid of antibiotics, but those that do not display more severe side effects which includes red or purple raised lesions, known as erythema nodosum and joint pain commonly in the knees, wrists, or ankles [[#References|[5]]]. Erythema nodosum lesions appear 2-20 days after the onset of the infection and usually resolve without medical treatment in about a month [[#References|[7]]]. Lesions are more commonly seen in females and present on the patient’s trunk and legs. Joint pain may manifest about a month after the onset of symptoms and cease after 1 to 6 months [[#References|[5]]]. Septicemia, or bacteria in the blood, can occur in adults with predisposing conditions, such as diabetes mellitus, immune defect, alcoholism, thalassemia, sickle cell disease, or hemochromatosis. Septicemia can also cause metastatic infections including abscesses in the liver, spleen, kidneys, and lungs [[#References|[7]]]. [[File:yersinitis.jpg|1000px|thumb|right|<i>Yersinia enterocolitica</i>in a 45 year old woman. From:http://img.medscape.com/pi/emed/ckb/infectious_diseases/211212-232343-1185.jpg]] | ||
==Diagnosis== | ==Diagnosis== | ||
There are numerous tests that can be | There are numerous tests that can be conducted to diagnose a <i> Yersinia enterocolitica </i> infection. A stool culture is the best way to confirm the presence of the pathogen, but can take two weeks after the onset of the disease for the culture result to come back positive or negative [[#References|[7]]]. Other tests include tube agglutination, enzyme-linked immunosorbent assays, radioimmunoassays, ultrasonography or computed tomography scanning imaging studies, colonoscopy, and joint aspiration in certain cases [[#References|[7]]]. A majority of <i> Y. enterocolitica </i> infections will clear up on their own with good nutrition and hydration [[#References|[7]]]. Severe or complicated infections can be treated with the appropriate antibiotics. [[#References|[5]]]. | ||
==Treatment== | ==Treatment== | ||
Infections by <i> Yersinia enterocolitica </i> are usually self-limiting and will resolve on their own in most patients who recover without any antibiotic treatment within a seven days to three weeks [[#References|[ | Infections by <i> Yersinia enterocolitica </i> are usually self-limiting and will resolve on their own in most patients who recover without any antibiotic treatment within a seven days to three weeks period [[#References|[5]]]. Hydration is important in uncomplicated cases of diarrhea caused by the organism and will be sufficient treatment in the infection, however in severe or more complicated cases of infection antibiotic treatment may be necessary. The antibiotics commonly used are aminoglycosides, doxycycline, trimethoprim-sulfamethoxazole, or fluoroquinolones [[#References|[5]]]. | ||
==Prevention== | ==Prevention== | ||
Prevention of <i>Yersinia enterocolitica</i> infection is | Prevention of <i>Yersinia enterocolitica</i> infection is a matter of avoidance of certain foods. The most common mode of transmission is via poultry and livestock [[#References|[7]]]. Thus, avoid raw or undercooked meats. Milk products must be pasteurized before consumption. If raw meat is handled, clean hands thoroughly to avoid cross-contamination. Beware of cross-contamination in the kitchen by cleaning all surfaces and appliances with soap and hot water. Animal feces may also be contaminated, so dispose of all animal waste properly [[#References|[7]]]. | ||
==Host Immune Response== | ==Host Immune Response== | ||
During the later stages of <i>Yersinia</i> infection, there are many clinical and histological signs of host response. The host immune response activates macrophages against the infection. Macrophage activation is dependent upon the number of | During the later stages of <i>Yersinia</i> infection, there are many clinical and histological signs of host response. The host's innate immune response activates macrophages against the infection. Macrophage activation is dependent upon the number of CFUs in the host and the duration of the infection. The immune response will produce multiple TLR ligands, which activate the macrophages [[#References|[10]]]. The release of the aforementioned ligands by macrophages will contribute to inflammation of the small intestine. Induction of inflammation is a typical host immune response to enteric pathogens. | ||
==References== | ==References== | ||
1. Microbiology in Pictures. http://www.microbiologyinpictures.com/yersinia%20enterocolitica.html | |||
2. Handbook of Foodborne Pathogenic Microorganisms. http://www.fda.gov/downloads/Food/FoodSafety/FoodborneIllness/FoodborneIllnessFoodbornePathogensNaturalToxins/BadBugBook/UCM297627.pdf | |||
3. Public Heath Agency of Canada. http://www.phac-aspc.gc.ca/lab-bio/res/psds-ftss/yersinia-enterocolitica-eng.php#footnote7 | |||
4. Infection and Immunity. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1951990/#!po=1.72414 | |||
