Cyclospora cayetanensis: Difference between revisions
No edit summary |
|||
| (52 intermediate revisions by one other user not shown) | |||
| Line 1: | Line 1: | ||
{{Conway}} | |||
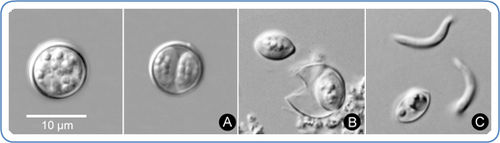
{{ | [[Image:Sporulation_and_Rupturing_of_Cyclospora_oocyst.jpg|thumb|500px|right|Sporulation and Rupturing of <i> Cyclospora cayetanensis </i> oocyst [From:http://www.cdc.gov/parasites/cyclosporiasis/]]] | ||
[[Image: | |||
==Etiology/Bacteriology== | ==Etiology/Bacteriology== | ||
===Taxonomy=== | ===Taxonomy=== | ||
| Line 13: | Line 12: | ||
{| | {| | ||
| height="10" bgcolor="#FFDF95" | | | height="10" bgcolor="#FFDF95" | | ||
'''NCBI: [http://www.ncbi.nlm.nih.gov/Taxonomy/Browser/wwwtax.cgi] </font>''' | '''NCBI: [http://www.ncbi.nlm.nih.gov/Taxonomy/Browser/wwwtax.cgi] <font size="2"></font>''' | ||
|} | |} | ||
===Description=== | ===Description=== | ||
<i> Cyclospora cayetanensis </i> is a parasitic pathogen that causes Cyclosporiasis, which is characterized by prolonged watery diarrhea and intestinal distress, also including abdominal pain among many other symptoms. [[#References|[3]]] <i> Cyclospora cayetanensis </i> is an obligate intracellular, coccidian protozoan pathogen to humans, classified within the phylum Apicomplexa, and is known to for several food-borne outbreaks in the United States. [[#References|[1]]] The oocyst of <i> Cyclospora cayetanensis </i> is a spherical shape, and can range from 8 to 10 μm, and after sporulation each oocyst contains four sporozoites ready for invasion of the host. [[#References|[8]]]<i> Cyclospora cayetanensis </i> causes infection by the ingestion of contaminated foods or liquids by a sporulated oocyst that is in its infectious stage; unsporulated oocysts are not infectious to hosts and must first complete sporulation outside the host to become infectious. [[#References|[1]]] All organisms under the Apicompleza phylum have a complex life cycle involving an invasive stage, using specialized organelles for penetration and invasion of host cell. [[#References|[4]]] This pathogen is known to cause traveller’s diarrhea in infected hosts, and several water-borne and food-borne outbreaks of this microorganism have been reported in the past decades. [[#References|[1]]] The infection is usually self-limiting, however for more persistent cases of infection, drug treatment is available. Diagnosis for this organism can be difficult, but improved diagnostic methods such as autofluorescence, has assisted in easier detection of <i> C. cayetanensis </i>oocysts in stool samples. Even though there are several species of <i> Cyclospora </i> that also develop in the gastrointestinal tract of vertebrates, only <i> Cyclospora cayetanensis </i> had been observed to cause illness in humans. [[#References|[3]]] | |||
==Pathogenesis== | ==Pathogenesis== | ||
===Transmission=== | ===Transmission=== | ||
<i> Cyclospora cayetanensis </i> is spread via the fecal-oral route, meaning that the host must ingest something, food or water for example, that had been contaminated with feces that contain infectious oocysts; to be infectious the oocyst has to be sporulated. An unsporulated oocyst takes from days to weeks outside a host cell after being excreted in a fecal matter of an infected host to become a sporulated oocyst, now capable of infecting another host. | <i> Cyclospora cayetanensis </i> is spread via the fecal-oral route, meaning that the host must ingest something, food or water for example, that had been contaminated with feces that contain infectious oocysts; to be infectious the oocyst has to be sporulated. An unsporulated oocyst takes from days to weeks outside a host cell after being excreted in a fecal matter of an infected host to become a sporulated oocyst, now capable of infecting another host. [[#References|[2]]] Imported fresh produce from tropical regions, such as raspberries, basil and lettuce have caused outbreaks of cyclosporiasis from contamination from feces. [[#References|[3]]] Essentially, any food that has been contaminated with fecal matter containing infectious, sporulated oocysts have the potential to cause infection of <i> Cyclospora cayetanensis </i>. To date, there has been no documented transmission from human-to-human, likely due to the amount of time outside a host the oocyst has be to transform into a sporulated oocyst capable of infection. [[#References|[5]]] It is thought that the topology of the surface of certain kinds of fruits and vegetables help contribute to adherence and of the <i> Cyclospora </i>oocysts, for example, the fuzzy surface of raspberries may contribute to its contamination, when compared to the smoother surface of grapes. [[#References|[8]]] | ||
===Infectious dose, incubation, and colonization=== | ===Infectious dose, incubation, and colonization=== | ||
