Small Intestinal Bacterial Overgrowth: Difference between revisions
| (102 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
==Overview== | ==Overview== | ||
Small intestinal bacterial overgrowth (SIBO) is defined as the abnormal increase in the overall bacterial population in the small intestine. <ref name="Mayo">[https://www.mayoclinic.org/diseases-conditions/small-intestinal-bacterial-overgrowth/symptoms-causes/syc-20370168. “Small Intestinal Bacterial Overgrowth (SIBO).” Mayo Clinic, Mayo Foundation for Medical Education and Research, 6 Jan. 2022, https://www.mayoclinic.org/diseases-conditions/small-intestinal-bacterial-overgrowth/symptoms-causes/syc-20370168.]</ref> | Small intestinal bacterial overgrowth (SIBO) is defined as the abnormal increase in the overall bacterial population in the small intestine.<ref name="Mayo">[https://www.mayoclinic.org/diseases-conditions/small-intestinal-bacterial-overgrowth/symptoms-causes/syc-20370168. “Small Intestinal Bacterial Overgrowth (SIBO).” Mayo Clinic, Mayo Foundation for Medical Education and Research, 6 Jan. 2022, https://www.mayoclinic.org/diseases-conditions/small-intestinal-bacterial-overgrowth/symptoms-causes/syc-20370168.]</ref> Other sources suggest that SIBO is defined by the presence of abnormally high level of bacteria in the small intestine.<ref name="Sachdev">[https://doi.org/10.1177/2040622313496126 Sachdev, Amit H, and Mark Pimentel. “Gastrointestinal bacterial overgrowth: pathogenesis and clinical significance.” Therapeutic advances in chronic disease vol. 4,5 (2013): 223-31. doi:10.1177/2040622313496126]</ref><ref name="Bohm">[https://doi.org/10.1177/0884533613485882 Bohm, Matthew, et al. “Diagnosis and Management of Small Intestinal Bacterial Overgrowth.” Nutrition in Clinical Practice, vol. 28, no. 3, 2013, pp. 289–299., https://doi.org/10.1177/0884533613485882]</ref><ref name="MedlinePlusSIBO">[https://medlineplus.gov/ency/article/000222.htm Lehrer, Jenifer K. “Small Bowel Bacterial Overgrowth: Medlineplus Medical Encyclopedia.” MedlinePlus, U.S. National Library of Medicine, 27 May 2020, https://medlineplus.gov/ency/article/000222.htm.]</ref><ref name="Rana">[https://doi.org/10.1007/s12291-014-0426-4 Rana, Satya Vati, and Aastha Malik. “Hydrogen Breath Tests in Gastrointestinal Diseases.” Indian Journal of Clinical Biochemistry, vol. 29, no. 4, 2014, pp. 398–405., https://doi.org/10.1007/s12291-014-0426-4]</ref> Another source suggests that there has been no consensus on the definition of SIBO.<ref name="Adike">[https://doi.org/10.1016/j.gtc.2017.09.008 Adike, Abimbola, and John K. DiBaise. “Small Intestinal Bacterial Overgrowth.” Gastroenterology Clinics of North America, vol. 47, no. 1, 2018, pp. 193–208., https://doi.org/10.1016/j.gtc.2017.09.008.]</ref> | ||
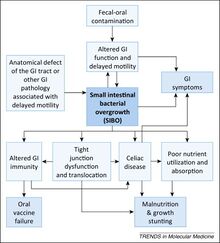
Common symptoms of SIBO include diarrhea, flatulence, abdominal pain, malabsorption, and bloating.<ref name="Mayo"></ref><ref name="Sachdev"></ref><ref name="MedlinePlusSIBO"></ref><ref name="Donowitz"></ref> More severe cases might be presented with malnutrition due to malabsorption, vitamin deficiency, osteoporosis, and kidney stones.<ref name="Mayo"></ref><ref name="Bohm"></ref> Currently, there is no single valid test for SIBO, but common ways of screening for SIBO include small-bowel aspiration and quantitative culture and breath testing.<ref name="Sachdev"></ref><ref name="Saad">[https://doi.org/10.1016/j.cgh.2013.09.055 Saad, Richard J., and William D. Chey. “Breath Testing for Small Intestinal Bacterial Overgrowth: Maximizing Test Accuracy.” Clinical Gastroenterology and Hepatology, vol. 12, no. 12, 2014, pp. 1964–1972., https://doi.org/10.1016/j.cgh.2013.09.055]</ref> Risk factors for SIBO includes gastric surgery, injury or structural defects in the gastrointestinal(GI) tract, especially in the small intestine, fistula in the bowel, Crohn’s disease, intestinal tumors, history of abdominal radiation therapy, diabetes, diverticulosis in the small intestine, and intestinal adhesions.<ref name=Mayo></ref><ref name="Donowitz"></ref> SIBO is also found in children in unsanitary conditions and those who do not have access to clean water.<ref name="Donowitz"></ref> | |||
[[Image:SIBOFigure1.jpeg|thumb|220px|left|<b>Figure 1.</b> Hypothesis of SIBO of potentially detrimental outcomes for children in developing countries.<ref name="Donowitz">[https://doi.org/10.1016/j.molmed.2014.11.001 Donowitz, Jeffrey R., and William A. Petri. “Pediatric Small Intestine Bacterial Overgrowth in Low-Income Countries.” Trends in Molecular Medicine, vol. 21, no. 1, 2015, pp. 6–15., https://doi.org/10.1016/j.molmed.2014.11.001]</ref>]] | |||
As the name suggests, bacteria involved in SIBO | As the name suggests, bacteria involved in SIBO are coliform bacteria, bacteria that are present in the colon.<ref name="Mayo"></ref><ref name="Bohm"></ref><ref name="Adike"></ref><ref name=”NYGov”>[https://www.health.ny.gov/environmental/water/drinking/coliform_bacteria.htm “Coliform Bacteria in Drinking Water Supplies”, NY Department of Health, July 2017, https://www.health.ny.gov/environmental/water/drinking/coliform_bacteria.htm.]</ref><ref name="MRBDC">[https://mrbdc.mnsu.edu/sites/mrbdc.mnsu.edu/files/public/major/gbe/gbe_tmdl/fecal.html “Fecal Coliform Bacteria.” Blue Earth River Basin Fecal Coliform Bacteria TMDL, https://mrbdc.mnsu.edu/sites/mrbdc.mnsu.edu/files/public/major/gbe/gbe_tmdl/fecal.html.]</ref> The presence of coliform can be used to indicate that matter of fecal origin may be present.<ref name="Li">[https://doi.org/10.1016/B978-0-12-811330-1.00012-0 Li, Daoliang, and Shuangyin Liu. “Chapter 12 - Water Quality Monitoring in Aquaculture.” Water Quality Monitoring and Management: Basis, Technology and Case Studies, Academic Press, London, England, 2019, pp. 303–328, https://doi.org/10.1016/B978-0-12-811330-1.00012-0. Accessed 8 Dec. 2022.]</ref> | ||
