Plasmodium falciparum in Cambodia: Difference between revisions
| Line 3: | Line 3: | ||
==Malaria: The Disease== | ==Malaria: The Disease== | ||
Malaria is fatal disease that | Malaria is fatal disease that has infected about 515 million people worldwide and kills nearly a million people annually (1). It is widespread mostly in tropical and subtropical countries where conditions allow the Anopheles mosquitoes to thrive. | ||
Very often malaria is found in poor | Very often malaria is found in economically poor countries, where people are unable to afford preventive vaccinations or any medical treatments. Throughout the years it has been shown that poverty and malaria are inter-linked, one affects the other. People in poverty, individual or family, may not be able to pay for their transportation, consultation with doctors and, of course, for their treatment (such as anti-malarial drug) fees at health facilities (21). | ||
There are four types of human malaria | There are four types of human malaria: ''Plasmodium(P) falciparum'', ''Plasmodium vivax'', ''Plasmodium malariae'' and ''Plasmodium oval''. Among these four, ''P. falciparum'' and ''P. vivax'' are the most common ones, with ''P. falciparum'' causing the most number of deaths. | ||
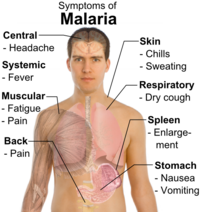
[[Image:Symptoms_of_Malaria.png|thumb|200px|left|Symptoms of Malaria|]] | [[Image:Symptoms_of_Malaria.png|thumb|200px|left|Symptoms of Malaria|]] | ||
Malaria | Malaria is a disease that includes symptoms such as fever, abdominal pain, chills, headaches, nausea, diarrhea and vomiting, which can appear after couple of days or weeks after the infection. Also, very often malaria can lead to severe anemia, seizures, kidney failure, confusion and death if not treated on time (5). | ||
An interesting study shows that in Southeast Asia malaria was first transmitted to humans by chimpanzees and not by mosquitoes (20). The parasite in monkeys is ''Plasmodium Knowlesi'' , not ''Plasmodium falciparum'', and is found in monkeys only. There have also been found some similarities between the human and monkey parasites which suggested that those two strains might have evolved from a common ancestor million of years ago. As a result of these findings, researchers are now wondering if ''P. Knowlesi'' is the fifth human malaria. | An interesting study shows that in Southeast Asia malaria was first transmitted to humans by chimpanzees and not by mosquitoes (20). The parasite in monkeys is ''Plasmodium Knowlesi'' , not ''Plasmodium falciparum'', and is found in monkeys only. There have also been found some similarities between the human and monkey parasites which suggested that those two strains might have evolved from a common ancestor million of years ago. As a result of these findings, researchers are now wondering if ''P. Knowlesi'' is the fifth human malaria. | ||
Revision as of 16:09, 28 August 2009
Malaria: The Disease
Malaria is fatal disease that has infected about 515 million people worldwide and kills nearly a million people annually (1). It is widespread mostly in tropical and subtropical countries where conditions allow the Anopheles mosquitoes to thrive.
Very often malaria is found in economically poor countries, where people are unable to afford preventive vaccinations or any medical treatments. Throughout the years it has been shown that poverty and malaria are inter-linked, one affects the other. People in poverty, individual or family, may not be able to pay for their transportation, consultation with doctors and, of course, for their treatment (such as anti-malarial drug) fees at health facilities (21).
There are four types of human malaria: Plasmodium(P) falciparum, Plasmodium vivax, Plasmodium malariae and Plasmodium oval. Among these four, P. falciparum and P. vivax are the most common ones, with P. falciparum causing the most number of deaths.
Malaria is a disease that includes symptoms such as fever, abdominal pain, chills, headaches, nausea, diarrhea and vomiting, which can appear after couple of days or weeks after the infection. Also, very often malaria can lead to severe anemia, seizures, kidney failure, confusion and death if not treated on time (5).
