Shigella boydii: Difference between revisions
No edit summary |
|||
| (17 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
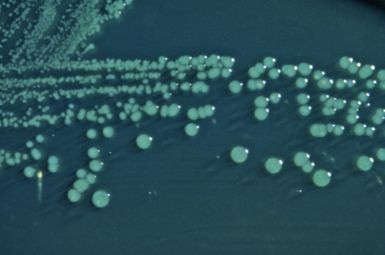
[[image:shigella_boydii_01.jpg|right|thumb|385px|[[help:contents|S. boydii on Hektoen enteric(HE) agar. Image in public domain; found in CDC.]]]] | {{Curated}} | ||
[[image:shigella_boydii_01.jpg|right|thumb|385px|[[help:contents|''S. boydii'' on Hektoen enteric(HE) agar. Image in public domain; found in CDC.]]]] | |||
{{Biorealm Genus}} | {{Biorealm Genus}} | ||
| Line 28: | Line 29: | ||
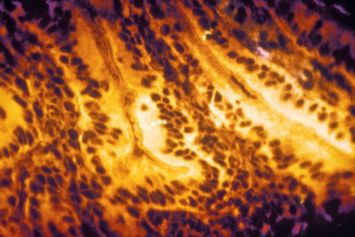
[[image:1st_stage_shiga.jpg|right|thumb|355px|[[help:contents|This micrograph reveals the first stage of shigellosis as it progresses; by this stage, the Shigella bacteria have penetrated the intestinal mucosa. Image in public domain; found in CDC.]]]] | [[image:1st_stage_shiga.jpg|right|thumb|355px|[[help:contents|This micrograph reveals the first stage of shigellosis as it progresses; by this stage, the Shigella bacteria have penetrated the intestinal mucosa. Image in public domain; found in CDC.]]]] | ||
In the 1950's Shigella was accepted as a genus and subgrouped into four species: ''S. dysenteriae'', ''S. | In the 1950's Shigella was accepted as a genus and subgrouped into four species: ''S. dysenteriae'', ''S. fexneri'', ''S. boydii'', and ''S. sonnei'' (also referred to as subgroups A-D).[3] | ||
'''Appearance:''' ''Shigella boydii'' is a bacillary (rod-shaped) gram negative bacterium that does not form spores and is usually nonmotile.[2][5] | '''Appearance:''' ''Shigella boydii'' is a bacillary (rod-shaped) gram-negative bacterium that does not form spores and is usually nonmotile.[2][5] | ||
'''Habitat:''' ''S. boydii'' inhabits the intestine and rectum of humans and other primates. It can survive | '''Habitat:''' ''S. boydii'' inhabits the intestine and rectum of humans and other primates. It can survive in feces and soil and/or food/water contaminated with fecal matter. For example, in Guadalajara, Mexico, Salmonella and Shigella species were found in freshly squeezed orange juice, oranges, and wiping cloths found in public markets and street booths. ''S. boydii'' was specifically found in the oranges and wiping cloths. This may indicate poor sanitary methods of food processing which led to raw sewage exposure.[13][14] | ||
Locationally, ''S. boydii'' is found mainly on the sub-continent of India.[3] | |||
'''Significance:''' Human pathogen that causes bacillary dysentery. | '''Significance:''' Human pathogen that causes bacillary dysentery.[4] | ||
'''Serotypes:''' There are 20 ''S. boydii'' serotypes.[5] | '''Serotypes:''' There are 20 ''S. boydii'' serotypes.[5] | ||
| Line 47: | Line 49: | ||
'''Pathogenic Contents:''' The one plasmid, pSb4_227, has post-segregation killing systems mvpA/mvpT, found in all Shigella species' plasmids and ccdA/ccdB not found in some.[3] | '''Pathogenic Contents:''' The one plasmid, pSb4_227, has post-segregation killing systems mvpA/mvpT, found in all Shigella species' plasmids and ccdA/ccdB not found in some.[3] | ||
It is believed that most Shigella have gained and | It is believed that most Shigella have gained and lost Stx genes at one time or another, the toxin genes found in ''S. dysenteriae''. One evidence of this is Sb227 which has a T2SS pseudogene. T2SS, found in ''S. dysenteriae'', enables export of toxins to host that would otherwise build up inside of the cell and cause lysis, therefore T2SS greatly contributes to pathogenicity. This inactivation of T2SS in ''S. boydii'' has most likely been naturally selected to better adapt to a human host as having greater pathogenicity offers little benefit for longterm survival.[3] | ||
