Effects of Scleroderma on Human Microbiome: Difference between revisions
No edit summary |
|||
| Line 22: | Line 22: | ||
===Taxonomy=== | ===Taxonomy=== | ||
In SSc patients, there is a shift at the phylum level of microbiome composition.<ref name="Tan"></ref> More specifically, the ratio of Firmicutes to Bacteroidetes increases -- meaning that the abundance of Bacteroidetes decreases -- a trend shown in patients with obesity. This suggests a potential mechanism in SSc patients struggling to maintain a healthy weight. This is supported by research that has indicated microbiome changes are associated with the development of digestive dysbiosis, a condition characterized by diverse possible GI symptoms, including obesity.<ref>[https://doi.org/10.2478/jim-2021-0018 Bratoiu, Ioana, Alexandra Burlui, Patricia Richter, Anca Cardoneanu, Ciprian Rezus, and Elena Rezus. 2021. “Digestive Dysbiosis in Systemic Scleroderma: A Review.” Journal of Interdisciplinary Medicine 6 (2): 53–59.]</ref> Furthermore, there have been other changes in the gut microbiome characteristic of other GI disorders such as IBD. Some of these are increases in the abundance of Actinobacteria, Fusobacteria, and Verrucomicrobia.<ref name="Tan"></ref><br><br> | |||
Genus level differences were also noticed between Scleroderma patients and healthy controls. For example, <i>Bacteroides</i> have been observed as less abundant in SSc patients. This genus of species serves to protect from mucosal inflammation and pathogenic bacteria. Moreover, decreases in<i> Bacteroides</i> have been seen in immunodeficiency disorders such as Crohn’s Disease. Additionally, butyrate-producing bacteria species that facilitate healthy gut function decrease in abundance in SSc patients. Namely, <i>Clostridium</i> and <i>Faecilibacterium</i>. Moreover, these bacteria help to protect from mucosal inflammation as well, furthering the issue of mucosal inflammation resulting from taxonomic shifts in the gut microbiome of SSc patients.<br><br> | |||
Furthermore, there have been links between changes in the metabolome of SSc patients and healthy controls.<ref>[https://doi.org/10.1111/nyas.13736 Bellocchi, Chiara, Álvaro Fernández-Ochoa, Gaia Montanelli, Barbara Vigone, Alessandro Santaniello, Christian Milani, Rosa Quirantes-Piné, et al. 2018. “Microbial and Metabolic Multi-Omic Correlations in Systemic Sclerosis Patients.” Annals of the New York Academy of Sciences 1421 (1): 97–109.]</ref> Increases in the <i>Desulfovibrio</i> genus in the gut microbiome have been associated with increased levels of the alpha-N-phenylacetyl-l-glutamine and 2,4-dinitrobenzenesulfonic acid metabolites. The effect of increased plasma levels of these metabolites is currently unclear, though it has been suggested that they might contribute to the development or progression of SSc.<br><br> | |||
==Conclusion== | ==Conclusion== | ||
Revision as of 01:58, 2 December 2021
Introduction
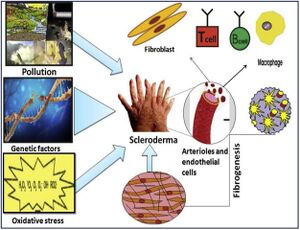
Scleroderma (or systemic sclerosis) is an autoimmune rheumatological disorder in which hardening of the skin and other organs occurs through increased amounts of collagen in the skin. [1] Additionally, there are significant impacts on the vascular system by this hardening. There are two types of scleroderma, localized and systemic. Localized is when the hardening occurs exclusively in the skin and muscular tissues. Systemic occurs when the hardening is widespread throughout many organs in the body. Additionally, there are a variety of factors suggested in the pathogenesis of scleroderma, namely, environmental, genetic, and oxidative stressors. Further, sex is known to be a major risk factor for scleroderma and autoimmune disorders in general, with autoimmune disorders occurring in those of the female sex at double the frequency. [2] A potential cause of these sex disparities is the difference in the human microbiome between the sexes. It has been noted that autoimmunity is able to be characterized by changes in the gut microbiome. Moreover, these changes occur more frequently in the female sex.[3]
Microbiome
It has been observed specifically in the GI tract that scleroderma symptoms are associated with a change in the gut microbiome, including decreases in microbial diversity [4]In studies of scleroderma patients’ gut microbiomes who displayed the SSc GI tract phenotype (scleroderma patients with GI symptoms), increased levels of Fusobacterium and Prevotella were observed.[5] This suggests that the gut microbiome contributes to the development of the SSc GI tract phenotype. Moreover, due to the established link between Prevotella in the gut and diet, it is suggested that dietary changes to lower the levels of Prevotella in the gut microbiome might reduce the effects of the SSc GI tract phenotype.
Differences in microbial diversity are typical of various forms of scleroderma.[4] Notably, when comparing the microbiomes of patients with diffuse cutaneous systemic sclerosis (DcSSc) and those with limited cutaneous systemic sclerosis (LcSSc), patients with DcSSc had lowered abundance of Lactobacillus and Coprococcus and raised abundance of Paludibacter. Furthermore, less Coproccus is seen in patients with nonalcoholic fatty liver disease, specifically in the metabolic pathway leading to liver fibrosis. This has led researchers to suggest further research into the potential role of Coproccus in the development of fibrosis phenotypes.