An interesting study shows that in Southeast Asia malaria was first transmitted to humans by chimpanzees and not by mosquitoes (20). The parasite in monkeys is Plasmodium Knowlesi , not Plasmodium falciparum, and is found in monkeys only. There have also been found some similarities between the human and monkey parasites which suggested that those two strains might have evolved from a common ancestor million of years ago. As a result of these findings, researchers are now wondering if P. Knowlesi is the fifth human malaria.
As a result of its devastating effects on the human population, many organizations, such as the Gates Foundation, and countries have banded together to find preventative measures and treatments for this global epidemic.
Description of Malaria
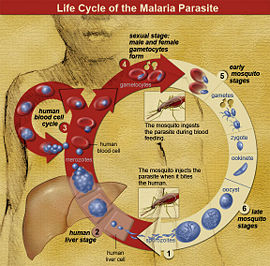
In Cambodia, the specific species (Anopheles dirus, A. minimus, and A. sundaicus) transmit the malaria-causing parasites (Plasmodium falciparum and P. vivax) to the host during feeding with the bite, transmitting the parasite through their saliva (2).
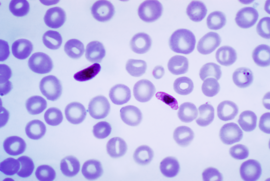
The parasite initially enters the liver, where it multiplies and then infects the red blood cells. Here parasites still continue to multiply until eventually the red blood cells burst and the parasite appears in the plasma. Now, the parasites are free in the plasma and will infect any mosquito that bites and feeds on the host’s blood. Once the parasites enter the mosquito, they are also found in its saliva and are ready to be transferred to another individual and repeats the cycle after biting another host.
Malaria can also be transmitted via blood transfusion, shared use of needles or syringes that are contaminated with blood, or organ transplant since malaria is in red blood ceels of infected individuals.
The number of infected people observed in Cambodia each year exceeds more than a million out of which about 10-15% die (5). Victims of malaria are mostly children, infants, and pregnant women because of their weaker immune system (3). Forest inhabitants, border workers and migrants are also in high risk in getting the disease because of their increased exposure to mosquito vectors.
Studies have shown that global warming and climate changes may also lead to malaria’s rise (4). Increasing temperatures, humidity, deforestation,and rains are all factors that may favor to mosquito spread to the areas where previously they did not exist which, in turn will lead to an increased incidence of malaria.
Description of the Plasmodium falciparum
Plasmodium falciparum is a species of the genus Plasmodium, which is of the Eukaryote domain and Plasmodiidae family. Plasmodium are much more complex than simple bacteria because of a “genetic complexity five times greater” (1). Their complex genome allows them more flexibility in various environments where simple bacteria can’t survive. Aside from having a complex genome, Plasmodium possesses various invasive stages for targeting specific host. Plasmodium falciparum are are the most dangerous and prominent due to being the cause of the majority of malaria cases and the cause of most severe malaria conditions.
Infection
Plasmodium possesses various forms, the most prominent being sporozoite, merozoite, and ookinete. These various forms of a plasmodium are directly tied to the cycle of infection. Sporozoite enters the human body via the saliva of mosquitoes during a blood meal. Sporozoites infect the hepatocytes (liver cell) within 30 minutes. From the hepatocyte, the parasite reproduces asexually into merozoites until they are released from the liver and enter the bloodstream. Merozoites then invade the erythrocytes (red blood cells) within 10 minutes. The merozoites continue proliferation in infected erythrocytes and also infect other uninfected erythrozytes. In an erythrocyte, merozoite can also differentiate to become gametocyte where they can be carried off by female mosquitoes after a blood meal. The gametocytes travel to the mosquitoes’ guts where they differentiate into male and female cells for fertilization. A zygote or ookinete is ultimately formed. The ookinete develops into sporozoites and venture into the saliva of the mosquitoes where they can further infect other human (7).
This cycle ties human and mosquitoes directly in the transmission and infection of malaria. In this relation, anopheline mosquitoes act as a vector and aid in spreading the infection. However, not all mosquitoes can be vectors. Only 68 out of 460 Anopheles can be vectors. Moreover, only female mosquitoes can take up gametocytes and transmit sporozoites as they are the only mosquitoes that bite.
