Small Intestinal Bacterial Overgrowth: Difference between revisions
| Line 14: | Line 14: | ||
“The current gold standard, small-bowel aspiration, and quantitative culture is limited by its high cost, invasive nature, lack of standardization, sampling error, and need for dedicated infrastructure.” | “The current gold standard, small-bowel aspiration, and quantitative culture is limited by its high cost, invasive nature, lack of standardization, sampling error, and need for dedicated infrastructure.” | ||
The hydrogen breath test(BT) is a commonly used form of screening for SIBO. Bond and Levitt first applied the hydrogen breath test to prove that hydrogen concentration in breath is related to the malabsorption of certain sugars in the GI tract in 1978. <ref name="Bond">[https://doi.org/10.1093/ajcn/31.10.s169 Bond, John H., and Michael D. Levitt. “Effect of Dietary Fiber on Intestinal Gas Production and Small Bowel Transit Time in Man.” The American Journal of Clinical Nutrition, vol. 31, no. 10, 1978, https://doi.org/10.1093/ajcn/31.10.s169]</ref> Most commonly used agents in BT that screens for SIBO are lactulose and glucose breath tests, while lactose, fructose, and sorbitol should not be used as agents for testing SIBO. (LBT and GBT, respectively) <ref name="Saad"></ref><ref name= | The hydrogen breath test(BT) is a commonly used form of screening for SIBO. Bond and Levitt first applied the hydrogen breath test to prove that hydrogen concentration in breath is related to the malabsorption of certain sugars in the GI tract in 1978. <ref name="Bond">[https://doi.org/10.1093/ajcn/31.10.s169 Bond, John H., and Michael D. Levitt. “Effect of Dietary Fiber on Intestinal Gas Production and Small Bowel Transit Time in Man.” The American Journal of Clinical Nutrition, vol. 31, no. 10, 1978, https://doi.org/10.1093/ajcn/31.10.s169]</ref> Most commonly used agents in BT that screens for SIBO are lactulose and glucose breath tests, while lactose, fructose, and sorbitol should not be used as agents for testing SIBO. (LBT and GBT, respectively) <ref name="Saad"></ref><ref name="Losurdo"></ref> The procedure is based on the process of hydrogen production in the human GI tract. <ref name=""></ref> | ||
Critique | Critique | ||
Revision as of 06:03, 8 December 2022
Overview
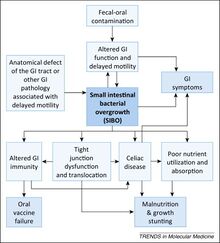
Small intestinal bacterial overgrowth (SIBO) is defined as the abnormal increase in the overall bacterial population in the small intestine. [1][2] Common symptoms of SIBO include diarrhea, flatulence, abdominal pain, malabsorption, and bloating. [1][3][4] More severe cases might be presented with malnutrition due to malabsorption.[4] Currently, there is no single valid test for SIBO, but common ways of screening for SIBO include small-bowel aspiration and quantitative culture and breath testing.[3][5] Risk factors for SIBO includes gastric surgery, injury or structural defects in the GI tract, especially in the small intestine, fistula in the bowel, Crohn’s disease, intestinal tumors, history of abdominal radiation therapy, diabetes, diverticulosis in the small intestine, and adhesions. [1]
SIBO was first suggested by Barker and Hummel in their 1939 publication “Macrocytic anemia in association with intestinal strictures and anastomoses.”, which provides key findings for both the study of macrocytic anemia and the study of SIBO. [7]
As the name suggests, bacteria involved in SIBO is coliform bacteria, bacteria that are present in the digestive tract. [8]
Testing for SIBO
Small bowel aspiration and quantitative culture (“Saad”) “The current gold standard, small-bowel aspiration, and quantitative culture is limited by its high cost, invasive nature, lack of standardization, sampling error, and need for dedicated infrastructure.”