[[Image:SIBOFigure2.jpeg|thumb|220px|right|<b>Figure 2.</b> The Sources of Fecal Coliform Bacteria.<ref name="MRBDC"></ref>]] | |||
Like many other diseases, the prevalence of SIBO has socioeconomic disparities.<ref name="Donowitz"></ref> Besides the physiological factors listed above, living in impoverished conditions is another risk factor for SIBO.<ref name="Donowitz"></ref><ref name="Mello">[https://pubmed.ncbi.nlm.nih.gov/23139610/ Mello, Carolina Santos. “Methane Production and Small Intestinal Bacterial Overgrowth in Children Living in a Slum.” World Journal of Gastroenterology, vol. 18, no. 41, 2012, p. 5932., https://doi.org/10.3748/wjg.v18.i41.5932. ]</ref> Although research is limited in this intersectional area,<ref name="Donowitz"></ref>, because SIBO may cause nutritional malabsorption and decrease the efficiency of oral vaccines,<ref name="Lagos">[https://doi.org/10.1086/315051 Lagos, Rosanna, et al. “Effect of Small Bowel Bacterial Overgrowth on the Immunogenicity of Single‐Dose Live Oral Cholera Vaccine CVD 103‐HGR.” The Journal of Infectious Diseases, vol. 180, no. 5, 1999, pp. 1709–1712., https://doi.org/10.1086/315051. ]</ref> it can affect life quality of children significantly.<ref name="Donowitz"></ref> | |||
==Testing for SIBO== | ==Testing for SIBO== | ||
The two most common ways of screening for SIBO are small bowel aspiration and quantitative culture.<ref name="Mayo2">[https://www.mayoclinic.org/diseases-conditions/small-intestinal-bacterial-overgrowth/diagnosis-treatment/drc-20370172 “Small Intestinal Bacterial Overgrowth (SIBO).” Mayo Clinic, Mayo Foundation for Medical Education and Research, 6 Jan. 2022, https://www.mayoclinic.org/diseases-conditions/small-intestinal-bacterial-overgrowth/diagnosis-treatment/drc-20370172.]</ref> | |||
( | |||
===Small Bowel Aspirate and Fluid Culture=== | |||
Small bowel aspirate and fluid culture, the current "gold standard" for diagnosing SIBO, is limited by the invasive test procedure and high cost.<ref name="Saad"></ref><ref name="Mayo2"></ref> To screen for SIBO using quantitative culture, medical professionals insert an endoscope down the patient's upper digestive tract and obtain a fluid sample from the patient's intestine.<ref name="Mayo2"></ref> The fluid sample is subsequently used for lab testing for bacterial growth.<ref name="Mayo2"></ref> The current diagnostic criteria for SIBO is the presence of coliform bacteria with >10<sup>5</sup> colony-forming units/mL when the normal amount ranges from 10<sup>2</sup>–10<sup>3</sup> to 10<sup>8</sup> colony-forming units(CFU)/ml in the small intestines.<ref name="Bohm"></ref><ref name="Donowitz"></ref> | |||
===Hydrogen Breath Test (BT)=== | |||
A study published in Clinical Gastroenterology and Hepatology suggests that the diagnostic accuracy of hydrogen breath testing for SIBO can be maximized by careful patient selection, proper preparation, and standardization of test performance and interpretation.<ref name="Saad"></ref> The authors also suggest testing both methane and hydrogen concentrations for better accuracy. <ref name="Saad"></ref> | The hydrogen breath test (BT) is a commonly used form of screening for SIBO. The procedure is based on the process of hydrogen production in the human GI tract.<ref name="Rana"></ref> Bacteria in the bowel produce hydrogen due to the fermentation of carbohydrates that are not digested or absorbed in the small intestine and travels into the large intestine instead.<ref name="Rana"></ref> Most of the bacteria-produced hydrogen is absorbed into the blood through the colon lining.<ref name="Rana"></ref> As the hydrogen moves along the bloodstream to the lungs, hydrogen gas is exchanged out of the blood and into the airways and exhaled by the patient.<ref name="Rana"></ref> This process is the sole source of H<sub>2</sub> gas in the human breath.<ref name="Rana"></ref> The most commonly used agents in BT that screens for SIBO are lactulose and glucose breath tests(LBT and GBT, respectively).<ref name="Saad"></ref><ref name="Losurdo">[https://doi.org/10.5056/jnm19113 Losurdo, Giuseppe, et al. “Breath Tests for the Non-Invasive Diagnosis of Small Intestinal Bacterial Overgrowth: A Systematic Review with Meta-Analysis.” Journal of Neurogastroenterology and Motility, vol. 26, no. 1, 2020, pp. 16–28., https://doi.org/10.5056/jnm19113]</ref> Glucose is absorbed in healthy individuals' intestines yet malabsorption of glucose happens in the intestines of those with SIBO.<ref name="Bond">[https://doi.org/10.1172/jci106916 Bond, John H., and Michael D. Levitt. “Use of Pulmonary Hydrogen (H2) Measurements to Quantitate Carbohydrate Absorption.” Journal of Clinical Investigation, vol. 51, no. 5, 1972, pp. 1219–1225., https://doi.org/10.1172/jci106916. ]</ref> For lactulose, the case is entirely different. Lactulose is not absorbed in healthy individuals, which means almost all(more than 99%) of ingested lactulose is fermented in the large intestine.<ref name="Ruszkowski">[https://doi.org/10.1016/j.anaerobe.2019.06.002 Ruszkowski, Jakub, and Jacek M. Witkowski. “Lactulose: Patient- and Dose-Dependent Prebiotic Properties in Humans.” Anaerobe, vol. 59, 2019, pp. 100–106., https://doi.org/10.1016/j.anaerobe.2019.06.002]</ref> But for individuals with SIBO, there is excessive lactulose fermentation in the large bowel, signified by a significant increase in hydrogen exhale.<ref name="Ruszkowski"></ref> | ||