Sb227 contains pathogenic islands SHI-1, SHI-2 and ipaH (invasion plasmid antigen). Insertion (IS) element IS''Sbo6'' is restricted in SHI-1, SHI-2 and ipaH pathogenic islands. This | Sb227 contains pathogenic islands SHI-1, SHI-2 and ipaH (invasion plasmid antigen). Insertion (IS) element IS''Sbo6'' is restricted in SHI-1, SHI-2 and ipaH pathogenic islands. This suggests that these islands were acquired before the IS-element.[3] | ||
'''Iron Up-take:''' Iron is taken up from the environment by ABC transporters and by the iron transport compound aerobactin.[3] | '''Iron Up-take:''' Iron is taken up from the environment by ABC transporters and by the iron transport compound aerobactin.[3] | ||
| Line 58: | Line 60: | ||
==Cell Structure and Metabolism== | ==Cell Structure and Metabolism== | ||
'''Cell Structure:''' Shigella structural characteristics follow that of Gram-negative bacteria. Most research would agree that Shigella are nonmotile but some evidence suggests that they do in fact have flagella, although motility is not necessary for infection of intestine. The | '''Cell Structure:''' Shigella's structural characteristics follow that of Gram-negative bacteria. Most research would agree that Shigella are nonmotile but some evidence suggests that they do in fact have flagella, although motility is not necessary for infection of intestine. The flagella tend to be on one pole of the cell and about 10 microns in length and 12-14nm in diameter. The genes coding for the flagella in ''S. dysenteriae'', ''S. flexneri'', ''S. boydii'' and ''S. sonnei'' were found to be different and attribute to the genetic diversity among the species.[8] | ||
'''Metabolism:''' ''S. boydii'' typically does not have oxidase enzymes but rather catalase enzymes (catalyzes the reduction of H2O2->H20). | '''Metabolism:''' ''S. boydii,'' when found in the intestine, go though anaerobic metabolic pathways but can survive outside of the body due to its ability to utilize aerobic pathways.[14] More specifically, ''S. boydii,'' typically does not have oxidase enzymes but rather catalase enzymes (catalyzes the reduction of H2O2->H20). Methyl red testing is positive, meaning that the bacteria uses a mixed acid fermentation pathway. Voges–Proskauer and Simmons’ citrate reactions are negative, meaning that this organism does not utilize the butylene glycol pathway or produce acetoin. Lysine decarboxylase, arginine dihydrolase and ornithine decarboxylase are not present. ''S. boydii'' does not produce H2S, does not hydrolyze urea and does not grow in KCN broth. Carbohydrates are usually fermented and these include glucose (in the absence of gas production), D-mannitol, arabinose, trehalose and mannose.[7] | ||
==Ecology/Pathology== | ==Ecology/Pathology== | ||
| Line 67: | Line 69: | ||
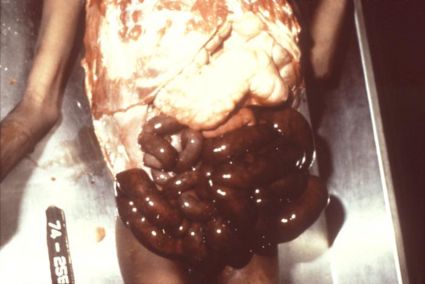
Shigella bacteria cause diarrhea and shigellosis (bacillary dysentery) through oral-fecal transmission. Shigella is a highly infective agent able to infect a host with less than 20 | Shigella bacteria cause diarrhea and shigellosis (bacillary dysentery) through oral-fecal transmission. Shigella is a highly infective agent able to infect a host with less than 20 cells with an onset of about 12-48 hours, in favorable conditions. Once ingested, the Shigella makes its way through the gastrointestinal tract until it reaches the epithelial cells of the intestinal mucosa, there it infects, causing irritation, inflammation and necrosis (swelling and breaking of infected cells, which spreads infection). General symptoms include stomach cramps, high fever, mucus in feces, and bloody diarrhea due to ulceration of intestinal lining and rectum. [[image:Necrosis.jpg|left|thumb|425px|[[help:contents|This man developed necrosis of the intestines due to a Shigellosis infection resulting in his death. Image in public domain; found in CDC.]]]]In most cases these symptoms are mild and resolve in about a week but other cases can become severe enough to be fatal without proper medical care. The elderly, very young and those weakened by disease are much more sensitive to the bacteria. In very young children very high fever may also be accompanied with seizures.[4] Usually Shigella bacteria are found in areas of poor sanitation. Food washed with contaminated water or not cleaned properly may also be a target. In 1998 an outbreak of Shigellosis occurred in Chicago due to ''Shigella boydii'' type 18 found on the cilantro and parsley in bean salad.[6] | ||