Reasons for Symptoms
Many symptoms of malaria may be caused by the effects of merozoites interfering with the red blood cells' ability to carry oxygen. In infected erythrocytes, the cells are found to be deformed and stiffen due to merozoites making cellular structure and membrane changes. These changes are made to aid in the transport of parasitic nutrients and to satisfy parasitic needs. Hemoglobins also function as nutrients for the merozoites. Infected red blood cells are also more prone to cytoadhenerece known as auto-agglutination, rosetting, and sequestration. Rosetting is the adherence of infected red blood cells to uninfected red blood cells. Rosetting may be one of the mechanism for infection of other eyrthocytes by infected eyrthocytes. Auto-agglutination is adherence to other infected erythrocytes. Sequestration is the adherence of infected blood cells to the endothelial layer. The site of sequestration also prompts more infected cells to attach resulting in a buildup of infected cells. Sequestration hinders oxygen delivery to organs or tissue and may result coma symptom in cases of severe malaria. The combined effect of rosetting, sequestration, auto-agglutination, and consumption of hemoglobin by merozoites play a strong role in the hindrance of oxygen delivery. This may be the cause of flu-like symptoms of malaria. Other causes of symptoms are due to the release of malaria toxins. Malaria toxins can both damage tissue and over-stimulate cytokines. Cytokine is generally used to fight against microorganisms but overproduction result in inflammatory response and is more harmful than helpful. This may be the cause of fever in malaria.(8)
Prevention: Mosquito Bite
Prevention can begin before the mosquito even bites. To deter and prevent mosquito bites wear long sleeves, pants, hats, and shoes rather than exposing skin with sandals, shorts and short sleeves. For areas that are exposed apply insect repellents containing DEET we especially in areas where travelers may encounter potentially lethal mosquito-vector diseases such as malaria and yellow fever. DEET effectiveness over a period of time is dependent on the concentration; higher concentrations means longer repellent protection. 100% DEET=9.5 hours, 30% for 6.5 hours, 15% for 5 hours, and 10% for 3 hours. Although, it looks like using a higher amount of DEET would always be the best case, high concentrations of DEET carry greater toxicity without much benefit. Neurological toxicity may occur in humans as a result of high amounts of DEET exposure. The effectiveness of the repellent is also affected by temperatures, humidity, sweating, and exposure to water, so caution and awareness are key to preventing bug bites.
Permethrin is another insecticide that can protect against mosquito bites. This compound can be applied to clothing, shoes, tents, and bed nets, with research showing that they were more effective against mosquito bites than untreated articles. Contrary to claims, repellent-impregnated wristbands are ineffective against mosquito bites. (11)
Anti-malaria drugs can also be combined with bite prevention to lower the risk of infection. This is known as chemoprophylaxis. The goal of this method is to prevent progression of the disease in the chance of transmittance of sporozoites from mosquito bites. However, chemoprophylaxis should only be limited to travelers staying short time due to cost of continuous anti-malaria drug usage. Usage of Chloroquine and pyrimethamine with sulfadoxine is advised against due to plasmodium falciparum increasing resistance to these drugs. Alternatives such as mefloquine, doxycycline, and atovaquone with proguanil should be used instead to minimize risk.(7)
Treatment
Increasing resistance of Plasmodium falciparum makes treatments, especially in Cambodia and other Southeast Asian countries, difficult. Drugs such as Chloroquine and Artemisinin based are inadvisable due to increasing resistance of the parasite worldwide. Artemisinin based drug such as Artesunate, prior to resistance, was the more recommended treatment due to fewer side effects and effectiveness. Outside of the high resistance area, Artemisinin-based treatment may still be used for treating falciparum cases malaria. Chloroquine is still used for non-falciparum malaria but resistance often occurs and Chloroquine is often accompanied by Quinine. Treatments for falciparum malaria now would be in some form of Quinine for condition of mild and severe malaria in location of high resistance. However, Quinine has many side effects and severe cases of malaria would require much stronger dosage or concentration. Quinine is also not suitable for children and pregnant women though it can still be administered with appropriate dosage.(27,28)
A potential new vaccine in development may be a permanent solution to malaria cased by falciparum. This new vaccine is Merozoite Surface Protein-3, or MSP3. MSP3 stimulates IgG, which is an antigen of monocyte and is crucial in the recognition and killing of plasmodium falciparum parasite. It is currently in clinical trial and has shown to be safe and satisfying in preventing malaria when tested in children of age 12 – 24 months.(29)
Why is this disease a problem in Cambodia?
