Staphylococcus aureus: Evasion of neutrophils: Difference between revisions
No edit summary |
No edit summary |
||
| Line 35: | Line 35: | ||
<b>Aggregation</b> | <b>Aggregation</b> | ||
<br> | <br> | ||
During the infection, S. aureus sometimes form fibrin-containing bacterial aggregates to elude phagocytosis. <ref name="cite ipad"></ref> To achieve agglutination with fibrinogen, S. aureus produces three important products. They are: coagulase (Coa), von Willebrand factor binding protein (vWbp), and clumping factor (Clfa). Interestingly, fibrinogen is a glycoprotein complex that is produced normally by human body to stop bleeding and it is made of three pairs of three chains of Aα-, Bβ-, and γ-chains. [ | During the infection, S. aureus sometimes form fibrin-containing bacterial aggregates to elude phagocytosis. <ref name="cite ipad"></ref> To achieve agglutination with fibrinogen, S. aureus produces three important products. They are: coagulase (Coa), von Willebrand factor binding protein (vWbp), and clumping factor (Clfa). Interestingly, fibrinogen is a glycoprotein complex that is produced normally by human body to stop bleeding and it is made of three pairs of three chains of Aα-, Bβ-, and γ-chains. <ref>[https://en.wikipedia.org/wiki/Fibrinogen#Structure Wikipedia: Fibrinogen]</ref> The compounds produced by S. aureus, coagulase and vWbp, promotes cleavage of Aα- and Bβ- chains of fibrinogen. <ref>[https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3197598/ McAdow M, Kim HK, Dedent AC, Hendrickx AP, Schneewind O, Missiakas DM. Preventing Staphylococcus aureus sepsis through the inhibition of its agglutination in blood. PLoS Pathog. 2011 Oct;7(10):e1002307.]</ref> Then, S. aureus uses Clfa to bind to fibrin clots and generate fibrin-containing bacterial aggregates. <ref name="cite ipad"></ref> | ||
<br><br> | <br><br> | ||
Revision as of 03:40, 8 December 2022
Introduction
Staphylococcus aureus (S. aureus), also known as “golden staph” and “oro staphira”, is a member of Bacillota. Staphylo meaning grape in Greek and aureus meaning golden, indicating S. aureus is a kind of yellow-colored, grapelike-cluster of bacteria. [1] [2]
S. aureus is a common type of bacteria that appears everywhere in our daily life and has a high lethal rate all around the world.
S. aureus is commonly found in the environment such as soil, water, and air, and also in the nose and on the skin of humans and animals.[3]
Its high lethality is due to its high antibiotic resistance. In the past, doctors used penicillin to treat patients with S. aureus infection but the antibiotic no longer kills the bacteria by the end of 1940s.
S. aureus is famous for its serious infection reaction in the human body. In order for bacteria to cause infection in the human body, they need to escape from the immune system. S. aureus has developed a number of strategies to survive outside of the immune system before infecting a cell. Besides, S. aureus seems to be inextirpable in that it is resistant to nearly all types of antibiotics. Whenever a new drug is tested against S. aureus infection, it fails after preliminary successes.
The infection of S. aureus is completed within the human body. After S. aureus enters the bloodstream, it will be detected by the immune system. Neutrophils, mast cells and different kinds of immune cells quickly respond to the infection site, causing inflammation reaction and other signaling pathways that command the body to fight against the intruder. While they are still in the bloodstreams, S. aureus have a wide variety of mechanisms to avoid being killed by neutrophils. For example, they release cytotoxic compounds to kill phagocytes which inhibit the function of neutrophils.
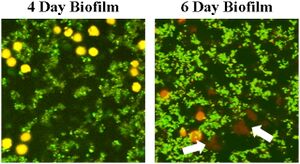
When S. aureus enter the body from (), they travel along the bloodstream to [some organs][cite]. The immune cells in the bloodstreams are a major threat to S. aureus as theyhave to avoid being attacked by the immune system. The strategies used by S.aureus include neutrophils activation and chemotaxis inhibition, phagocytosis inhibition, opsonization suppression, and neutrophils elimination. In specific, S.aureus inhibits phagocytosis by aggregation, protective surface proteins, and biofilm structures and kills neutrophils by cytolytic toxins or apoptosis.