5. CDC. http://www.cdc.gov/ncidod/dbmd/diseaseinfo/yersinia_g.htm | |||
6. Hindawi. http://www.hindawi.com/journals/jpath/2011/429069/ | |||
7. Medscape. http://emedicine.medscape.com/article/232343-overview | |||
8. FDA. http://www.fda.gov/Food/FoodborneIllnessContaminants/CausesOfIllnessBadBugBook/ucm070040.htm | |||
9. Virulence Factors of Pathogenic Bacteria. http://www.mgc.ac.cn/cgi-bin/VFs/vfs.cgi?Genus=Yersinia&Keyword=Toxin | |||
10. Journal of Immunology. http://www.jimmunol.org/content/168/3/1315.full.pdf | 10. Journal of Immunology. http://www.jimmunol.org/content/168/3/1315.full.pdf | ||
11. Infection and Immunity. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3811832/ | |||
12. Yersinia enterocolitica: Pathogenesis, virulence and antimicrobial resistance. http://www.elsevier.es/es-revista-enfermedades-infecciosas-microbiologia-clinica-28-articulo-iyersinia-enterocolitica-i-pathogenesis-virulence-and-90093119 | |||
Created by Emily Kurtz, Kristen Hoelscher, Dane Korber and Caitlyn Baukal, students of Tyrrell Conway at the University of Oklahoma | Created by Emily Kurtz, Kristen Hoelscher, Dane Korber and Caitlyn Baukal, students of Tyrrell Conway at the University of Oklahoma | ||
Edited by Jordan Abney and Sofia Buscarini | |||
Latest revision as of 19:12, 11 February 2016

Etiology/Bacteriology
Taxonomy
| Domain = Bacteria | Phylum = Proteobacteria | Class = Gammaproteobacteria | Order = Enterobacteriales | Family = Enterobacteriaceae | Genus = Yersinia | species = Y. enterocolitica
Description
Yersinia enterocolitica is a Gram negative coccobacillus-shaped, facultative anaerobe that is motile at temperatures ranging from 22 to 30°C. This bacterium is not part of the human microbiota, but has been isolated from clinical specimens along with many other animals including pigs, cattle, birds, and domestic animals [1]. Y. enterocolitica is psychrotrophic, meaning it can flourish in lower temperatures, even below 4°C. Therefore, it can survive freezing and inhabit frozen foods for a long period of time [2]. There are several different serotypes of Yersinia enterocolitica classified by the surface antigens they share, which are then further categorized according to which O-antigen they express on their surface. Only certain types of this bacterium are human pathogens. Infections from Yersinia enterocolitica are common year-round, but have an optimum infection period in fall and winter. Certain types of infections occur in different geographical areas. For example, serotypes O:3 and O:9 are responsible for outbreaks in Europe, while O:8 is found in the United States, and O:5 and O:27 are found in Canada and Japan [3]. Yersinia enterocolitica is a common cause of food-borne gastrointestinal diseases in moderate and subtropical climates around the world. An infection may present itself as enteritis, terminal ileitis, pseudo appendicitis, or mesenteric lyphadenitis, which is inflammation of the mesenteric lymph nodes [4]. As a zoonotic pathogen,Y. enterocolitica can infect the host after ingestion of contaminated food or water. Although host gastric acid act as a substantial barrier to prevent infection from the pathogen, Y. enterocolitica utilizes plasmids during pathogenesis to overcome this barrier. These plasmids include an outer membrane protein, YadA, that is used for adhesion and can resist phagocytosis by host cell with the help of Yops proteins [2]. Yersiniosis, a disease caused by this microorganism, has symptoms including abdominal pain, fever and diarrhea that occurs in 80% of cases. Patients usually recover within three weeks of infection without the use of antimicrobials, unless it becomes chronic entercolitis. This disease may last a few months; however, fatalities from Yersinia entercolitica are extremely rare. Infections caused by this pathogen can be easily prevented using proper sterilization techniques when handling food, practicing proper hygiene, and avoiding raw milk or undercooked pork products [2].
Pathogenesis
Transmission
Yersinia enterocolitica is found in meats (pork, beef, lamb, ect.), fish, and raw milk. Exact reason for food contamination is unknown [5]. Human-to-human transmission is rare, however, incidences have been observed and reported. It is thought that an infected person suffering from diarrheal symptoms will transmit the disease to others if proper hand washing techniques are not followed [6]. Yersinia enterocolitica infection results in yersiniosis—a zoonotic disease that occurs in humans, cattle, birds and pigs [5]. Only a few strains cause infection in humans, and children are infected more often than adults. However, there are extreme cases in which Y. enterocolitica has been transmitted via blood transfusions. In such cases, transfusion acquired septicemia usually results from the infected blood serum [6]. There are over 60 serotypes for Yersinia enterocolitica . The serotypes pathogenic to humans are O:3, O:5,27, O:8, O:9, and O:13 [5,7].