Lactose and fructose, although common agents for BT, should not be used as agents for testing SIBO because other underlying conditions unrelated to SIBO such as lactose intolerance or fructose malabsorption may affect test results.<ref name="Rana"></ref><ref name="Saad"></ref> Sorbitol should not be used as a BT agent for SIBO-screening purposes because of similar reasons.<ref name="Saad"></ref> Individuals without SIBO may suffer from bloating and other GI issues after ingesting sorbitol thus using sorbitol as a test agent might affect test accuracy.<ref name="Rana"></ref> | |||
A study published in Clinical Gastroenterology and Hepatology suggests that the diagnostic accuracy of hydrogen breath testing for SIBO can be maximized by careful patient selection, proper preparation, and standardization of test performance and interpretation.<ref name="Saad"></ref> The authors also suggest testing both methane and hydrogen concentrations for better accuracy, which is backed up by Mayo Clinic.<ref name="Saad"></ref><ref name="Mayo2"></ref> Another improvement suggested through literature includes decreasing test time from 100 minutes after ingestion of lactulose to 60 and 80 minutes after ingestion to prevent false positives.<ref name="Sunny">[https://doi.org/10.1016/j.amjms.2015.12.008 Sunny, Joseph K., et al. “Interpreting the Lactulose Breath Test for the Diagnosis of Small Intestinal Bacterial Overgrowth.” The American Journal of the Medical Sciences, vol. 351, no. 3, 2016, pp. 229–232., https://doi.org/10.1016/j.amjms.2015.12.008.]</ref> A study on SIBO among children living in developing countries also discusses the lack of data on efficiency of these test methods on children.<ref name="Donowitz"></ref> | |||
==Medical Management of SIBO== | ==Medical Management of SIBO== | ||
Unfortunately, the current management strategies for SIBO are mostly empirical. <ref name ="Bohm"></ref><ref name="Leonello">[https://doi.org/10.1016/s1590-8658(16)30289-4 Leonello, R., et al. “P.12.7 Outcome of Patients with Positive Breath Test for SIBO Six Months after Combined Treatment with Rifaximin and Probiotics.” Digestive and Liver Disease, vol. 48, 2016, https://doi.org/10.1016/s1590-8658(16)30289-4]</ref> Common management strategies include using antibiotics and probiotics.<ref name="Leonello"></ref><ref name="Richard">[https://doi.org/10.1002/ueg2.12116 Richard, Nicolas, et al. “The Effectiveness of Rotating versus Single Course Antibiotics for Small Intestinal Bacterial Overgrowth.” United European Gastroenterology Journal, vol. 9, no. 6, 2021, pp. 645–654., https://doi.org/10.1002/ueg2.12116]</ref> Other strategies for management besides eliminating overgrowth include treating underlying conditions that caused overgrowth and addressing nutritional deficiencies potentially caused by SIBO. <ref name="Sachdev"></ref> | Unfortunately, the current management strategies for SIBO are mostly empirical.<ref name ="Bohm"></ref><ref name="Leonello">[https://doi.org/10.1016/s1590-8658(16)30289-4 Leonello, R., et al. “P.12.7 Outcome of Patients with Positive Breath Test for SIBO Six Months after Combined Treatment with Rifaximin and Probiotics.” Digestive and Liver Disease, vol. 48, 2016, https://doi.org/10.1016/s1590-8658(16)30289-4]</ref> Common management strategies include using antibiotics and probiotics.<ref name="Mayo2"></ref><ref name="Leonello"></ref><ref name="Richard">[https://doi.org/10.1002/ueg2.12116 Richard, Nicolas, et al. “The Effectiveness of Rotating versus Single Course Antibiotics for Small Intestinal Bacterial Overgrowth.” United European Gastroenterology Journal, vol. 9, no. 6, 2021, pp. 645–654., https://doi.org/10.1002/ueg2.12116]</ref> Other strategies for management besides eliminating overgrowth include treating underlying conditions that caused overgrowth and addressing nutritional deficiencies potentially caused by SIBO.<ref name="Sachdev"></ref> | ||