Inhibition of neutrophil extravasation, activation, and chemotaxis
Extravasation inhibition
The extravasation of neutrophils includes tethering, rolling, adhesion, crawling and transmigration. [4] These steps are inhibited by S. aureus to reduce the ability of neutrophils. One way to inhibit extravasation is to inhibit neutrophil rolling. Staphylococcal superantigen-like protein 5 (SSL5), a member of SSL family that is produced by S. aureus is being used to prevent neutrophil rolling. The rolling of neutrophil is primarily promoted by P-selectin glycoprotein ligand-1 (PSGL-1), a glycoprotein binds to P-selectin that is found on white blood cells and endothelial cells. [5] Recent research suggest that during infection, the interaction between PSGL-1 and P-selectin is being disturbed by SSL5 by directly binding to PSGL-1 and competing with antibiotics. [6]
Activation inhibition
The activation of leukocytes is also inhibited by SSL5. [7] Chemoattractants, the small molecules that bind to the receptors on leukocytes, act as an important factor in neutrophil activation, including stimulation, polarization, and locomotion. [8] Thus, in order to limit the function of neutrophils, SSL5 will also target chemoattractants. In the process of inactivation, SSL5 interact to cells with chemokine and anaphylatoxin receptors on the cell surface and directly bind to G protein-coupled receptors (GPCRs). To be more specific, among variety kinds of chemoattractants, C3a, C5a, and CXCL8 induced-neutrophil stimulation is being inhibited by SSL5. [7]
Chemotaxis inhibition
Chemotaxis, the movement of neutrophils responding to chemoattractants [9], is also inhibited by S. aureus. Research showed that chemotaxis inhibitory protein of S. aureus (CHIPS) is responsible for the inhibition of chemotaxis by specifically targeting and inhibiting the C5a- and fMLP-induced responses. When the gene of CHIPS was identified and knocked-out, S. aureus is not able to prevent chemotaxis. [10] To be more specific, CHIPS cut down the mobilization or neutrophils by affecting fMLP or C5a, by directing binding to their receptors.

Avoid phagocytosis by aggregation and biofilm formation
Aggregation
During the infection, S. aureus sometimes form fibrin-containing bacterial aggregates to elude phagocytosis. [1] To achieve agglutination with fibrinogen, S. aureus produces three important products. They are: coagulase (Coa), von Willebrand factor binding protein (vWbp), and clumping factor (Clfa). Interestingly, fibrinogen is a glycoprotein complex that is produced normally by human body to stop bleeding and it is made of three pairs of three chains of Aα-, Bβ-, and γ-chains. [11] The compounds produced by S. aureus, coagulase and vWbp, promotes cleavage of Aα- and Bβ- chains of fibrinogen. [12] Then, S. aureus uses Clfa to bind to fibrin clots and generate fibrin-containing bacterial aggregates. [1]
Inhibition of opsonization
still being edited
Inhibition of neutrophil killing mechanisms
still editing.
Toxin-driven elimination of neutrophils
editing.
Conclusion
Overall text length (all text sections) should be at least 1,000 words (before counting references), with at least 2 images.
Include at least 5 references under References section.
References
- ↑ 1.0 1.1 1.2 Gordon Y. C. Cheung, Justin S. Bae & Michael Otto (2021) Pathogenicity and virulence of Staphylococcus aureus, Virulence, 12:1, 547-569
- ↑ Liu GY, Essex A, Buchanan JT, Datta V, Hoffman HM, Bastian JF, Fierer J, Nizet V. Staphylococcus aureus golden pigment impairs neutrophil killing and promotes virulence through its antioxidant activity. J Exp Med. 2005 Jul 18;202(2):209-15.
- ↑ Agents of Foodborne Illness.
- ↑ Kolaczkowska, E., Kubes, P. Neutrophil recruitment and function in health and inflammation. Nat Rev Immunol 13, 159–175 (2013).
- ↑ Wikipedia: Leukocyte extravasation
- ↑ ovanka Bestebroer, Miriam J. J. G. Poppelier, Laurien H. Ulfman, Peter J. Lenting, Cecile V. Denis, Kok P. M. van Kessel, Jos A. G. van Strijp, Carla J. C. de Haas; Staphylococcal superantigen-like 5 binds PSGL-1 and inhibits P-selectin–mediated neutrophil rolling. Blood 2007; 109 (7): 2936–2943
- ↑ 7.0 7.1 Jovanka Bestebroer, Kok P. M. van Kessel, Hafida Azouagh, Annemiek M. Walenkamp, Ingrid G. J. Boer, Roland A. Romijn, Jos A. G. van Strijp, Carla J. C. de Haas; Staphylococcal SSL5 inhibits leukocyte activation by chemokines and anaphylatoxins. Blood 2009; 113 (2): 328–337
- ↑ Douglas J. Weiss, Bruce Walcheck, in Clinical Biochemistry of Domestic Animals (Sixth Edition), 2008
- ↑ Wikipedia: Chemotaxis
- ↑ de Haas CJ, Veldkamp KE, Peschel A, Weerkamp F, Van Wamel WJ, Heezius EC, Poppelier MJ, Van Kessel KP, van Strijp JA. Chemotaxis inhibitory protein of Staphylococcus aureus, a bacterial antiinflammatory agent. J Exp Med. 2004 Mar 1;199(5):687-95.
- ↑ Wikipedia: Fibrinogen
- ↑ McAdow M, Kim HK, Dedent AC, Hendrickx AP, Schneewind O, Missiakas DM. Preventing Staphylococcus aureus sepsis through the inhibition of its agglutination in blood. PLoS Pathog. 2011 Oct;7(10):e1002307.
Edited by Reina He, student of Joan Slonczewski for BIOL 116 Information in Living Systems, 2022, Kenyon College.