Cambodia is one of a few countries in Southeast Asia that have been struck by the malaria epidemic. It is home to the world’s most drug-resistant strain of malaria (P. falciparum) and there are fears that more resistance to antimalarial drugs are developing. Plasmodium falciparum, one of the most common and deadliest strands of malaria has been a major problem in Cambodia due to numerous factors.
Geography
Cambodia has an area of 69,898 square miles and about 60% this is comprised of forests and plains (5). This geography coupled with Monsoon-dominated weather makes Cambodia’s climate very moist. With its shady and wooded landscape, it makes Cambodia the perfect home for mosquitoes to survive and breed. Most of the population in Cambodia lives in these dense and moist forests where mosquitoes can transmit malaria to humans. Forest regions bordering Thailand and rubber plantations found in the East and Northwest are where malaria is likely to be found. About 15% of Cambodians are at elevated risks of malaria infection; of these forest inhabitants, migrant and border workers, pregnant women, infants, and children are the most susceptible to the disease (5).
The Overwhelmed and Inadequate Health Care System
Poor health infrastructure and poor communication systems are also major contributing factors to the malaria epidemic in Cambodia. In high transmission areas such as forests, health facilities like hospitals are lacking, and transportation systems are insufficient or nonexistent. Poor road conditions, lack of suitable vehicles and a lack of telephone facilities lead to treatment delays for the infected in remote areas. Many of the affected areas are often inaccessible (18).
The inadequate health care system adds to the problem of malaria in Cambodia. There are often shortages of diagnostic kits and appropriate drugs, as well as a lack of qualified private practitioners. Many unqualified doctors and pharmacies do not follow the national treatment guidelines. There are also large numbers of fake drugs available in the market due to lack of strict regulation and quality control practices. The counterfeits may contain no active ingredients or contain ingredients different from the package label. In 1999, fake antimalarial drugs were responsible for at least 30 deaths in Cambodia (19).
Malaria's Economic Toll
Furthermore, the malaria epidemic greatly hinders Cambodia ability for economic improvements because it disables the work force, lowers educational achievements, slowed tourism and business investments. Due to the low economic growth, it causes a continued cycle of Cambodia’s inability to improve its living standards and therefore restricting its resources to prevent further outspread of malaria (16).
What is being done to address this problem
Government Policies
In the year 2000, Cambodia was the first country to switch its anti-malarial drug policy to an artesunate combination therapy (ACT), in which they recommended a first-line treatment consisting of a combination of artesunate and mefloquine (A+M). ACT is important because artemisinin monotherapy (using artemisinin alone) will very likely cause a widespread artemisinin-resistant Plasmodium falciparum, which would be devastating. Other drugs, like chloroquine and pyrimethamine-sulfadoxine, usually used to treat malaria, can no longer be used because Plasmodium falciparum is multi-drug resistant and render them ineffective as treatment. However, recently, Artemisnin-resistant P. Falciparum has been emerging in parts of Western Cambodia, and since Artemisnin is the first line treatment, this is becoming a large problem. (9)
Included with this policy were blister packaging of the A+M and separating them into three distinct age groups, marketing of the A+M product as "Malarine®" at a subsidized cost, public campaigning to educate the general public on fake anti-malarials and their negative effects, and advocating the usage of rapid diagnostic tests (RDT) also known as the dipstick test which works by testing the patients blood smear for the presence of parasites transmitted by malaria, most prominently P. falciparum (14).