Research also proposes dietary changes to help relieve the functional gastrointestinal (GI) symptoms. <ref name="Gibson"> [https://doi.org/10.1038/ajg.2012.49 Gibson, Peter R, and Susan J Shepherd. “Food Choice as a Key Management Strategy for Functional Gastrointestinal Symptoms.” American Journal of Gastroenterology, vol. 107, no. 5, 2012, pp. 657–666., https://doi.org/10.1038/ajg.2012.49] </ref> Reduce intake of FODMAPs (fermentable oligo-, di-, and mono-saccharides and polyols)—poorly absorbed | Research also proposes dietary changes to help relieve the functional gastrointestinal (GI) symptoms.<ref name="Gibson"> [https://doi.org/10.1038/ajg.2012.49 Gibson, Peter R, and Susan J Shepherd. “Food Choice as a Key Management Strategy for Functional Gastrointestinal Symptoms.” American Journal of Gastroenterology, vol. 107, no. 5, 2012, pp. 657–666., https://doi.org/10.1038/ajg.2012.49] </ref> Reduce intake of FODMAPs (fermentable oligo-, di-, and mono-saccharides and polyols)—poorly absorbed carbohydrates can effectively reduce bloating and other functional gastrointestinal symptoms.<ref name="Gibson"></ref><ref name="Biesiekierski">[https://doi.org/10.1016/j.coph.2022.102208 Biesiekierski, Jessica R., and Caroline J. Tuck. “Low Fodmap Diet beyond IBS: Evidence for Use in Other Conditions.” Current Opinion in Pharmacology, vol. 64, 2022, p. 102208., https://doi.org/10.1016/j.coph.2022.102208]</ref> Although the effectiveness of this strategy—previously used only to treat IBS and other GI conditions—for treating SIBO-related symptoms is still unclear.<ref name="Adike"></ref> Other food sources of functional gastrointestinal symptoms including gluten and natural and added food chemicals such as amines and glutamates and the benefit of dietary strategies that reduce the intake of these chemicals are still being researched.<ref name="Gibson"></ref> | ||
<ref name= | |||
==Interactions Between SIBO and Other Systemic Conditions== | ==Interactions Between SIBO and Other Systemic Conditions== | ||
Although the prevalence and role in the pathogenesis of other diseases remain uncertain, reviews and case studies still show potential connections between SIBO and other systemic conditions such as irritable bowel syndrome(IBS) or Ehlers-Danlos Syndrome. <ref name="Adike"></ref> Other conditions that are hypothesized to be associated with SIBO include cirrhosis, chronic pancreatitis, and celiac disease. <ref name="Bohm"></ref> < | Although the prevalence and role in the pathogenesis of other diseases remain uncertain, reviews and case studies still show potential connections between SIBO and other systemic conditions such as irritable bowel syndrome (IBS) or Ehlers-Danlos Syndrome (EDS).<ref name="Rana"></ref><ref name="Adike"></ref> Other conditions that are hypothesized to be associated with SIBO include cirrhosis, chronic pancreatitis, and celiac disease.<ref name="Bohm"></ref><ref name="Rana"></ref><ref name="Donowitz"></ref> | ||
===SIBO and Ehlers-Danlos Syndrome (EDS)=== | |||
Ehlers-Danlos Syndrome is a group of rare disorders caused by collagen synthesis defects.<ref name="MedlinePlusEDS">[https://medlineplus.gov/genetics/condition/ehlers-danlos-syndrome/#frequency. “Ehlers-Danlos Syndrome: Medlineplus Genetics.” MedlinePlus, U.S. National Library of Medicine, https://medlineplus.gov/genetics/condition/ehlers-danlos-syndrome/#frequency.]</ref> Delayed gastric emptying, which is a risk factor for SIBO, is common among EDS patients.<ref name="Bohm"></ref><ref name=“Xiong”>[https://doi.org/10.14309/01.ajg.0000594256.00026.1d Xiong, Tingting, et al. “1182 Small Intestinal Bacterial Overgrowth (SIBO) Is Common in Patients with Ehlers-Danlos Syndrome (EDS).” American Journal of Gastroenterology, vol. 114, no. 1, 2019, https://doi.org/10.14309/01.ajg.0000594256.00026.1d] </ref><ref name= Nelson>[https://doi.org/10.1111/nmo.12665 Nelson, A. D., et al. “Ehlers Danlos Syndrome and Gastrointestinal Manifestations: A 20-Year Experience at Mayo Clinic.” Neurogastroenterology & Motility, vol. 27, no. 11, 2015, pp. 1657–1666., https://doi.org/10.1111/nmo.12665] </ref> Studies show that SIBO diagnosis is common among EDS patients.<ref name=“Xiong”></ref> Another study suggests that EDS might be correlated with the constipation-predominant type of SIBO instead of the diarrhea-predominant type.<ref name=“Zhou”> [https://journals.lww.com/ajg/Fulltext/2020/10001/S0476_High_Prevalence_of_Methane_Predominant_Small.477.aspx Zhou, Wendy, et al. S0476 High Prevalence of Methane Predominant Small Bowel Bacterial Overgrowth and Constipation in Patients With Hypermobile Ehlers-Danlos Syndrome. The American Journal of Gastroenterology: October 2020 - Volume 115 - Issue - p S238 doi: 10.14309/01.ajg.0000703952.17443.b0 ]</ref> Yet because EDS is quite rare among the general population, sample sizes are small for most research done on EDS patients, especially those involving other comorbidities, which limits the scope of research.<ref name="MedlinePlusEDS"></ref><ref name=“Zhou”></ref> | |||
===SIBO and Irritable Bowel Syndrome (IBS)=== | |||
The relationship between IBS and SIBO is even more complicated because they both affect the GI system, as the names suggest. IBS is a common disorder that affects the large intestines.<ref name="MedlinePlusIBS">[https://medlineplus.gov/irritablebowelsyndrome.html “Irritable Bowel Syndrome | IBS.” MedlinePlus, U.S. National Library of Medicine, 2018, https://medlineplus.gov/irritablebowelsyndrome.html.]</ref><ref name="MayoIBS">[https://www.mayoclinic.org/diseases-conditions/irritable-bowel-syndrome/symptoms-causes/syc-20360016 “Irritable Bowel Syndrome.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 2 Nov. 2022, https://www.mayoclinic.org/diseases-conditions/irritable-bowel-syndrome/symptoms-causes/syc-20360016]</ref> The symptoms of IBS are similar to those of SIBO, including abdominal pain, bloating, gas, and diarrhea and/or constipation.