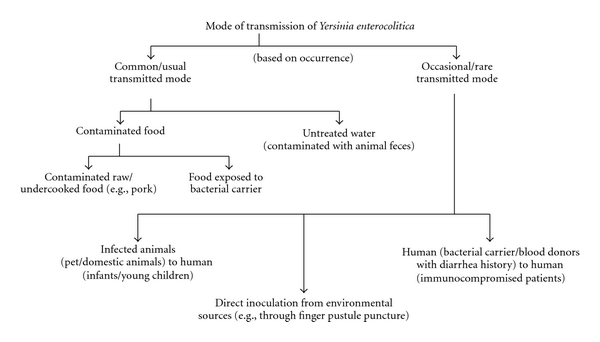
Y. enterocolitica has various serotypes for different mammals and each strain has different virulence factors. Biotypes 2 to 5 are less virulent in mice yet account for a majority of human illnesses [11]. Bioserotype 4/O:3 accounts for around 90% of illnesses in the Eastern hemisphere, and is one of the two main strains found in pigs. As stated earlier, the bacteria are mainly foodborne pathogens, and transmitted through undercooked pork. Studies show that each biotype possesses similar mechanisms but different virulence in humans.
Infectious dose, incubation, and colonization
According to the CDC, the infectious dose of Yersinia enterocolitica is currently unknown, however, the FDA estimates it is between 104 to 106 organisms. The infectious dose depend on the strain and host factors. It takes a lower dose of organisms to cause yersiniosis in young children and the elderly, who have weakened immune systems, compared to a healthy adult's immune system [2]. Illness takes place between 24 and 48 hours after ingestion [8]. Illness typically presents as diarrhea—sometimes bloody—low-grade fever, abdominal pain and vomiting, which is present in 15%-40% of cases [7]. Yersiniosis is less common due to the improvement of food processing techniques, which eliminate the risk of infection [8]. Y. enterocolitica efficiently colonizes the small intestine. After entering the host, bacteria adhere to the lumen and invade the epithelial lining, eventually going to the Peyer Patches where the microorganism proliferates [7]. Y. enterocolitica colonization requires the transfer of the bacteria across the epithelial tissue barrier.
Yersinia enterocolitica attaches to epithelial cells by use of three proteins: per se, Inv promotes entry, YadA (plasma encoded protein) promotes adhesion for attachment, and Ail correlates with virulence because its only detected among pathogenic strains [12].
Virulence Factors
There are 3 invasive proteins—Ail, YadA and invasin that are produced by Yersinia entercolitica [7]. These proteins promote adherence and invasion of microfold cells, which are found in the follicle-associated epithelium of Peyer's patches. Microfold cells, or M cells, are a type of antigen-sampling intestinal epithelial cells.
Enterotoxicity
The toxin Yst, included on the genes ystA and ystB, is a membrane-acting virulence factor. It is a heat-stable enterotoxin that is important in causing diarrhea in the host, however, it is only present in virulent strains of Y. enterocolitica . It stimulates the cGMP synthesis in the intestinal lining, which leads to an overall effect of fluid loss due to a lack of fluid absorption [9]. The enterotoxin produced by Y. enterocolitica is similar to that of Escherichia coli . Nevertheless, the enterotoxin only plays a minor role in pathogenesis, because diarrheal symptoms have been observed in the absence of the enterotoxin [7] . The outer membrane antigens are associated with bacterial resistance to opsonization and phagocytosis by neutrophils [7].
Iron and Pathogenicity
Y. enterocolitica is unable to chelate iron. Despite not being able to produce siderophores-- Y. enterocolitica can utilize siderophores produced by other bacteria [7]. This pathogen contains the plasmid PYV encoding virulence genes that affect pathogenesis. Included in these virulence genes it YadA (Yersinia adhesion A), which is an outer-membrane protein that is expressed by the organism. Also included is the type III secretory system guided by Yops proteins that offer Y. enterocolitica a way to resist phagocytosis and immune responses by the host [2].
Epidemiology
The populations most susceptible to Y. enterocolitica are small children, the elderly, and immuno-suppressed hosts [8] . 75% of patients with this disease are between the age of 5-15 years [7]. Most isolates of the disease are type O:3 and O:9 serotypes found in Canada and Europe. In the US it is estimated that approximately 5% of enteric bacterial infections are in children under the age of 5.The CDC reports 17,000 cases of infection in the United States annually [5]. This disease is much more common in Northern Europe, Scandinavia, and Japan.
