Chlamydia trachomatis: Difference between revisions
| Line 53: | Line 53: | ||
Does this organism produce any useful compounds or enzymes? What are they and how are they used? | Does this organism produce any useful compounds or enzymes? What are they and how are they used? | ||
''Chlamydia trachomatis'' | Using the major outer membrane protein (MOMP) of ''Chlamydia trachomatis,'' antibody-based diagnostics as well as recombinant vaccines | ||
antibody-based diagnostics as well as recombinant vaccines | |||
==Current Research== | ==Current Research== | ||
Revision as of 06:28, 5 June 2007
A Microbial Biorealm page on the genus Chlamydia trachomatis
.
Classification
Higher order taxa
Bacteria; Chlamydiae/Verrucomicrobia group; Chlamydiae; Chlamydiae (class); Chlamydiales; Chlamydiaceae; Chlamydia
Genus
Chlamydia
Description and significance
Describe the appearance, habitat, etc. of the organism, and why it is important enough to have its genome sequenced. Describe how and where it was isolated.
C. trachomatis is an obligate, aerobic, intracellular parasite of eukaryotic cells. It is a Gram-negative bacteria and has a coccoid or rod shape. It has a cytoplasmic membrane and outer membrane similar to Gram-negative bacteria (thus, it being classified as Gram-negative) but, it lacks a peptidoglycan cell wall. C. trachomatis require growing cells in order to remain viable since it cannot synthesize its own ATP. Without a host organism, C. trachomatis cannot survive on its own [3].
C. trachomatis is the leading cause of sexually transmitted disease worldwide--in the United States, alone, over 4 million cases are diagnosed each year. It is also the leading cause of preventable blindness (caused by a chlamydia infection called trachoma)in the world [5]. C. trachomatis is also one of the major causes of pelvic inflammatory disease (PID) and infertility in women [3].
It is important to understand and sequence the genome of C. trachomatis because it would help us better understand its functions as a pathogen--the properties that allow it to live within its human host and its virulence and biological capabilities as a pathogen. Thus, an effort has been made to sequence most of the C. trachomatis genome [2].
Genome structure
Describe the size and content of the genome. How many chromosomes? Circular or linear? Other interesting features? What is known about its sequence? Does it have any plasmids? Are they important to the organism's lifestyle?
Chlamydia trachomatis has a genome that consists of 1,042,519 nucleotide base pairs and has approximately 894 likely protein coding sequences. [2] C. trachomatis strains have an extrachromosomal plasmid, which was sequenced to be a 7493-base pair plasmid. Because there is less than 1% nucleotide sequnce variation, ll plasmids from human C. trachomatis isolates are considered to be very similar. All the isolates "are about 7,500 nucleotides long and has eight open reading frames computer-predicted to code for proteins of more than 100 amino acids, with short non-coding sequences between some of them." [1]
Interestingly, in their nucleotide sequence, chlamydial plasmids are more closely related than is the corresponding chromosomal DNA. The plasmid of C. trachomatis is a favored target for DNA-based diagnosis of C. trachomatis because there are approximately 7-10 copies of the plasmid present per chlamydial particle. Its sequence is highly conserved among different isolates of C. trachomatis. Some C. trachomatis strains lack these plasmids, and the consequences aid in detection of the C. trachomatis strain. Plaque purified C. trachomatis that do not contain the plasmids have unusual inclusion morphology, has no glycogen, and shows no alteration in antibiotic sensitivity . However, the fact that such strains exist shows that the plasmid is not essential for C. trachomatis survival [1].
Cell structure and metabolism
Describe any interesting features and/or cell structures; how it gains energy; what important molecules it produces.