<ref name="Rana"></ref><ref name="MayoIBS"></ref><ref name="NIDDK">[https://www.niddk.nih.gov/health-information/digestive-diseases/irritable-bowel-syndrome/symptoms-causes “Symptoms & Causes of Irritable Bowel Syndrome.” National Institute of Diabetes and Digestive and Kidney Diseases, U.S. Department of Health and Human Services, 2017, https://www.niddk.nih.gov/health-information/digestive-diseases/irritable-bowel-syndrome/symptoms-causes.]</ref> A review published on <i>The Lancet Gastroenterology & Hepatology</i> suggests that evidence between the link of SIBO and IBS is weak contrary to popular belief.<ref name="Aziz">[https://doi.org/10.1016/s2468-1253(20)30212-0 Aziz, Imran, and Magnus Simrén. “The Overlap between Irritable Bowel Syndrome and Organic Gastrointestinal Diseases.” The Lancet Gastroenterology & Hepatology, vol. 6, no. 2, 2021, pp. 139–148., https://doi.org/10.1016/s2468-1253(20)30212-0]</ref> | |||
==Conclusion== | ==Conclusion== | ||
Since SIBO is a fairly common condition, there is a general overview of its nature, yet the diagnostic criteria and treatment are mostly based on empirical evidence instead of quantitative research. <ref name="Bohm"></ref><ref name="Leonello"></ref><ref name="Richard"></ref> | Since SIBO is a fairly common condition, there is a general overview of its nature, yet the diagnostic criteria and treatment are mostly based on empirical evidence instead of quantitative research.<ref name="Bohm"></ref><ref name="Leonello"></ref><ref name="Richard"></ref> But in the past few years, there has been more literature discussing and criticizing the previous approaches to diagnosing and treating SIBO and more research done on interactions between SIBO and other conditions.<ref name="Adike"></ref> | ||
==References== | ==References== | ||
Latest revision as of 13:18, 9 December 2022
Overview
Small intestinal bacterial overgrowth (SIBO) is defined as the abnormal increase in the overall bacterial population in the small intestine.[1] Other sources suggest that SIBO is defined by the presence of abnormally high level of bacteria in the small intestine.[2][3][4][5] Another source suggests that there has been no consensus on the definition of SIBO.[6]
Common symptoms of SIBO include diarrhea, flatulence, abdominal pain, malabsorption, and bloating.[1][2][4][7] More severe cases might be presented with malnutrition due to malabsorption, vitamin deficiency, osteoporosis, and kidney stones.[1][3] Currently, there is no single valid test for SIBO, but common ways of screening for SIBO include small-bowel aspiration and quantitative culture and breath testing.[2][8] Risk factors for SIBO includes gastric surgery, injury or structural defects in the gastrointestinal(GI) tract, especially in the small intestine, fistula in the bowel, Crohn’s disease, intestinal tumors, history of abdominal radiation therapy, diabetes, diverticulosis in the small intestine, and intestinal adhesions.[1][7] SIBO is also found in children in unsanitary conditions and those who do not have access to clean water.[7]
As the name suggests, bacteria involved in SIBO are coliform bacteria, bacteria that are present in the colon.[1][3][6][9][10] The presence of coliform can be used to indicate that matter of fecal origin may be present.[11]
Like many other diseases, the prevalence of SIBO has socioeconomic disparities.[7] Besides the physiological factors listed above, living in impoverished conditions is another risk factor for SIBO.[7][12] Although research is limited in this intersectional area,[7], because SIBO may cause nutritional malabsorption and decrease the efficiency of oral vaccines,[13] it can affect life quality of children significantly.[7]
Testing for SIBO
The two most common ways of screening for SIBO are small bowel aspiration and quantitative culture.[14]
Small Bowel Aspirate and Fluid Culture
Small bowel aspirate and fluid culture, the current "gold standard" for diagnosing SIBO, is limited by the invasive test procedure and high cost.[8][14] To screen for SIBO using quantitative culture, medical professionals insert an endoscope down the patient's upper digestive tract and obtain a fluid sample from the patient's intestine.[14] The fluid sample is subsequently used for lab testing for bacterial growth.[14] The current diagnostic criteria for SIBO is the presence of coliform bacteria with >105 colony-forming units/mL when the normal amount ranges from 102–103 to 108 colony-forming units(CFU)/ml in the small intestines.[3][7]
Hydrogen Breath Test (BT)
The hydrogen breath test (BT) is a commonly used form of screening for SIBO. The procedure is based on the process of hydrogen production in the human GI tract.[5] Bacteria in the bowel produce hydrogen due to the fermentation of carbohydrates that are not digested or absorbed in the small intestine and travels into the large intestine instead.[5] Most of the bacteria-produced hydrogen is absorbed into the blood through the colon lining.[5] As the hydrogen moves along the bloodstream to the lungs, hydrogen gas is exchanged out of the blood and into the airways and exhaled by the patient.[5] This process is the sole source of H2 gas in the human breath.[5] The most commonly used agents in BT that screens for SIBO are lactulose and glucose breath tests(LBT and GBT, respectively).[8][15] Glucose is absorbed in healthy individuals' intestines yet malabsorption of glucose happens in the intestines of those with SIBO.[16] For lactulose, the case is entirely different. Lactulose is not absorbed in healthy individuals, which means almost all(more than 99%) of ingested lactulose is fermented in the large intestine.[17] But for individuals with SIBO, there is excessive lactulose fermentation in the large bowel, signified by a significant increase in hydrogen exhale.[17]