The infectious dose of oocysts needed to infect the host is relatively unknown, but it is thought to be in the low numbers. [[#References|[3]]] The incubation period for <i> Cyclospora cayetanensis </i> infection is at average one week, but can range from even 1 day to around two weeks. [[#References|[3]]] <i> Cyclospora cayetanensis </i> completes its life cycle in only one host, and can be broken into two phases-- exogenous and endogenous. The exogenous stage takes place outside the host, in the environment and is when an immature oocyst sporulates, becoming infectious for humans. During sporulation, the sporont divides into 2 sporocysts, each containing 2 sporozoites. [[#References|[5]]] This sporulation process requires some time, ranging from a few days to a couple of weeks, outside a host and exposed to the environment, which occurs only at appropriate oxygen concentrations, temperature, humidity, and other factors. [[#References|[3]]] The endogenous stage takes place in the human host. [[#References|[10]]] After ingestion of a sporulated <i> Cyclospora </i> oocysts, which is its infectious state, the oocysts releasing the sporozoites into the small intestine due to some special stimuli, such as the anaerobic condition in the GI tract, or the presence of bile salts. These sporozoites invade small intestine epithelia, or enterocytes especially in the jejunum and reside intracellular in a parasitophorous vacuole. [[#References|[10]]] Now, they undergo asexual division followed by sexual division and eventually produce unsporulated oocysts, and as the enterocytes die, they are are shed in the stool. [[#References|[5]]] In the environment, the oocyst sporulates, becoming infectious for humans and the life cycle process occurs again in another host that ingests the contaminated item. [[#References|[5]]] [[Image:Cyclospora_cayetanensis_Life_Cycle.gif|thumb|300px|left|Life Cycle of <i> Cyclospora cayetanensis </i> [From:http://www.cdc.gov]]] | |||
===Epidemiology=== | ===Epidemiology=== | ||
Cyclosporiasis occurs in many countries all over the world, but is more prevalent in tropical and subtropical regions, where people living there have an increased risk of infection, as well as the people traveling to those regions. [[#References|[2]]] <i> Cyclospora </i> has been shown to generally affect children in areas where access to clean water and sanitation is less than desired, for example in rural China 4% of preschool children with diarrhea had infection of <i> Cyclospora </i>. [[#References|[8]]] In Venezuela, parasites cause persistent health problems, including<i> Cyclospora cayetanensis </i>, which have infection rates of around 5.3% in children, along with 6-12% in immunocompromised patients. [[#References|[9]]] It is thought that infection is based on seasons, for example from epidemiological studies it seems that infection is higher in Peru from December to July or in the United States from May to July, however no consistent data has been able to prove that yet. [[#References|[3]]] In the United States, foodborne outbreaks of cyclosporiasis have involved imported fresh produce, for example in 1997, both contaminated raspberries and fresh basil resulted in 1,498 cases of disease. [[#References|[2]]] Epidemiologic data suggest that immunity may develop to <i> C. cayetanensis </i> in areas where cyclosporiasis is endemic and that the disease is more severe in naïve populations. [[#References|[6]]] | |||
===Virulence factors=== | ===Virulence factors=== | ||
<i> Cyclospora cayetanensis </i> infects the epithelial cells that line the small intestine using several mechanisms, however much is still not known about this parasites virulence factors and characteristics used to infected the host. Of course it is known that several requirements are needed for a parasite to cause disease in a host, and without these, the parasite would not be able to invade the host. These requirements include the ability for the organism’s infectious form, and in the case of <i> Cyclospora </i>, its oocyst, to survive in harsh environmental conditions. The oocyst has a thick bilayered wall, allowing the organism to be environmentally resistant and able to survive until ingestion of a host. 10 This characteristic help the oocyst to survive a chlorination process of water, leaving it still contaminated by the pathogen. Another helpful feature of the mature oocysts contributing to pathogenesis is its fibrillar coat, which is also seen in the noninfectious, unsporulated oocysts that are in the stool of infected hosts. 10 This fibrillar coat is thought to help the parasite adhere to the foods it is known to contaminate, like the basil leaf or raspberries. This fibrillar coat is thought to help the parasite adhere to the foods it is known to contaminate, like the basil leaf or raspberries. It has also been predicted that the symptom of watery diarrhea without blood or leukocytes present caused by <i> Cyclospora cayetanensis </i> infection may be due to an unidentified toxin causing said diarrhea. 