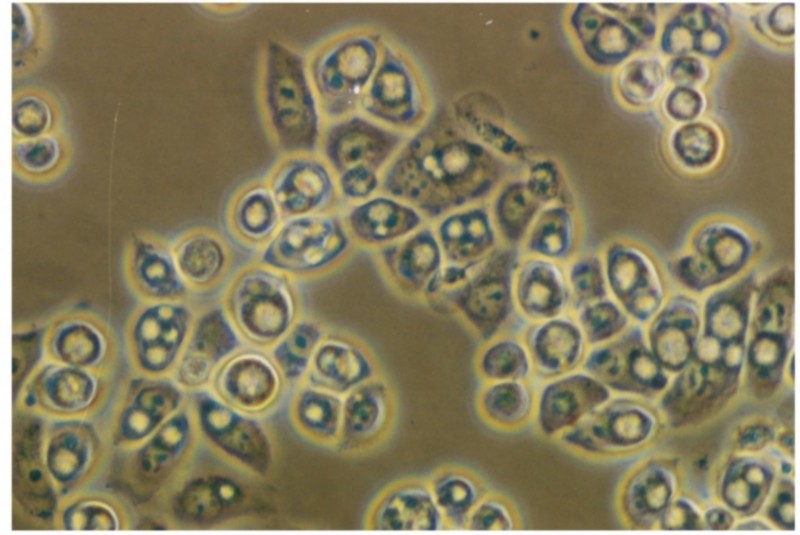
The life cycle of Chlamydia trachomatis consists of two stages: elementary body and reticulate body. The elementary body is the dispersal form, which is analogous to a spore. The dispersal form is about 0.3 um in diameter and induces its own endocytosis upon exposure to target cells. It is this form that prevents phagolysosomal fusion, which then allows for intracellular survival of the bacteria. Once inside the endosome, the elementary body germinates into the reticulate body as a result of the glycogen that is produced. The reticulate body divides through binary fission at approximately 2-3 hours per generation. The cell body has an incubation period of 7-21 days in the host. It contains no cell wall and is detected as an inclusion in the cell. After division, the reticulate body transforms back to the elementary form and is released by the cell by exocytosis. One phagolysosome usually produces 100-1000 elementary bodies [2].
For metabolism, Chlamydia trachomatis has a glycolytic pathway and a linked tricarboxylic acid cycle. Glycogen synthesis and use of glucose derivatives plays a supporting role in chlamydial metabolism. The presence of metabloic precursors and products, such as pyruvate, succinate, glycerol-3-phosphate and NADH dehydrogenases, NADH-ubiquinone oxidoreductase and cytochrome oxidase indicate that Chlamydia trachomatis uses a form of electron transport in order to produce energy [2].
Ecology
Describe any interactions with other organisms (included eukaryotes), contributions to the environment, effect on environment, etc.
Chlamydia trachomatis is a pathogenic bacteria. It cannot survive outside of a eukaryotic host. In fact, humans are the only known natural host for C. trachomatis. The bacterium is transmitted by sexual contact with an infected individual.
Pathology
How does this organism cause disease? Human, animal, plant hosts? Virulence factors, as well as patient symptoms.
Chlamydiae replicate intracellularly in what is called an inclusion--a membrane bound structure. This inclusion, is able to avoid lysosomal fusion and degradation. Thus, the metabolically inactive elementary body form of chlamydia is able to become the reticulate body. The multiplying reticulate bodies then become elementary bodies again and burst out of the host cell to continue the infection cycle. Since Chlamydiae are obligate intracellular parasites, they cannot be cultured outside of host cells, leading to many difficulties in research [3]. (Also, see Cell Structure Section)
Chlamydia is transmitted through infected secretions only. It infects mainly mucosal membranes, such as the cervix, rectum, urethra, throat, and conjunctiva. It is primarily spread via sexual contact and manifests as the sexually transmitted disease. The bacterium is not easily spread among women, so the STD is mainly transmitted by heterosexual or male homosexual contact. However, infected secretions from the genitals to the hands and eventually to the eyes can cause trachoma [5].
Application to Biotechnology
Does this organism produce any useful compounds or enzymes? What are they and how are they used?
Using the major outer membrane protein (MOMP) of Chlamydia trachomatis, antibody-based diagnostics as well as recombinant vaccines
Current Research
Enter summaries of the most recent research here--at least three required
References
[3]Byrne, Gerald I. 2003. "Chlamydia uncloaked." PNSA 100:14. 2003
Edited by Christina Bach, student of Rachel Larsen and Kit Pogliano