Insecticide Treated Mosquito Nets (ITN)
The government has also been distributing insecticide treated mosquito nets (ITN) which are useful preventative measures by creating a physical barrier between the parasite carrying mosquitoes and the potential victim, and is especially helpful, seeing as mosquitoes have a tendency to attack at night. These nets help by repelling, disabling, and/ or killing the mosquitoes that come in contact with the net (10). In 2007, 557,000 mosquito nets were distributed, and one million nets are going to be distributed in 2008. However, only 54.2% of Cambodians have received the mosquito nets; more volunteers are needed to distribute them (13).
Village Malaria Workers (VMW) and Malaria Outreach Teams (MOT)
A fairly efficient method currently used to ensure that the individuals who need the drug treatments receive and correctly use them are Village Malaria Workers (VMW) and Malaria Outreach Teams (MOT). The VMW are funded and run by “National Malaria Control Programme” and receive additional funding from the “Global Fund for AIDS, Tuberculosis and Malaria”, and the MOT is funded by "Médecins Sans Frontières" (MSF) (15). These groups greatly increase treatment accessibility by diffusing into areas including rural and difficult to reach endemic areas. They perform an effective survey of the local population with RDTs which are relatively inexpensive, mobile, and quick in relation to past tests done in laboratories. They provide high grade A+M (artemisinin-mefloquine drugs) virtually free to those infected and check on their progress and whether they have completed the full course of anti-malarials(14). And those who believe they have become infected then have convenient access to diagnosis and treatment.
What else could be done to address this problem
VWM and MOT Funding
Since the VMW and MOT are widely distributed and run in difficult to reach, endemic areas, there are large monetary costs associated with the start up and upkeep of the groups. More investment and the increase in the amount of willing and dedicated volunteers are needed to extenuate the reach of these groups, along with increased global awareness. With these, the positive effects of these groups can be even greater and more widespread.
Further Publicity Campaigning and Malaria Education
A method necessary for prevention includes an awareness campaign in which communities are educated on 1) identifying symptoms of malaria and where to go and what to expect during treatment as well as 2) how to identify genuine and counterfeit blister packaging of A+M. They must also be 3) provided with insecticide treated nets (ITN), to reduce mosquito contact, at no or very low costs to encourage their use among the large numbers of people who live in poverty. The VMW and MOT can then go around and check to see whether people are utilizing the nets. Campaigning and ITNs will be costly and a raised global awareness along with additional funding are imperative for the publicity campaign’s success.
Research for an Effective Artemisinin Substitute
Currently ACTs are more effective as treatment than other treatments because they decrease malaria transmission by preventing the development of P. falciparum gametocytes while at the same time, using a combination of drugs with distinct targets, this significantly decreases the chance of a mutation with resistance, because resistance to both drugs would be necessary (16). But at the same time, more research must be allotted towards finding other suitable drugs for treatment in the event that there is a widespread artemisinin resistance, which is now becoming a large possibility.
Parasites are rapidly becoming resistant to those drugs. For example, patients could have been clear of parasites in 2 days, however, now it takes about 3.5 days to kill (9). The World Health Organization (WHO) suggests several ways to reduce the artemisinin resistance: to detect all malaria cases in target areas and to kill all artemisinin-tolerant parasites, and limit the emergence of a widespread resistance by reducing exposure of the parasites to artemisinin. (26)
Prohibiting the Sales and Distribution of Artemisinin Mono-therapies and Sub-standard Drugs
Contributing to this problem is the tendency for individuals living in rural endemic areas to seek treatment from informal health providers who would often times sell them artemisinin monotherapies, sub-standard artemisinin-mefloquine (A+M), or even fake drugs. Along with these low-grade drugs, individuals were not checked to see if they had finished the full course of the drug treatment (16). In many other instances, individuals were even given anti-malarials with the sign of a mere fever without any biological confirmation of malaria itself (16). These are large contributing factors to the drug resistances that Plasmodium falciparum has developed towards other previously effective anti-malarials. Blister packages are now used to ensure the user of high-grade A+M because it would be evident if the drug and packaging were tampered with and can ensure the user that the drug is not sub-standard nor fake. This system packages drugs recognized internationally by “Good Manufacturing Practice” (GMP) and are run by the “National Malaria Centre” (CNM) and supported by the “World Health Organization” (WHO) (15). Additionally, a government policy banning the use of artemisnin mono-treatments and the unnecessary prescription of anti-malarials without biological confirmation of the disease needs to be enacted, in order to reduce the risk of widespread artemisinin-resistant P. Falciparum. Artemisinin mono-treatments greatly increase the risk of creating an artemisinin-resistant P. Falciparum. So exposure to the drug should be limited, by only giving the drug to those who need it, and always giving artemisinin in combination with another drug.