10 | <i> Cyclospora cayetanensis </i> infects the epithelial cells that line the small intestine using several mechanisms, however much is still not known about this parasites virulence factors and characteristics used to infected the host. Of course it is known that several requirements are needed for a parasite to cause disease in a host, and without these, the parasite would not be able to invade the host. These requirements include the ability for the organism’s infectious form, and in the case of <i> Cyclospora </i>, its oocyst, to survive in harsh environmental conditions. The oocyst has a thick bilayered wall, allowing the organism to be environmentally resistant and able to survive until ingestion of a host, and allows the pathogen to survive while traveling through the stomach to get to the small intestine where it wants to be. [[#References|[10]]] This characteristic help the oocyst to survive a chlorination process of water, leaving it still contaminated by the pathogen. Another helpful feature of the mature oocysts contributing to pathogenesis is its fibrillar coat, which is also seen in the noninfectious, unsporulated oocysts that are in the stool of infected hosts. [[#References|[10]]] This fibrillar coat is thought to help the parasite adhere to the foods it is known to contaminate, like the basil leaf or raspberries. This fibrillar coat is thought to help the parasite adhere to the foods it is known to contaminate, like the basil leaf or raspberries. It has also been predicted that the symptom of watery diarrhea without blood or leukocytes present caused by <i> Cyclospora cayetanensis </i> infection may be due to an unidentified toxin causing said diarrhea. [[#References|[10]]] | ||
==Clinical features== | ==Clinical features== | ||
Typical symptoms of <i> Cyclospora cayetanensis </i> infection include most commonly watery diarrhea, that can sometimes be described as explosive, along with abdominal cramping, loss of appetite, weight loss, nausea and vomiting, all associated with an early onset. [[#References|[1]]] It can also include headaches, and a low fever, sometimes described as flu-like symptoms, however it is possible that the infected host do not even have symptoms. These symptoms, if not treated can last an average of 7 days, but can range anywhere from a few days to a month or longer, and even though the infection can resolve itself, if treated with specific drugs, the symptoms are resolved faster, compared to untreated patients. [[#References|[1]]] It is always possible for symptoms of infection to relapse, or come back. Infection in travelers are more severe in symptoms, while in <i> Cyclospora </i> endemic countries about 70% of children often have asymptomatic infections, while adults are occasionally infected. [[#References|[5]]] <i> Cyclospora cayetanensis </i> infection is not considered a fatal disease, and there have been no reported deaths attributed to the actual parasite in the United States, however it is when the infection induces protracted diarrhea onto the host, which could possibly lead to severe dehydration if not taken care. [[#References|[5]]] Infants are at greater risk for dehydration due to prolonged diarrhea as a symptom from infection. Diarrheal diseases attribute to over two million deaths in children each year, however it is not known how many of these could be due to <i> Cyclospora </i> infection. [[#References|[5]]] | |||
==Diagnosis== | ==Diagnosis== | ||
The first step in diagnosis of <i> Cyclospora cayetanensis </i> infection should be when health care providers notice the symptom of prolonged diarrhea in the patient, and should also look at the other symptoms associated with the disease as well. If the patient has recently traveled to a tropical or sub-tropical area that is known for causing infection, the healthcare provider should ask the patient for a stool sample 3 However, because testing for <i> Cyclospora </i> is not usually done in most laboratories in the US when the stool is tested for parasites, identification for <i> C. cayetanensis </i> in the stool requires special lab tests not routinely done, therefore this microorganism can be difficult to diagnose, especially when it comes to laboratory tests. This is because even if an infected patient is symptomatic, there may not be enough oocysts in the stool to detect infection in lab examinations; therefore it is not uncommonly needed for the patient to provide multiple stool specimens ranging within several days. 2 Identification of this organism can be made through microscopic techniques, usually several different stains, such as Acid-fast stains, or using an | [[File:Autofluorescence_of_Cyclospora.jpg|700px|thumb|right|Autofluorescence of <i> Cyclospora cayetanensis </i> oocysts. [From:http://www.cdc.gov]]] | ||