Shigella species account for less than 10% of all foodborne illnesses reported in the United States. With an estimated 300,000 yearly incidents of shigellosis in the U.S., the exact percentage due to food contamination is unknown, due to the difficulty in isolating the bacteria from food but given its infectiousness the number is undoubtedly high.[2] | |||
==Current Research== | ==Current Research== | ||
'''1.''' Comparisons between Shigella species and between E. coli have been made and are being made in order to better understand Shigella's pathogenicity, patterns of infection, and varying | '''1.''' Comparisons between Shigella species and between ''E. coli'' have been made and are being made in order to better understand Shigella's pathogenicity, patterns of infection, and varying harmfulness. Answers to these questions will hopefully lead to better avoidance and treatment of shigellosis in the future.[3] | ||
'''2.''' At the National Shigella Reference Centre in Israel during the years 2000- 2004, 5,616 Shigella isolates were tested for resistance to certain antibacterial products. In one strain of Shigella boydii 2 and in two strains each of Shigella flexneri 2a, S. flexneri 6, and Shigella sonnei there was discovered resistance to ceftriaxone. All of these strains were found to be producers of extended-spectrum beta-lactamase (ESBL) and also very sensitive to tazobactam which inhibits the bacterial beta-lactamases. More research is needed to determine the rate of resistance to antibiotics and rate of transfer of resistant genes.[9] | '''2.''' At the National Shigella Reference Centre in Israel during the years 2000- 2004, 5,616 Shigella isolates were tested for resistance to certain antibacterial products. In one strain of ''Shigella boydii'' 2 and in two strains each of ''Shigella flexneri'' 2a, ''S. flexneri'' 6, and ''Shigella sonnei'' there was discovered resistance to ceftriaxone. All of these strains were found to be producers of extended-spectrum beta-lactamase (ESBL) and also very sensitive to tazobactam which inhibits the bacterial beta-lactamases. More research is needed to determine the rate of resistance to antibiotics and rate of transfer of resistant genes.[9] | ||
'''3.''' At the French National Reference Centre for Escherichia coli and Shigella, from 2000- 2004, 4,198 Shigella isolates were obtained. 180 of those isolates, taken from patients infected with diarrhea and dysentery, did not respond to any available antisera (serum containing antibodies) that had been used on all known S. boydii serotypes. All of the isolates shared characteristics of S. boydii serotypes except that their rRNA genes were unique from all others. A new antiserum was manufactured and destroyed the new serotype S. boydii 20. 91 of the 180 patients had traveled internationally while infected therefore further studies must be done in order to determine the epidemiology of this serogroup and the its | '''3.''' At the French National Reference Centre for ''Escherichia coli'' and Shigella, from 2000- 2004, 4,198 Shigella isolates were obtained. 180 of those isolates, taken from patients infected with diarrhea and dysentery, did not respond to any available antisera (serum containing antibodies) that had been used on all known ''S. boydii'' serotypes. All of the isolates shared characteristics of ''S. boydii'' serotypes except that their rRNA genes were unique from all others. A new antiserum was manufactured and destroyed the new serotype ''S. boydii'' 20. 91 of the 180 patients had traveled internationally while infected therefore further studies must be done in order to determine the epidemiology of this serogroup and the its potentially widespread threat.[10] | ||