Counterfeit Detecting and Decreasing Counterfeit Distribution
But these blister packages have been victim to counterfeiting, causing a new array of problems. Unfortunately, counterfeit blister packaging containing less than sufficient amounts of artemisinin are often being sold by informal health providers. This is a problem because the drug is not capable of wiping out P. falciparum, thus enabling the possibility of an artemisinin-resistant P. falciparum mutant, which would, again, be catastrophic (14). Genuine A+M blister packaging contains a specific hologram and other key features that consumers should learn to identify, which needs to be taught because the differences between counterfeit and authentic blister packaging are very subtle. But fake blister packages may contain holograms as well, and special attention to details is necessary to identify a counterfeit. As counterfeit awareness has been increasing, sometimes, the counterfeits now being produced are so well duplicated that the average consumers may not even be able to differentiate between the real and the fakes. Chemical testing, i.e. LC-MS and Raman spectroscopy, may even be necessary in order to determine its authenticity (17). Luckily, receiving free genuine A+M from VMW's and MOT's can assist in alleviating widespread distribution of counterfeits.
Summary
Overall, malaria is a life-threatening disease which is caused by parasites that are transmitted to people via the bites of infected mosquitoes. Malaria is spread almost everywhere, and more specifically at the low-income countries. Even though it is wide spread and fatal, it can be prevented and cured through various anti-malarial drugs and vaccines available. Patients infected with malaria should get an early treatment in order to prevent complications and decrease the number of deaths each year. Cambodia is a perfect place for mosquitoes to live because 60% of the country is comprised of forests and plains. Also, moist climate makes it easier for mosquitoes to survive and breed. The government of Cambodia distributed Insecticide Treated Mosquito Nets (ITN); and this reduced the number of malarial infections and deaths have decreased in recent years. For every 100,000 people, the rate has been reduced from 2.81 percent to 1.68 percent. Other efforts of volunteers, such as Village Malaria Workers (VMW) and Malaria Outreach Teams (MOT) prevent and stop the spread of malaria by providing drug treatments and improving local communications in rural areas. However, there is a growing concern about the disease that parasites become resistant to anti-malarial drugs. The World Health Organization urges people to be aware of the disease before getting infected. It also tells to eradicate malaria in target areas and minimize the exposure of the parasites to Artemisinin to limit the resistance. We can expect a bright future in Cambodia because there are on-going researches for an effective Artemisinin substitute and funding from organization like VMW and MOT.
References
5. "Fewer Malaria Cases in Cambodia.” 2009. Population Reference Bureau. Dec. 2002. Web. 13 Aug. 2009
11. “Bites from mosquitoes, ticks, and other insects”. Mdtravelhealth. Web. 23 Aug. 2009.
12. Traveler’s Health, Centers for Disease Control and Prevention. Web. 21 Aug. 2009.
13. “Malaria”. National Institute of Allergy and Infectious Diseases. Web. 23 Aug. 2009.
20. "Scientists Find Malaria Jumping from Chimps to Humans.” AFP. 3 Aug. 2009. Web. 21 Aug. 2009.
23. “Mosquitoes” Centers of Disease Control and Prevention. Web. 21 Aug. 2009.
24. “Malaria self-test module”. Royal Perth Hospital. Web. 21 Aug. 2009.
25. Public Health Image Library, Centers of Disease Control and Prevention. Web. 21 Aug. 2009.
26. Chinnock , Paul . "Containing artemisinin resistance ". TropIKA. 2 Mar 2009. Web. 24 Aug. 2009.
Edited by [Betsy Chiem, Lusine Minasyan, Chuong Do, Katherine Leu, Albert Luong and Ben Cho], students of Rachel Larsen