The hydrogen breath test(BT) is a commonly used form of screening for SIBO. Bond and Levitt first applied the hydrogen breath test to prove that hydrogen concentration in breath is related to the malabsorption of certain sugars in the GI tract in 1978. [9] Most commonly used agents in BT that screens for SIBO are lactulose and glucose breath tests, while lactose, fructose, and sorbitol should not be used as agents for testing SIBO. (LBT and GBT, respectively) [5][10] The procedure is based on the process of hydrogen production in the human GI tract. Cite error: Invalid <ref> tag; refs with no name must have content
Critique “The accuracy of all current tests remains limited due to the failure of culture to be a gold standard and the lack of standardization of the normal bowel flora in the small intestine” [3]
Improvements to the BT A study published in Clinical Gastroenterology and Hepatology suggests that the diagnostic accuracy of hydrogen breath testing for SIBO can be maximized by careful patient selection, proper preparation, and standardization of test performance and interpretation.[5] The authors also suggest testing both methane and hydrogen concentrations for better accuracy. [5]
Medical Management of SIBO
Unfortunately, the current management of SIBO is unclear and mostly empirical. [4][11] Common management strategies include using antibiotics and probiotics.[11][12]
Other strategies for management besides eliminating overgrowth include treating underlying conditions that caused overgrowth and addressing nutritional deficiencies potentially caused by SIBO. [3]
Research also proposes dietary changes to help relieve the functional gastrointestinal (GI) symptoms. [13] Reduce intake of FODMAPs (fermentable oligo-, di-, and mono-saccharides and polyols)—poorly absorbed short-chain carbohydrates can effectively reduce bloating and other functional gastrointestinal symptoms. [13] Although the effectiveness of this strategy—previously used only to treat IBS and other GI conditions—for treating SIBO-related symptoms is still unclear. [14] Other food sources of functional gastrointestinal symptoms including gluten and natural and added food chemicals such as amines and glutamates and the benefit of dietary strategies that reduce the intake of these chemicals are still being researched. [13]
Interactions Between SIBO and Other Systemic Conditions
Although the prevalence and role in the pathogenesis of other diseases remain uncertain, reviews and case studies still show potential connections between SIBO and other systemic conditions such as irritable bowel syndrome(IBS) or Ehlers-Danlos Syndrome. [2] Other conditions that are hypothesized to be associated with SIBO include cirrhosis, chronic pancreatitis, and celiac disease. [4]
Ehlers-Danlos Syndrome is a group of rare disorders caused by collagen synthesis defects. [15] Delayed gastric emptying, which is a risk factor for SIBO, is common among EDS patients. [4][16][17] Studies show that SIBO diagnosis is common among EDS patients. [16] Another study suggests that EDS might be correlated with the constipation predominant type of SIBO instead of the diarrhea predominant type. [18] Yet because EDS is quite rare among the general population, sample sizes are small for most researches done on EDS patients, especially those involving other comorbidities, which limits the scope of research.[15][18]
Conclusion
Since SIBO is a fairly common condition, there is a general overview of its nature, yet the diagnostic criteria and treatment are mostly based on empirical evidence instead of quantitative research. [4][11][12] In the past few years there has been more literature discussing and criticizing the previous approaches to diagnosing and treating SIBO and more research done on interactions between SIBO and other conditions.
References
- ↑ 1.0 1.1 1.2 “Small Intestinal Bacterial Overgrowth (SIBO).” Mayo Clinic, Mayo Foundation for Medical Education and Research, 6 Jan. 2022, https://www.mayoclinic.org/diseases-conditions/small-intestinal-bacterial-overgrowth/symptoms-causes/syc-20370168.
- ↑ 2.0 2.1 Adike, Abimbola, and John K. DiBaise. “Small Intestinal Bacterial Overgrowth.” Gastroenterology Clinics of North America, vol. 47, no. 1, 2018, pp. 193–208., https://doi.org/10.1016/j.gtc.2017.09.008.
- ↑ 3.0 3.1 3.2 3.3 Sachdev, Amit H, and Mark Pimentel. “Gastrointestinal bacterial overgrowth: pathogenesis and clinical significance.” Therapeutic advances in chronic disease vol. 4,5 (2013): 223-31. doi:10.1177/2040622313496126
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 Bohm, Matthew, et al. “Diagnosis and Management of Small Intestinal Bacterial Overgrowth.” Nutrition in Clinical Practice, vol. 28, no. 3, 2013, pp. 289–299., https://doi.org/10.1177/0884533613485882.