==References== | ==References== | ||
| Line 104: | Line 107: | ||
12. Entrez Genome. "S. boydii (serotype 4) Sb227 pSB4_227, 126697 bp" (2005). NC_007608 NCBI. <http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?db=genome&cmd=Retrieve&dopt=Overview&list_uids=19003>. | 12. Entrez Genome. "S. boydii (serotype 4) Sb227 pSB4_227, 126697 bp" (2005). NC_007608 NCBI. <http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?db=genome&cmd=Retrieve&dopt=Overview&list_uids=19003>. | ||
13. Castillo A, Villarruel-López A, Navarro-Hidalgo V, Martínez-González NE, Torres-Vitela MR. "Salmonella and Shigella in freshly squeezed orange juice, fresh oranges, and wiping cloths collected from public markets and street booths in Guadalajara, Mexico: incidence and comparison of analytical routes." Journal of Food Protection. 69 (11) (2006): 2595-2599. NCBI. <http://www.ncbi.nlm.nih.gov/sites/entrez?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids=17133801>. | |||
14. Prema P, Palavesam A, Balaji P. "Aerobic heterotrophic bacterial diversity in sediments of Rajakkamangalam estuary, south west coast of India." Journal of Environmental Biology. 26 (4) (2005): 729-724. NCBI. <http://www.ncbi.nlm.nih.gov/sites/entrez?Db=pubmed&Cmd=ShowDetailView&TermToSearch=16459565&ordinalpos=3&itool=EntrezSystem2.PEntrez.Pubmed.Pubmed_ResultsPanel.Pubmed_RVDocSum>. | |||
Edited by James Cunningham a student of [mailto:ralarsen@ucsd.edu Rachel Larsen] and Kit Pogliano | Edited by James Cunningham a student of [mailto:ralarsen@ucsd.edu Rachel Larsen] and Kit Pogliano | ||
KMG | |||
Latest revision as of 19:01, 22 April 2011
A Microbial Biorealm page on the genus Shigella boydii
Classification
Higher order taxa
Bacteria (domain); Proteobacteria (phylum); Gamma Proteobacteria (class); Enterobacteriales (order); Enterobacteriaceae (family); Shigella (genus)
Species
Shigella boydii
|
NCBI: Taxonomy |
Description and significance
In the 1950's Shigella was accepted as a genus and subgrouped into four species: S. dysenteriae, S. fexneri, S. boydii, and S. sonnei (also referred to as subgroups A-D).[3]
Appearance: Shigella boydii is a bacillary (rod-shaped) gram-negative bacterium that does not form spores and is usually nonmotile.[2][5]
Habitat: S. boydii inhabits the intestine and rectum of humans and other primates. It can survive in feces and soil and/or food/water contaminated with fecal matter. For example, in Guadalajara, Mexico, Salmonella and Shigella species were found in freshly squeezed orange juice, oranges, and wiping cloths found in public markets and street booths. S. boydii was specifically found in the oranges and wiping cloths. This may indicate poor sanitary methods of food processing which led to raw sewage exposure.[13][14] Locationally, S. boydii is found mainly on the sub-continent of India.[3]
Significance: Human pathogen that causes bacillary dysentery.[4]
Serotypes: There are 20 S. boydii serotypes.[5]
Genetics: Shigella bacteria are thought to be derived from different strains of Escherichia coli. S. boydii is the most genetically divergent and some serotypes seem to be more closely related to other species. S. boydii type 13, for example, shares sequence similarities with Vibrio cholerae for the genes encoding the O antigen, the polysaccharide part of the lipopolysaccharide (LPS), and therefore these may be more closely related. LPS is an endotoxin and part of the Gram-negative outer membrane.[1]
Genome structure
Size of genome: Shigella boydii (Sb227) serotype 4- Circular DNA chromosome with 4,519,823 nt (446 genes); Plasmid (pSB4_227)- 126,697 nt (149 genes). Both were completed 2005/11/18. [11][12]