Clinical Features
Yersinia enterocolitica typically causes diarrhea in all manifestations of the infection, with occasional more severe cases containing blood in the stools [7]. The disease may present differently when comparing adult and adolescent cases. Pediatric cases are characterized by fever, abdominal pain, and more commonly present with bloody diarrhea than in adults [8]. The most common presentation of Y. enterocolitica in children is enterocolitis. The symptoms include watery and mucoid diarrhea, fever, colicky abdominal pain, and stools containing a high number of white blood cells. Adults characterize their infection symptoms as being diarrhea, localized lower right quadrant abdominal pain, vomiting, and low-grade fever [7]. Often the infection will clear without the aid of antibiotics, but those that do not display more severe side effects which includes red or purple raised lesions, known as erythema nodosum and joint pain commonly in the knees, wrists, or ankles [5]. Erythema nodosum lesions appear 2-20 days after the onset of the infection and usually resolve without medical treatment in about a month [7]. Lesions are more commonly seen in females and present on the patient’s trunk and legs. Joint pain may manifest about a month after the onset of symptoms and cease after 1 to 6 months [5]. Septicemia, or bacteria in the blood, can occur in adults with predisposing conditions, such as diabetes mellitus, immune defect, alcoholism, thalassemia, sickle cell disease, or hemochromatosis. Septicemia can also cause metastatic infections including abscesses in the liver, spleen, kidneys, and lungs [7].
Diagnosis
There are numerous tests that can be conducted to diagnose a Yersinia enterocolitica infection. A stool culture is the best way to confirm the presence of the pathogen, but can take two weeks after the onset of the disease for the culture result to come back positive or negative [7]. Other tests include tube agglutination, enzyme-linked immunosorbent assays, radioimmunoassays, ultrasonography or computed tomography scanning imaging studies, colonoscopy, and joint aspiration in certain cases [7]. A majority of Y. enterocolitica infections will clear up on their own with good nutrition and hydration [7]. Severe or complicated infections can be treated with the appropriate antibiotics. [5].
Treatment
Infections by Yersinia enterocolitica are usually self-limiting and will resolve on their own in most patients who recover without any antibiotic treatment within a seven days to three weeks period [5]. Hydration is important in uncomplicated cases of diarrhea caused by the organism and will be sufficient treatment in the infection, however in severe or more complicated cases of infection antibiotic treatment may be necessary. The antibiotics commonly used are aminoglycosides, doxycycline, trimethoprim-sulfamethoxazole, or fluoroquinolones [5].
Prevention
Prevention of Yersinia enterocolitica infection is a matter of avoidance of certain foods. The most common mode of transmission is via poultry and livestock [7]. Thus, avoid raw or undercooked meats. Milk products must be pasteurized before consumption. If raw meat is handled, clean hands thoroughly to avoid cross-contamination. Beware of cross-contamination in the kitchen by cleaning all surfaces and appliances with soap and hot water. Animal feces may also be contaminated, so dispose of all animal waste properly [7].
Host Immune Response
During the later stages of Yersinia infection, there are many clinical and histological signs of host response. The host's innate immune response activates macrophages against the infection. Macrophage activation is dependent upon the number of CFUs in the host and the duration of the infection. The immune response will produce multiple TLR ligands, which activate the macrophages [10]. The release of the aforementioned ligands by macrophages will contribute to inflammation of the small intestine. Induction of inflammation is a typical host immune response to enteric pathogens.
References
1. Microbiology in Pictures. http://www.microbiologyinpictures.com/yersinia%20enterocolitica.html
2. Handbook of Foodborne Pathogenic Microorganisms. http://www.fda.gov/downloads/Food/FoodSafety/FoodborneIllness/FoodborneIllnessFoodbornePathogensNaturalToxins/BadBugBook/UCM297627.pdf
3. Public Heath Agency of Canada. http://www.phac-aspc.gc.ca/lab-bio/res/psds-ftss/yersinia-enterocolitica-eng.php#footnote7
4. Infection and Immunity. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1951990/#!po=1.72414
5. CDC. http://www.cdc.gov/ncidod/dbmd/diseaseinfo/yersinia_g.htm
6. Hindawi. http://www.hindawi.com/journals/jpath/2011/429069/
7. Medscape. http://emedicine.medscape.com/article/232343-overview
8. FDA. http://www.fda.gov/Food/FoodborneIllnessContaminants/CausesOfIllnessBadBugBook/ucm070040.htm
9. Virulence Factors of Pathogenic Bacteria. http://www.mgc.ac.cn/cgi-bin/VFs/vfs.cgi?Genus=Yersinia&Keyword=Toxin
10. Journal of Immunology. http://www.jimmunol.org/content/168/3/1315.full.pdf
11. Infection and Immunity. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3811832/
12. Yersinia enterocolitica: Pathogenesis, virulence and antimicrobial resistance. http://www.elsevier.es/es-revista-enfermedades-infecciosas-microbiologia-clinica-28-articulo-iyersinia-enterocolitica-i-pathogenesis-virulence-and-90093119
Created by Emily Kurtz, Kristen Hoelscher, Dane Korber and Caitlyn Baukal, students of Tyrrell Conway at the University of Oklahoma
Edited by Jordan Abney and Sofia Buscarini