- ↑ 5.0 5.1 5.2 5.3 Saad, Richard J., and William D. Chey. “Breath Testing for Small Intestinal Bacterial Overgrowth: Maximizing Test Accuracy.” Clinical Gastroenterology and Hepatology, vol. 12, no. 12, 2014, pp. 1964–1972., https://doi.org/10.1016/j.cgh.2013.09.055
- ↑ Donowitz, Jeffrey R., and William A. Petri. “Pediatric Small Intestine Bacterial Overgrowth in Low-Income Countries.” Trends in Molecular Medicine, vol. 21, no. 1, 2015, pp. 6–15., https://doi.org/10.1016/j.molmed.2014.11.001
- ↑ Barker, W. H., and L. E. Hummel. "Macrocytic anemia in association with intestinal strictures and anastomoses." Bull Johns Hopkins Hosp 64.2 (1939): 15.
- ↑ “Department of Health.” Coliform Bacteria in Drinking Water Supplies, July 2017, https://www.health.ny.gov/environmental/water/drinking/coliform_bacteria.htm.
- ↑ Bond, John H., and Michael D. Levitt. “Effect of Dietary Fiber on Intestinal Gas Production and Small Bowel Transit Time in Man.” The American Journal of Clinical Nutrition, vol. 31, no. 10, 1978, https://doi.org/10.1093/ajcn/31.10.s169
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedLosurdo - ↑ 11.0 11.1 11.2 Leonello, R., et al. “P.12.7 Outcome of Patients with Positive Breath Test for SIBO Six Months after Combined Treatment with Rifaximin and Probiotics.” Digestive and Liver Disease, vol. 48, 2016, https://doi.org/10.1016/s1590-8658(16)30289-4
- ↑ 12.0 12.1 Richard, Nicolas, et al. “The Effectiveness of Rotating versus Single Course Antibiotics for Small Intestinal Bacterial Overgrowth.” United European Gastroenterology Journal, vol. 9, no. 6, 2021, pp. 645–654., https://doi.org/10.1002/ueg2.12116
- ↑ 13.0 13.1 13.2 Gibson, Peter R, and Susan J Shepherd. “Food Choice as a Key Management Strategy for Functional Gastrointestinal Symptoms.” American Journal of Gastroenterology, vol. 107, no. 5, 2012, pp. 657–666., https://doi.org/10.1038/ajg.2012.49
- ↑ Adike, Abimbola, and John K. DiBaise. “Small Intestinal Bacterial Overgrowth.” Gastroenterology Clinics of North America, vol. 47, no. 1, 2018, pp. 193–208., https://doi.org/10.1016/j.gtc.2017.09.008.
- ↑ 15.0 15.1 “Ehlers-Danlos Syndrome: Medlineplus Genetics.” MedlinePlus, U.S. National Library of Medicine, https://medlineplus.gov/genetics/condition/ehlers-danlos-syndrome/#frequency.
- ↑ 16.0 16.1 Xiong, Tingting, et al. “1182 Small Intestinal Bacterial Overgrowth (SIBO) Is Common in Patients with Ehlers-Danlos Syndrome (EDS).” American Journal of Gastroenterology, vol. 114, no. 1, 2019, https://doi.org/10.14309/01.ajg.0000594256.00026.1d
- ↑ Nelson, A. D., et al. “Ehlers Danlos Syndrome and Gastrointestinal Manifestations: A 20-Year Experience at Mayo Clinic.” Neurogastroenterology & Motility, vol. 27, no. 11, 2015, pp. 1657–1666., https://doi.org/10.1111/nmo.12665
- ↑ 18.0 18.1 Zhou, Wendy DO1; Zikos, Thomas MD2; Neshatian, Leila MD3; Nguyen, Linda MD3. S0476 High Prevalence of Methane Predominant Small Bowel Bacterial Overgrowth and Constipation in Patients With Hypermobile Ehlers-Danlos Syndrome. The American Journal of Gastroenterology: October 2020 - Volume 115 - Issue - p S238 doi: 10.14309/01.ajg.0000703952.17443.b0
Edited by Yufan Lu, student of Joan Slonczewski for BIOL 116 Information in Living Systems, 2022, Kenyon College.