Pathogenic Contents: The one plasmid, pSb4_227, has post-segregation killing systems mvpA/mvpT, found in all Shigella species' plasmids and ccdA/ccdB not found in some.[3]
It is believed that most Shigella have gained and lost Stx genes at one time or another, the toxin genes found in S. dysenteriae. One evidence of this is Sb227 which has a T2SS pseudogene. T2SS, found in S. dysenteriae, enables export of toxins to host that would otherwise build up inside of the cell and cause lysis, therefore T2SS greatly contributes to pathogenicity. This inactivation of T2SS in S. boydii has most likely been naturally selected to better adapt to a human host as having greater pathogenicity offers little benefit for longterm survival.[3]
Sb227 contains pathogenic islands SHI-1, SHI-2 and ipaH (invasion plasmid antigen). Insertion (IS) element ISSbo6 is restricted in SHI-1, SHI-2 and ipaH pathogenic islands. This suggests that these islands were acquired before the IS-element.[3]
Iron Up-take: Iron is taken up from the environment by ABC transporters and by the iron transport compound aerobactin.[3]
Interesting Features: Shigella has a very large number of IS-elements which not only lead to rearrangement of DNA but also deletion. For example, the cell entry region, found in all Shigella virulence plasmids, and the icsA gene were deleted from pSB4_227. Also about 30kb that lie between icsA and ccdA in pCP301 (plasmid of S. flexneri 2a, strain 301) are missing.[3]
All Shigella species including most of S. boydii serotypes share about 3 Mb worth of genetic material with E. coli. This supports the idea that Shigella species diverged from the same origins as E. coli.[3]
Cell Structure and Metabolism
Cell Structure: Shigella's structural characteristics follow that of Gram-negative bacteria. Most research would agree that Shigella are nonmotile but some evidence suggests that they do in fact have flagella, although motility is not necessary for infection of intestine. The flagella tend to be on one pole of the cell and about 10 microns in length and 12-14nm in diameter. The genes coding for the flagella in S. dysenteriae, S. flexneri, S. boydii and S. sonnei were found to be different and attribute to the genetic diversity among the species.[8]
Metabolism: S. boydii, when found in the intestine, go though anaerobic metabolic pathways but can survive outside of the body due to its ability to utilize aerobic pathways.[14] More specifically, S. boydii, typically does not have oxidase enzymes but rather catalase enzymes (catalyzes the reduction of H2O2->H20). Methyl red testing is positive, meaning that the bacteria uses a mixed acid fermentation pathway. Voges–Proskauer and Simmons’ citrate reactions are negative, meaning that this organism does not utilize the butylene glycol pathway or produce acetoin. Lysine decarboxylase, arginine dihydrolase and ornithine decarboxylase are not present. S. boydii does not produce H2S, does not hydrolyze urea and does not grow in KCN broth. Carbohydrates are usually fermented and these include glucose (in the absence of gas production), D-mannitol, arabinose, trehalose and mannose.[7]
Ecology/Pathology
Shigella bacteria cause diarrhea and shigellosis (bacillary dysentery) through oral-fecal transmission. Shigella is a highly infective agent able to infect a host with less than 20 cells with an onset of about 12-48 hours, in favorable conditions. Once ingested, the Shigella makes its way through the gastrointestinal tract until it reaches the epithelial cells of the intestinal mucosa, there it infects, causing irritation, inflammation and necrosis (swelling and breaking of infected cells, which spreads infection). General symptoms include stomach cramps, high fever, mucus in feces, and bloody diarrhea due to ulceration of intestinal lining and rectum.