Changes in microbial diversity have not only been associated with scleroderma but other autoimmune disorders as well. These include inflammatory bowel disease, rheumatoid arthritis, and systemic lupus erythematosus, among others.

Genetics
Gene Expression
The presence of Alistipes, Bacteroides, and butyrate-producing bacteria are less abundant in SSc patients than healthy controls; Clostridium and Streptococcus are more abundant.[6] Perhaps more importantly, Eggerthella lenta and Clostridium boltae are also more abundant in SSc patients. E. lenta, specifically, plays a potentially critical role in upregulating Th17-activating genes in SSc patients. T helper 17 (Th17) cells are pro-inflammatory and thus potential contributors to the phenotype of organ inflammation in SSc. By upregulating Th17-activating genes, inflammation observed in SSc patients might be induced or worsened.
Taxonomy
In SSc patients, there is a shift at the phylum level of microbiome composition.[4] More specifically, the ratio of Firmicutes to Bacteroidetes increases -- meaning that the abundance of Bacteroidetes decreases -- a trend shown in patients with obesity. This suggests a potential mechanism in SSc patients struggling to maintain a healthy weight. This is supported by research that has indicated microbiome changes are associated with the development of digestive dysbiosis, a condition characterized by diverse possible GI symptoms, including obesity.[7] Furthermore, there have been other changes in the gut microbiome characteristic of other GI disorders such as IBD. Some of these are increases in the abundance of Actinobacteria, Fusobacteria, and Verrucomicrobia.[4]
Genus level differences were also noticed between Scleroderma patients and healthy controls. For example, Bacteroides have been observed as less abundant in SSc patients. This genus of species serves to protect from mucosal inflammation and pathogenic bacteria. Moreover, decreases in Bacteroides have been seen in immunodeficiency disorders such as Crohn’s Disease. Additionally, butyrate-producing bacteria species that facilitate healthy gut function decrease in abundance in SSc patients. Namely, Clostridium and Faecilibacterium. Moreover, these bacteria help to protect from mucosal inflammation as well, furthering the issue of mucosal inflammation resulting from taxonomic shifts in the gut microbiome of SSc patients.
Furthermore, there have been links between changes in the metabolome of SSc patients and healthy controls.[8] Increases in the Desulfovibrio genus in the gut microbiome have been associated with increased levels of the alpha-N-phenylacetyl-l-glutamine and 2,4-dinitrobenzenesulfonic acid metabolites. The effect of increased plasma levels of these metabolites is currently unclear, though it has been suggested that they might contribute to the development or progression of SSc.
Conclusion
Overall text length (all text sections) should be at least 1,000 words (before counting references), with at least 2 images.
Include at least 5 references under References section.
References
- ↑ Singh, Deependra, Arun KS Parihar, Satish Patel, Shikha Srivastava, Prakriti Diwan, and Manju R. Singh. 2019. “Scleroderma: An Insight into Causes, Pathogenesis and Treatment Strategies.” Pathophysiology 26 (2): 103–14.
- ↑ Angum, Fariha, Tahir Khan, Jasndeep Kaler, Lena Siddiqui, and Azhar Hussain. 2020. “The Prevalence of Autoimmune Disorders in Women: A Narrative Review.” Cureus, May.
- ↑ Gomez, Andres, David Luckey, and Veena Taneja. 2015. “The Gut Microbiome in Autoimmunity: Sex Matters.” Clinical Immunology 159 (2): 154–62.
- ↑ 4.0 4.1 4.2 4.3 Tan, Tze Chin, Maria Noviani, Ying Ying Leung, and Andrea Hsiu Ling Low. 2021. “The Microbiome and Systemic Sclerosis: A Review of Current Evidence.” Best Practice and Research: Clinical Rheumatology. Bailliere Tindall Ltd.
- ↑ Volkmann, Elizabeth R., Yu Ling Chang, Nashla Barroso, Daniel E. Furst, Philip J. Clements, Alan H. Gorn, Bennett E. Roth, et al. 2016. “Association of Systemic Sclerosis with a Unique Colonic Microbial Consortium.” Arthritis and Rheumatology 68 (6): 1483–92.
- ↑ Plichta, Damian R., Juhi Somani, Matthieu Pichaud, Zachary S. Wallace, Ana D. Fernandes, Cory A. Perugino, Harri Lähdesmäki, et al. 2021. “Congruent Microbiome Signatures in Fibrosis-Prone Autoimmune Diseases: IgG4-Related Disease and Systemic Sclerosis.” Genome Medicine 13 (1).
- ↑ Bratoiu, Ioana, Alexandra Burlui, Patricia Richter, Anca Cardoneanu, Ciprian Rezus, and Elena Rezus. 2021. “Digestive Dysbiosis in Systemic Scleroderma: A Review.” Journal of Interdisciplinary Medicine 6 (2): 53–59.
- ↑ Bellocchi, Chiara, Álvaro Fernández-Ochoa, Gaia Montanelli, Barbara Vigone, Alessandro Santaniello, Christian Milani, Rosa Quirantes-Piné, et al. 2018. “Microbial and Metabolic Multi-Omic Correlations in Systemic Sclerosis Patients.” Annals of the New York Academy of Sciences 1421 (1): 97–109.
Edited by Andrew Van Horn, student of Joan Slonczewski for BIOL 116 Information in Living Systems, 2021, Kenyon College.