The first step in diagnosis of <i> Cyclospora cayetanensis </i> infection should be when health care providers notice the symptom of prolonged diarrhea in the patient, and should also look at the other symptoms associated with the disease as well. If the patient has recently traveled to a tropical or sub-tropical area that is known for causing infection, the healthcare provider should ask the patient for a stool sample. [[#References|[3]]] However, because testing for <i> Cyclospora </i> is not usually done in most laboratories in the US when the stool is tested for parasites, identification for <i> C. cayetanensis </i> in the stool requires special lab tests not routinely done, therefore this microorganism can be difficult to diagnose, especially when it comes to laboratory tests. This is because even if an infected patient is symptomatic, there may not be enough oocysts in the stool to detect infection in lab examinations; therefore it is not uncommonly needed for the patient to provide multiple stool specimens ranging within several days. [[#References|[2]]] Identification of this organism can be made through microscopic techniques, usually several different stains, such as Acid-fast stains, or using an ultraviolet microscope, in which the the autofluorescent <i> Cyclospora </i>oocyst appear a neon-blue color. [[#References|[1]]] Due to the face that <i> Cyclospora cayetanensis </i> is unable to be culture in the laboratory and its small size, it is near impossible to detect and isolate the organism on the contaminated food since the amount of organisms on it are so low. [[#References|[3]]] | |||
==Treatment== | ==Treatment== | ||
The specific drug treatment for disease caused by <i> Cyclospora cayetanensis </i> | The specific drug treatment for disease caused by <i> Cyclospora cayetanensis </i>is the combination of two antibiotics—trimethoprim and sulfamethoxazole (co-trimaxazole), which are also sold under the names of Bactrim, Cotrim, or Septra, and symptoms can diminish within the next several days. [[#References|[1]]] Unfortunately, there have been no alternative drug treatment options that have been effective for patients that suffer from a sulfa allergy or do not respond to the combination antibiotic. [[#References|[2]]] Of course anti-diarrheal medication can be given by a health care provider to reduce the diarrheal symptom, but this does not actually combat against the microorganism. Hydration and rest are also essential to patients with diarrhea, and in most healthy individuals the infection can be self-limiting, and most can recover in a few days, or possibly a month or longer. [[#References|[2]]] If left untreated the protracted diarrhea can lead to severe dehydration, and in cases like these hospitalization may occur. | ||
is the combination of two antibiotics—trimethoprim and sulfamethoxazole (co-trimaxazole), which are also sold under the names of Bactrim, Cotrim, or Septra, and symptoms can diminish within the next several days. | |||
==Prevention== | ==Prevention== | ||
<i> Cyclospora cayetanensis </i> oocysts, which are the cause of infection, are transmitted via the fecal-oral route, therefore the best prevention for infection of this microorganism is to simply avoid food or water that may have been contaminated with feces containing the infectious oocysts. 2 It is possible for <i> Cyclospora </i> to re-infect the same host more than once. Since most of the U.S cases of disease are caused from either imported contaminated food, or traveling to <i> Cyclospora </i>-endemic areas, it is important for travelers to be precautious about food and water consumption. Even if contaminated food or water is treated with chlorine and iodine, infectious <i> Cyclospora </i> oocyts are likely to remain, so drinking bottle water, and avoiding street venders are the safest ways to avoid infection. 2 Other good practices are to use proper hand washing techniques, and washing all food thoroughly. | <i> Cyclospora cayetanensis </i> oocysts, which are the cause of infection, are transmitted via the fecal-oral route, therefore the best prevention for infection of this microorganism is to simply avoid food or water that may have been contaminated with feces containing the infectious oocysts. [[#References|[2]]] It is possible for <i> Cyclospora </i> to re-infect the same host more than once. Since most of the U.S cases of disease are caused from either imported contaminated food, or traveling to <i> Cyclospora </i>-endemic areas, it is important for travelers to be precautious about food and water consumption. Even if contaminated food or water is treated with chlorine and iodine, infectious <i> Cyclospora </i> oocyts are likely to remain, so drinking bottle water, and avoiding street venders are the safest ways to avoid infection. [[#References|[2]]] Other good practices are to use proper hand washing techniques, and washing all food thoroughly. | ||
==Host Immune Response== | ==Host Immune Response== | ||
Upon the parasitic invasion, specifically when the sporozoites are released from the oocyst in the small intestine, the host mounts an innate and apaptive immune response. The the sporozoite invades the epithelial cells, or the enterocytes in that area, and there is a release of cytokines from the cells, which activate and recruit phagocytes from the blood to the site of infection. [[#References|[10]]] These phagocytes release several factors that increase intestinal secretion of chloride and water, and inhibit absorption. Not only is there enterocyte damage directly from the parasite itself, but inflammation can also lead to damage. T cells, protease, and oxidants secreted by mast cells are responsible for this occurring and as a result from this distruction of enterocytes, there is nutrient malabsorption and increased secretion of fluids and electrolytes, which give the watery diarrhea. [[#References|[10]]] | |||