In most cases these symptoms are mild and resolve in about a week but other cases can become severe enough to be fatal without proper medical care. The elderly, very young and those weakened by disease are much more sensitive to the bacteria. In very young children very high fever may also be accompanied with seizures.[4] Usually Shigella bacteria are found in areas of poor sanitation. Food washed with contaminated water or not cleaned properly may also be a target. In 1998 an outbreak of Shigellosis occurred in Chicago due to Shigella boydii type 18 found on the cilantro and parsley in bean salad.[6]
Shigella species account for less than 10% of all foodborne illnesses reported in the United States. With an estimated 300,000 yearly incidents of shigellosis in the U.S., the exact percentage due to food contamination is unknown, due to the difficulty in isolating the bacteria from food but given its infectiousness the number is undoubtedly high.[2]
Current Research
1. Comparisons between Shigella species and between E. coli have been made and are being made in order to better understand Shigella's pathogenicity, patterns of infection, and varying harmfulness. Answers to these questions will hopefully lead to better avoidance and treatment of shigellosis in the future.[3]
2. At the National Shigella Reference Centre in Israel during the years 2000- 2004, 5,616 Shigella isolates were tested for resistance to certain antibacterial products. In one strain of Shigella boydii 2 and in two strains each of Shigella flexneri 2a, S. flexneri 6, and Shigella sonnei there was discovered resistance to ceftriaxone. All of these strains were found to be producers of extended-spectrum beta-lactamase (ESBL) and also very sensitive to tazobactam which inhibits the bacterial beta-lactamases. More research is needed to determine the rate of resistance to antibiotics and rate of transfer of resistant genes.[9]
3. At the French National Reference Centre for Escherichia coli and Shigella, from 2000- 2004, 4,198 Shigella isolates were obtained. 180 of those isolates, taken from patients infected with diarrhea and dysentery, did not respond to any available antisera (serum containing antibodies) that had been used on all known S. boydii serotypes. All of the isolates shared characteristics of S. boydii serotypes except that their rRNA genes were unique from all others. A new antiserum was manufactured and destroyed the new serotype S. boydii 20. 91 of the 180 patients had traveled internationally while infected therefore further studies must be done in order to determine the epidemiology of this serogroup and the its potentially widespread threat.[10]
References
1. Feng Lu, Sof'ya N. Senchenkova, Jinghua Yang, Alexander S. Shashkov, Jiang Tao, Hongjie Guo, Guang Zhao, Yuriy A. Knirel, Peter Reeves, and Lei Wang. "Structural and Genetic Characterization of the Shigella Boydii Type 13 O Antigen." J Bacteriol 186(2) (2004): 383-392. NCBI. PMID 14702307
2. "Shigella." U.S. Food and Drug Administration. 14 June 2006. Department of Health and Human Services. 30 Apr. 2007 <http://www.cfsan.fda.gov/~mow/chap19.html>.
3. Yang, Fan, Jian Yang, Xiaobing Zhang, and Yan Jiang. "Genome Dynamics and Diversity of Shigella Species, the Etiologic Agents of Bacillary Dysentery." Nucleic Acids Research 33 (2005): 6445-6458. Oxford Journals. <http://nar.oxfordjournals.org/cgi/content/abstract/33/19/6445?maxtoshow=&HITS=10&hits=10&RESULTFORMAT=&fulltext=shigella+boydii&searchid=1&FIRSTINDEX=0&resourcetype=HWCIT>.
4. "Shigellosis." CDC. 13 Oct. 2005. HHS. 1 May 2007 <http://www.cdc.gov/ncidod/dbmd/diseaseinfo/shigellosis_g.htm#What%20sort%20of%20germ%20is%20Shigella>.