Lactose and fructose, although common agents for BT, should not be used as agents for testing SIBO because other underlying conditions unrelated to SIBO such as lactose intolerance or fructose malabsorption may affect test results.[5][8] Sorbitol should not be used as a BT agent for SIBO-screening purposes because of similar reasons.[8] Individuals without SIBO may suffer from bloating and other GI issues after ingesting sorbitol thus using sorbitol as a test agent might affect test accuracy.[5]
A study published in Clinical Gastroenterology and Hepatology suggests that the diagnostic accuracy of hydrogen breath testing for SIBO can be maximized by careful patient selection, proper preparation, and standardization of test performance and interpretation.[8] The authors also suggest testing both methane and hydrogen concentrations for better accuracy, which is backed up by Mayo Clinic.[8][14] Another improvement suggested through literature includes decreasing test time from 100 minutes after ingestion of lactulose to 60 and 80 minutes after ingestion to prevent false positives.[18] A study on SIBO among children living in developing countries also discusses the lack of data on efficiency of these test methods on children.[7]
Medical Management of SIBO
Unfortunately, the current management strategies for SIBO are mostly empirical.[3][19] Common management strategies include using antibiotics and probiotics.[14][19][20] Other strategies for management besides eliminating overgrowth include treating underlying conditions that caused overgrowth and addressing nutritional deficiencies potentially caused by SIBO.[2]
Research also proposes dietary changes to help relieve the functional gastrointestinal (GI) symptoms.[21] Reduce intake of FODMAPs (fermentable oligo-, di-, and mono-saccharides and polyols)—poorly absorbed carbohydrates can effectively reduce bloating and other functional gastrointestinal symptoms.[21][22] Although the effectiveness of this strategy—previously used only to treat IBS and other GI conditions—for treating SIBO-related symptoms is still unclear.[6] Other food sources of functional gastrointestinal symptoms including gluten and natural and added food chemicals such as amines and glutamates and the benefit of dietary strategies that reduce the intake of these chemicals are still being researched.[21]
Interactions Between SIBO and Other Systemic Conditions
Although the prevalence and role in the pathogenesis of other diseases remain uncertain, reviews and case studies still show potential connections between SIBO and other systemic conditions such as irritable bowel syndrome (IBS) or Ehlers-Danlos Syndrome (EDS).[5][6] Other conditions that are hypothesized to be associated with SIBO include cirrhosis, chronic pancreatitis, and celiac disease.[3][5][7]
SIBO and Ehlers-Danlos Syndrome (EDS)
Ehlers-Danlos Syndrome is a group of rare disorders caused by collagen synthesis defects.[23] Delayed gastric emptying, which is a risk factor for SIBO, is common among EDS patients.[3][24][25] Studies show that SIBO diagnosis is common among EDS patients.[24] Another study suggests that EDS might be correlated with the constipation-predominant type of SIBO instead of the diarrhea-predominant type.[26] Yet because EDS is quite rare among the general population, sample sizes are small for most research done on EDS patients, especially those involving other comorbidities, which limits the scope of research.[23][26]
SIBO and Irritable Bowel Syndrome (IBS)
The relationship between IBS and SIBO is even more complicated because they both affect the GI system, as the names suggest. IBS is a common disorder that affects the large intestines.[27][28] The symptoms of IBS are similar to those of SIBO, including abdominal pain, bloating, gas, and diarrhea and/or constipation.[5][28][29] A review published on The Lancet Gastroenterology & Hepatology suggests that evidence between the link of SIBO and IBS is weak contrary to popular belief.[30]
Conclusion
Since SIBO is a fairly common condition, there is a general overview of its nature, yet the diagnostic criteria and treatment are mostly based on empirical evidence instead of quantitative research.[3][19][20] But in the past few years, there has been more literature discussing and criticizing the previous approaches to diagnosing and treating SIBO and more research done on interactions between SIBO and other conditions.[6]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 “Small Intestinal Bacterial Overgrowth (SIBO).” Mayo Clinic, Mayo Foundation for Medical Education and Research, 6 Jan. 2022, https://www.mayoclinic.org/diseases-conditions/small-intestinal-bacterial-overgrowth/symptoms-causes/syc-20370168.