==References== | ==References== | ||
1. Curry A, Smith HV: Emerging pathogens: <i>Isospora</i>, <i>Cyclospora</i> and microsporidia. <i>Parasitology</i> 1999, 117: 143-159. Available at http://journals.cambridge.org.ezproxy.lib.ou.edu/action/displayAbstract?fromPage=online&aid=24615&fileId=S0031182099004904<br> | |||
2. Centers for Disease Control and Prevention (CDC). Parasites- Cyclosporiasis (Cyclospora Infection). Available at http://www.cdc.gov/parasites/cyclosporiasis/.<br> | |||
3. Food and Drug Administration. <i>Bad Bug Book, Foodborne Pathogenic Microorganisms and Natural Toxins</i>. Second Edition. [<i>Cyclospora cayetanensis</i>]. 2012. <br> | |||
4. Pierce K, Huston CD. Protozoan, Intestinal. <i>Eukaryotic Microbes</i>. 2012; 23: 323-332. Available at http://books.google.it/books?id=DJLIhDnqMk0C&pg=PA324&lpg=PA324&dq=host+immune+response+to+Cyclospora+cayetanensis&source=bl&ots=qtpoYfwyMX&sig=GY-TCoWOznpMMnEhrC7SijQePbg&hl=en&sa=X&ei=hODPU8zgDPD64QTXyYGABg&ved=0CDQQ6AEwAg#v=onepage&q=host%20immune%20response%20to%20Cyclospora%20cayetanensis&f=false<br> | |||
5. Medscape. Cyclospora. Available at http://emedicine.medscape.com/article/236105-overview.<br> | |||
6. Alfano-Sobsey EM, Eberhard ML, Seed JR, Weber DJ, Won KY, Nace EK, Moe CL. (2004). Human Challenge Pilot Study with <i>Cyclospora cayetanensis</i>. <i>Emerging Infectious Diseases</i> [CDC] 10(4). Available at http://wwwnc.cdc.gov/eid/article/10/4/03-0356_article<br> | |||
7. Herwaldt BL. “<i>Cyclospora cayetanensis</i>: A Review, Focusing on the Outbreaks of Cyclosporiasis in the 1990s”. (2000). Clinical Infectious Diseases, 31:1040-57. Available at http://www.bvsde.ops-oms.org/bvsacg/e/cdcagua/guias/b.parametos/3.RefB/microbiologicos/Cap11.3/04/04.000497.pdf<br> | |||
8. Motarjemi, Yasmine Moy, Gerald Todd, Ewen (2014). Encyclopedia of Food Safety. Elsevier. Available at:https://app.knovel.com/web/view/swf/show.v/rcid:kpEFS00001/cid:kt00C6CF82/viewerType:pdf/root_slug:encyclopedia-food-safety?cid=kt00C6CF82&page=1&b-toc-cid=kpEFS00001&b-toc-root-slug=encyclopedia-food-safety&b-toc-url-slug=protozoa&b-toc-title=Encyclopedia%20of%20Food%20Safety <br> | |||
9. Chacin-Bonilla L. "<i>Cyclospora cayetanensis</i>as a Global Health Problem". Epidemiol. 2(3). Available at: http://omicsonline.org/cyclospora-cayetanensis-as-a-global-health-problem-2161-1165.1000e110.pdf <br> | |||
10. Ghimire TR, Sherchan JB. “Human Infection of <i> Cyclospora cayetanensis </i>: A Review on its Medico-biological and Epidemiological Pattern in Global Scenario”. 2008. Journal of Nepal Health Research Council 4(10):25-40.<br> | |||
Created by Kristen Hoelscher, student of Tyrrell Conway at the University of Oklahoma. | |||
Latest revision as of 14:34, 11 February 2016

Etiology/Bacteriology
Taxonomy
| Domain = Eukaryota | Phylum = Apicomplexa | Class = Coccidia | Order = Eucoccidiorida | Family = Eimeriidae | Genus = Cyclospora | species = C. cayetanensis
|
NCBI: [2] |
Description
Cyclospora cayetanensis is a parasitic pathogen that causes Cyclosporiasis, which is characterized by prolonged watery diarrhea and intestinal distress, also including abdominal pain among many other symptoms. [3] Cyclospora cayetanensis is an obligate intracellular, coccidian protozoan pathogen to humans, classified within the phylum Apicomplexa, and is known to for several food-borne outbreaks in the United States. [1] The oocyst of Cyclospora cayetanensis is a spherical shape, and can range from 8 to 10 μm, and after sporulation each oocyst contains four sporozoites ready for invasion of the host. [8] Cyclospora cayetanensis causes infection by the ingestion of contaminated foods or liquids by a sporulated oocyst that is in its infectious stage; unsporulated oocysts are not infectious to hosts and must first complete sporulation outside the host to become infectious. [1] All organisms under the Apicompleza phylum have a complex life cycle involving an invasive stage, using specialized organelles for penetration and invasion of host cell. [4] This pathogen is known to cause traveller’s diarrhea in infected hosts, and several water-borne and food-borne outbreaks of this microorganism have been reported in the past decades. [1] The infection is usually self-limiting, however for more persistent cases of infection, drug treatment is available. Diagnosis for this organism can be difficult, but improved diagnostic methods such as autofluorescence, has assisted in easier detection of C. cayetanensis oocysts in stool samples. Even though there are several species of Cyclospora that also develop in the gastrointestinal tract of vertebrates, only Cyclospora cayetanensis had been observed to cause illness in humans. [3]