5. Woodward, David L., Clifford G. Clark, Richard A. Caldeira, and Rafiq Ahmed. "Identification and Characterization of Shigella Boydii 20 Serovar Nov., a New and Emerging Shigella Serotype." Journal of Medical Microbiology 54 (2005): 741-748. Society of General Microbiology. <http://jmm.sgmjournals.org/cgi/content/abstract/54/8/741>.
6. Chan, Yc, and Hp Blaschek. "Comparative Analysis of Shigella Boydii 18 Foodborne Outbreak Isolate and Related Enteric Bacteria: Role of RpoS and AdiA in Acid Stress Response." NCBI 68 (2005): 521-7. NCBI. <http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?db=PubMed&cmd=Retrieve&list_uids=15771176&dopt=Citation>. PMID: 15771176
7. Holt, J. G., Krieg, N. R., Sneath, P. H. A., Staley, J. T. & Williams, S. T. (editors) (1994). Bergey’s Manual of Determinative Bacteriology, 9th edn. Baltimore, MD: Williams & Wilkins.
8. Ja, Giron. "Expression of Flagella and Motility by Shigella." Molecular Microbiology 18 (1995): 63-75. NCBI. <http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=8596461&dopt=Abstract>. PMID: 8596461
9. Vasilev, V, R Japheth, R Yishai, N Andorn, L Valinsky, S Navon-Venezia, I, Chmelnitsky, Y Carmeli, and D Cohen. "Extended-Spectrum Beta-Lactamase-Producing Shigella Strains in Israel, 2000-2004." European Journal of Clinical Microbiology and Infectious Diseases 26 (2007): 189-194. NCBI. <http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?db=pubmed&cmd=Retrieve&dopt=AbstractPlus&list_uids=17265070&query_hl=4&itool=pubmed_docsum>.
10. Grimont,Francine, Monique Lejay-Collin, Kaisar A. Talukder, Isabelle Carle, Sylvie Issenhuth, Karine Le Roux1 and Patrick A. D. Grimont. "Identification of a group of shigella-like isolates as Shigella boydii 20." Jounal of Medical Microbiology 56 (2007): 749-754. Society for General Microbiology. <http://jmm.sgmjournals.org/cgi/content/abstract/56/6/749>.
11. Entrez Genome. "S. boydii (serotype 4) Sb227, 4519823 bp." (2005). NC_007613 NCBI. <http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?db=genome&cmd=Retrieve&dopt=Overview&list_uids=19008>.
12. Entrez Genome. "S. boydii (serotype 4) Sb227 pSB4_227, 126697 bp" (2005). NC_007608 NCBI. <http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?db=genome&cmd=Retrieve&dopt=Overview&list_uids=19003>.
13. Castillo A, Villarruel-López A, Navarro-Hidalgo V, Martínez-González NE, Torres-Vitela MR. "Salmonella and Shigella in freshly squeezed orange juice, fresh oranges, and wiping cloths collected from public markets and street booths in Guadalajara, Mexico: incidence and comparison of analytical routes." Journal of Food Protection. 69 (11) (2006): 2595-2599. NCBI. <http://www.ncbi.nlm.nih.gov/sites/entrez?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids=17133801>.
14. Prema P, Palavesam A, Balaji P. "Aerobic heterotrophic bacterial diversity in sediments of Rajakkamangalam estuary, south west coast of India." Journal of Environmental Biology. 26 (4) (2005): 729-724. NCBI. <http://www.ncbi.nlm.nih.gov/sites/entrez?Db=pubmed&Cmd=ShowDetailView&TermToSearch=16459565&ordinalpos=3&itool=EntrezSystem2.PEntrez.Pubmed.Pubmed_ResultsPanel.Pubmed_RVDocSum>.
Edited by James Cunningham a student of Rachel Larsen and Kit Pogliano
KMG