- ↑ 2.0 2.1 2.2 2.3 Sachdev, Amit H, and Mark Pimentel. “Gastrointestinal bacterial overgrowth: pathogenesis and clinical significance.” Therapeutic advances in chronic disease vol. 4,5 (2013): 223-31. doi:10.1177/2040622313496126
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 Bohm, Matthew, et al. “Diagnosis and Management of Small Intestinal Bacterial Overgrowth.” Nutrition in Clinical Practice, vol. 28, no. 3, 2013, pp. 289–299., https://doi.org/10.1177/0884533613485882
- ↑ 4.0 4.1 Lehrer, Jenifer K. “Small Bowel Bacterial Overgrowth: Medlineplus Medical Encyclopedia.” MedlinePlus, U.S. National Library of Medicine, 27 May 2020, https://medlineplus.gov/ency/article/000222.htm.
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 Rana, Satya Vati, and Aastha Malik. “Hydrogen Breath Tests in Gastrointestinal Diseases.” Indian Journal of Clinical Biochemistry, vol. 29, no. 4, 2014, pp. 398–405., https://doi.org/10.1007/s12291-014-0426-4
- ↑ 6.0 6.1 6.2 6.3 6.4 Adike, Abimbola, and John K. DiBaise. “Small Intestinal Bacterial Overgrowth.” Gastroenterology Clinics of North America, vol. 47, no. 1, 2018, pp. 193–208., https://doi.org/10.1016/j.gtc.2017.09.008.
- ↑ 7.00 7.01 7.02 7.03 7.04 7.05 7.06 7.07 7.08 7.09 7.10 Donowitz, Jeffrey R., and William A. Petri. “Pediatric Small Intestine Bacterial Overgrowth in Low-Income Countries.” Trends in Molecular Medicine, vol. 21, no. 1, 2015, pp. 6–15., https://doi.org/10.1016/j.molmed.2014.11.001
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 Saad, Richard J., and William D. Chey. “Breath Testing for Small Intestinal Bacterial Overgrowth: Maximizing Test Accuracy.” Clinical Gastroenterology and Hepatology, vol. 12, no. 12, 2014, pp. 1964–1972., https://doi.org/10.1016/j.cgh.2013.09.055
- ↑ “Coliform Bacteria in Drinking Water Supplies”, NY Department of Health, July 2017, https://www.health.ny.gov/environmental/water/drinking/coliform_bacteria.htm.
- ↑ 10.0 10.1 “Fecal Coliform Bacteria.” Blue Earth River Basin Fecal Coliform Bacteria TMDL, https://mrbdc.mnsu.edu/sites/mrbdc.mnsu.edu/files/public/major/gbe/gbe_tmdl/fecal.html.
- ↑ Li, Daoliang, and Shuangyin Liu. “Chapter 12 - Water Quality Monitoring in Aquaculture.” Water Quality Monitoring and Management: Basis, Technology and Case Studies, Academic Press, London, England, 2019, pp. 303–328, https://doi.org/10.1016/B978-0-12-811330-1.00012-0. Accessed 8 Dec. 2022.
- ↑ Mello, Carolina Santos. “Methane Production and Small Intestinal Bacterial Overgrowth in Children Living in a Slum.” World Journal of Gastroenterology, vol. 18, no. 41, 2012, p. 5932., https://doi.org/10.3748/wjg.v18.i41.5932.
- ↑ Lagos, Rosanna, et al. “Effect of Small Bowel Bacterial Overgrowth on the Immunogenicity of Single‐Dose Live Oral Cholera Vaccine CVD 103‐HGR.” The Journal of Infectious Diseases, vol. 180, no. 5, 1999, pp. 1709–1712., https://doi.org/10.1086/315051.