Pathogenesis
Transmission
Cyclospora cayetanensis is spread via the fecal-oral route, meaning that the host must ingest something, food or water for example, that had been contaminated with feces that contain infectious oocysts; to be infectious the oocyst has to be sporulated. An unsporulated oocyst takes from days to weeks outside a host cell after being excreted in a fecal matter of an infected host to become a sporulated oocyst, now capable of infecting another host. [2] Imported fresh produce from tropical regions, such as raspberries, basil and lettuce have caused outbreaks of cyclosporiasis from contamination from feces. [3] Essentially, any food that has been contaminated with fecal matter containing infectious, sporulated oocysts have the potential to cause infection of Cyclospora cayetanensis . To date, there has been no documented transmission from human-to-human, likely due to the amount of time outside a host the oocyst has be to transform into a sporulated oocyst capable of infection. [5] It is thought that the topology of the surface of certain kinds of fruits and vegetables help contribute to adherence and of the Cyclospora oocysts, for example, the fuzzy surface of raspberries may contribute to its contamination, when compared to the smoother surface of grapes. [8]
Infectious dose, incubation, and colonization
The infectious dose of oocysts needed to infect the host is relatively unknown, but it is thought to be in the low numbers. [3] The incubation period for Cyclospora cayetanensis infection is at average one week, but can range from even 1 day to around two weeks. [3] Cyclospora cayetanensis completes its life cycle in only one host, and can be broken into two phases-- exogenous and endogenous. The exogenous stage takes place outside the host, in the environment and is when an immature oocyst sporulates, becoming infectious for humans. During sporulation, the sporont divides into 2 sporocysts, each containing 2 sporozoites. [5] This sporulation process requires some time, ranging from a few days to a couple of weeks, outside a host and exposed to the environment, which occurs only at appropriate oxygen concentrations, temperature, humidity, and other factors. [3] The endogenous stage takes place in the human host. [10] After ingestion of a sporulated Cyclospora oocysts, which is its infectious state, the oocysts releasing the sporozoites into the small intestine due to some special stimuli, such as the anaerobic condition in the GI tract, or the presence of bile salts. These sporozoites invade small intestine epithelia, or enterocytes especially in the jejunum and reside intracellular in a parasitophorous vacuole. [10] Now, they undergo asexual division followed by sexual division and eventually produce unsporulated oocysts, and as the enterocytes die, they are are shed in the stool. [5] In the environment, the oocyst sporulates, becoming infectious for humans and the life cycle process occurs again in another host that ingests the contaminated item. [5]
Epidemiology
Cyclosporiasis occurs in many countries all over the world, but is more prevalent in tropical and subtropical regions, where people living there have an increased risk of infection, as well as the people traveling to those regions. [2] Cyclospora has been shown to generally affect children in areas where access to clean water and sanitation is less than desired, for example in rural China 4% of preschool children with diarrhea had infection of Cyclospora . [8] In Venezuela, parasites cause persistent health problems, including Cyclospora cayetanensis , which have infection rates of around 5.3% in children, along with 6-12% in immunocompromised patients. [9] It is thought that infection is based on seasons, for example from epidemiological studies it seems that infection is higher in Peru from December to July or in the United States from May to July, however no consistent data has been able to prove that yet. [3] In the United States, foodborne outbreaks of cyclosporiasis have involved imported fresh produce, for example in 1997, both contaminated raspberries and fresh basil resulted in 1,498 cases of disease. [2] Epidemiologic data suggest that immunity may develop to C. cayetanensis in areas where cyclosporiasis is endemic and that the disease is more severe in naïve populations. [6]
Virulence factors
Cyclospora cayetanensis infects the epithelial cells that line the small intestine using several mechanisms, however much is still not known about this parasites virulence factors and characteristics used to infected the host. Of course it is known that several requirements are needed for a parasite to cause disease in a host, and without these, the parasite would not be able to invade the host. These requirements include the ability for the organism’s infectious form, and in the case of Cyclospora , its oocyst, to survive in harsh environmental conditions. The oocyst has a thick bilayered wall, allowing the organism to be environmentally resistant and able to survive until ingestion of a host, and allows the pathogen to survive while traveling through the stomach to get to the small intestine where it wants to be. [10] This characteristic help the oocyst to survive a chlorination process of water, leaving it still contaminated by the pathogen. Another helpful feature of the mature oocysts contributing to pathogenesis is its fibrillar coat, which is also seen in the noninfectious, unsporulated oocysts that are in the stool of infected hosts. [10] This fibrillar coat is thought to help the parasite adhere to the foods it is known to contaminate, like the basil leaf or raspberries. This fibrillar coat is thought to help the parasite adhere to the foods it is known to contaminate, like the basil leaf or raspberries. It has also been predicted that the symptom of watery diarrhea without blood or leukocytes present caused by Cyclospora cayetanensis infection may be due to an unidentified toxin causing said diarrhea. [10]
Clinical features
Typical symptoms of Cyclospora cayetanensis infection include most commonly watery diarrhea, that can sometimes be described as explosive, along with abdominal cramping, loss of appetite, weight loss, nausea and vomiting, all associated with an early onset. [1] It can also include headaches, and a low fever, sometimes described as flu-like symptoms, however it is possible that the infected host do not even have symptoms. These symptoms, if not treated can last an average of 7 days, but can range anywhere from a few days to a month or longer, and even though the infection can resolve itself, if treated with specific drugs, the symptoms are resolved faster, compared to untreated patients. [1] It is always possible for symptoms of infection to relapse, or come back. Infection in travelers are more severe in symptoms, while in Cyclospora endemic countries about 70% of children often have asymptomatic infections, while adults are occasionally infected. [5] Cyclospora cayetanensis infection is not considered a fatal disease, and there have been no reported deaths attributed to the actual parasite in the United States, however it is when the infection induces protracted diarrhea onto the host, which could possibly lead to severe dehydration if not taken care. [5] Infants are at greater risk for dehydration due to prolonged diarrhea as a symptom from infection. Diarrheal diseases attribute to over two million deaths in children each year, however it is not known how many of these could be due to Cyclospora infection. [5]
Diagnosis
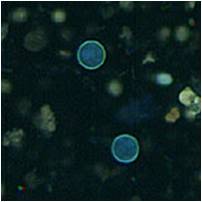
The first step in diagnosis of Cyclospora cayetanensis infection should be when health care providers notice the symptom of prolonged diarrhea in the patient, and should also look at the other symptoms associated with the disease as well. If the patient has recently traveled to a tropical or sub-tropical area that is known for causing infection, the healthcare provider should ask the patient for a stool sample. [3] However, because testing for Cyclospora is not usually done in most laboratories in the US when the stool is tested for parasites, identification for C. cayetanensis in the stool requires special lab tests not routinely done, therefore this microorganism can be difficult to diagnose, especially when it comes to laboratory tests. This is because even if an infected patient is symptomatic, there may not be enough oocysts in the stool to detect infection in lab examinations; therefore it is not uncommonly needed for the patient to provide multiple stool specimens ranging within several days. [2] Identification of this organism can be made through microscopic techniques, usually several different stains, such as Acid-fast stains, or using an ultraviolet microscope, in which the the autofluorescent Cyclospora oocyst appear a neon-blue color. [1] Due to the face that Cyclospora cayetanensis is unable to be culture in the laboratory and its small size, it is near impossible to detect and isolate the organism on the contaminated food since the amount of organisms on it are so low. [3]
Treatment
The specific drug treatment for disease caused by Cyclospora cayetanensis is the combination of two antibiotics—trimethoprim and sulfamethoxazole (co-trimaxazole), which are also sold under the names of Bactrim, Cotrim, or Septra, and symptoms can diminish within the next several days. [1] Unfortunately, there have been no alternative drug treatment options that have been effective for patients that suffer from a sulfa allergy or do not respond to the combination antibiotic. [2] Of course anti-diarrheal medication can be given by a health care provider to reduce the diarrheal symptom, but this does not actually combat against the microorganism. Hydration and rest are also essential to patients with diarrhea, and in most healthy individuals the infection can be self-limiting, and most can recover in a few days, or possibly a month or longer. [2] If left untreated the protracted diarrhea can lead to severe dehydration, and in cases like these hospitalization may occur.