- ↑ 14.0 14.1 14.2 14.3 14.4 14.5 “Small Intestinal Bacterial Overgrowth (SIBO).” Mayo Clinic, Mayo Foundation for Medical Education and Research, 6 Jan. 2022, https://www.mayoclinic.org/diseases-conditions/small-intestinal-bacterial-overgrowth/diagnosis-treatment/drc-20370172.
- ↑ Losurdo, Giuseppe, et al. “Breath Tests for the Non-Invasive Diagnosis of Small Intestinal Bacterial Overgrowth: A Systematic Review with Meta-Analysis.” Journal of Neurogastroenterology and Motility, vol. 26, no. 1, 2020, pp. 16–28., https://doi.org/10.5056/jnm19113
- ↑ Bond, John H., and Michael D. Levitt. “Use of Pulmonary Hydrogen (H2) Measurements to Quantitate Carbohydrate Absorption.” Journal of Clinical Investigation, vol. 51, no. 5, 1972, pp. 1219–1225., https://doi.org/10.1172/jci106916.
- ↑ 17.0 17.1 Ruszkowski, Jakub, and Jacek M. Witkowski. “Lactulose: Patient- and Dose-Dependent Prebiotic Properties in Humans.” Anaerobe, vol. 59, 2019, pp. 100–106., https://doi.org/10.1016/j.anaerobe.2019.06.002
- ↑ Sunny, Joseph K., et al. “Interpreting the Lactulose Breath Test for the Diagnosis of Small Intestinal Bacterial Overgrowth.” The American Journal of the Medical Sciences, vol. 351, no. 3, 2016, pp. 229–232., https://doi.org/10.1016/j.amjms.2015.12.008.
- ↑ 19.0 19.1 19.2 Leonello, R., et al. “P.12.7 Outcome of Patients with Positive Breath Test for SIBO Six Months after Combined Treatment with Rifaximin and Probiotics.” Digestive and Liver Disease, vol. 48, 2016, https://doi.org/10.1016/s1590-8658(16)30289-4
- ↑ 20.0 20.1 Richard, Nicolas, et al. “The Effectiveness of Rotating versus Single Course Antibiotics for Small Intestinal Bacterial Overgrowth.” United European Gastroenterology Journal, vol. 9, no. 6, 2021, pp. 645–654., https://doi.org/10.1002/ueg2.12116
- ↑ 21.0 21.1 21.2 Gibson, Peter R, and Susan J Shepherd. “Food Choice as a Key Management Strategy for Functional Gastrointestinal Symptoms.” American Journal of Gastroenterology, vol. 107, no. 5, 2012, pp. 657–666., https://doi.org/10.1038/ajg.2012.49
- ↑ Biesiekierski, Jessica R., and Caroline J. Tuck. “Low Fodmap Diet beyond IBS: Evidence for Use in Other Conditions.” Current Opinion in Pharmacology, vol. 64, 2022, p. 102208., https://doi.org/10.1016/j.coph.2022.102208
- ↑ 23.0 23.1 “Ehlers-Danlos Syndrome: Medlineplus Genetics.” MedlinePlus, U.S. National Library of Medicine, https://medlineplus.gov/genetics/condition/ehlers-danlos-syndrome/#frequency.
- ↑ 24.0 24.1 Xiong, Tingting, et al. “1182 Small Intestinal Bacterial Overgrowth (SIBO) Is Common in Patients with Ehlers-Danlos Syndrome (EDS).” American Journal of Gastroenterology, vol. 114, no. 1, 2019, https://doi.org/10.14309/01.ajg.0000594256.00026.1d
- ↑ Nelson, A. D., et al. “Ehlers Danlos Syndrome and Gastrointestinal Manifestations: A 20-Year Experience at Mayo Clinic.” Neurogastroenterology & Motility, vol. 27, no. 11, 2015, pp. 1657–1666., https://doi.org/10.1111/nmo.12665
- ↑ 26.0 26.1 Zhou, Wendy, et al. S0476 High Prevalence of Methane Predominant Small Bowel Bacterial Overgrowth and Constipation in Patients With Hypermobile Ehlers-Danlos Syndrome. The American Journal of Gastroenterology: October 2020 - Volume 115 - Issue - p S238 doi: 10.14309/01.ajg.0000703952.17443.b0
- ↑ “Irritable Bowel Syndrome | IBS.” MedlinePlus, U.S. National Library of Medicine, 2018, https://medlineplus.gov/irritablebowelsyndrome.html.
- ↑ 28.0 28.1 “Irritable Bowel Syndrome.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 2 Nov. 2022, https://www.mayoclinic.org/diseases-conditions/irritable-bowel-syndrome/symptoms-causes/syc-20360016
- ↑ “Symptoms & Causes of Irritable Bowel Syndrome.” National Institute of Diabetes and Digestive and Kidney Diseases, U.S. Department of Health and Human Services, 2017, https://www.niddk.nih.gov/health-information/digestive-diseases/irritable-bowel-syndrome/symptoms-causes.
- ↑ Aziz, Imran, and Magnus Simrén. “The Overlap between Irritable Bowel Syndrome and Organic Gastrointestinal Diseases.” The Lancet Gastroenterology & Hepatology, vol. 6, no. 2, 2021, pp. 139–148., https://doi.org/10.1016/s2468-1253(20)30212-0
Edited by Yufan Lu, student of Joan Slonczewski for BIOL 116 Information in Living Systems, 2022, Kenyon College.