Prevention
Cyclospora cayetanensis oocysts, which are the cause of infection, are transmitted via the fecal-oral route, therefore the best prevention for infection of this microorganism is to simply avoid food or water that may have been contaminated with feces containing the infectious oocysts. [2] It is possible for Cyclospora to re-infect the same host more than once. Since most of the U.S cases of disease are caused from either imported contaminated food, or traveling to Cyclospora -endemic areas, it is important for travelers to be precautious about food and water consumption. Even if contaminated food or water is treated with chlorine and iodine, infectious Cyclospora oocyts are likely to remain, so drinking bottle water, and avoiding street venders are the safest ways to avoid infection. [2] Other good practices are to use proper hand washing techniques, and washing all food thoroughly.
Host Immune Response
Upon the parasitic invasion, specifically when the sporozoites are released from the oocyst in the small intestine, the host mounts an innate and apaptive immune response. The the sporozoite invades the epithelial cells, or the enterocytes in that area, and there is a release of cytokines from the cells, which activate and recruit phagocytes from the blood to the site of infection. [10] These phagocytes release several factors that increase intestinal secretion of chloride and water, and inhibit absorption. Not only is there enterocyte damage directly from the parasite itself, but inflammation can also lead to damage. T cells, protease, and oxidants secreted by mast cells are responsible for this occurring and as a result from this distruction of enterocytes, there is nutrient malabsorption and increased secretion of fluids and electrolytes, which give the watery diarrhea. [10]
References
1. Curry A, Smith HV: Emerging pathogens: Isospora, Cyclospora and microsporidia. Parasitology 1999, 117: 143-159. Available at http://journals.cambridge.org.ezproxy.lib.ou.edu/action/displayAbstract?fromPage=online&aid=24615&fileId=S0031182099004904
2. Centers for Disease Control and Prevention (CDC). Parasites- Cyclosporiasis (Cyclospora Infection). Available at http://www.cdc.gov/parasites/cyclosporiasis/.
3. Food and Drug Administration. Bad Bug Book, Foodborne Pathogenic Microorganisms and Natural Toxins. Second Edition. [Cyclospora cayetanensis]. 2012.
4. Pierce K, Huston CD. Protozoan, Intestinal. Eukaryotic Microbes. 2012; 23: 323-332. Available at http://books.google.it/books?id=DJLIhDnqMk0C&pg=PA324&lpg=PA324&dq=host+immune+response+to+Cyclospora+cayetanensis&source=bl&ots=qtpoYfwyMX&sig=GY-TCoWOznpMMnEhrC7SijQePbg&hl=en&sa=X&ei=hODPU8zgDPD64QTXyYGABg&ved=0CDQQ6AEwAg#v=onepage&q=host%20immune%20response%20to%20Cyclospora%20cayetanensis&f=false
5. Medscape. Cyclospora. Available at http://emedicine.medscape.com/article/236105-overview.
6. Alfano-Sobsey EM, Eberhard ML, Seed JR, Weber DJ, Won KY, Nace EK, Moe CL. (2004). Human Challenge Pilot Study with Cyclospora cayetanensis. Emerging Infectious Diseases [CDC] 10(4). Available at http://wwwnc.cdc.gov/eid/article/10/4/03-0356_article
7. Herwaldt BL. “Cyclospora cayetanensis: A Review, Focusing on the Outbreaks of Cyclosporiasis in the 1990s”. (2000). Clinical Infectious Diseases, 31:1040-57. Available at http://www.bvsde.ops-oms.org/bvsacg/e/cdcagua/guias/b.parametos/3.RefB/microbiologicos/Cap11.3/04/04.000497.pdf
8. Motarjemi, Yasmine Moy, Gerald Todd, Ewen (2014). Encyclopedia of Food Safety. Elsevier. Available at:https://app.knovel.com/web/view/swf/show.v/rcid:kpEFS00001/cid:kt00C6CF82/viewerType:pdf/root_slug:encyclopedia-food-safety?cid=kt00C6CF82&page=1&b-toc-cid=kpEFS00001&b-toc-root-slug=encyclopedia-food-safety&b-toc-url-slug=protozoa&b-toc-title=Encyclopedia%20of%20Food%20Safety
9. Chacin-Bonilla L. "Cyclospora cayetanensisas a Global Health Problem". Epidemiol. 2(3). Available at: http://omicsonline.org/cyclospora-cayetanensis-as-a-global-health-problem-2161-1165.1000e110.pdf
10. Ghimire TR, Sherchan JB. “Human Infection of Cyclospora cayetanensis : A Review on its Medico-biological and Epidemiological Pattern in Global Scenario”. 2008. Journal of Nepal Health Research Council 4(10):25-40.
Created by Kristen Hoelscher, student of Tyrrell Conway at the University of Oklahoma.
