Mycobacterium leprae*: Difference between revisions
No edit summary |
No edit summary |
||
| (37 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
{{Uncurated}} | |||
{{Biorealm Genus}} | {{Biorealm Genus}} | ||
| Line 14: | Line 15: | ||
|} | |} | ||
'' | ''Mycobacterium leprae'' | ||
==Description and | ==Description and Significance== | ||
[[Image: Leprogirl.jpg|thumb|300px|Child with leprosy (1)]] | |||
''Mycobacterium leprae'', also known as "Hansen's Bacillus", was discovered by Doctor Gerhard Armauer Hansen in 1873. Dr. Hansen discovered the bacteria in the nodules of leprosy patients and determined that it was the cause of the leprosy. The disease that M. leprae causes is referred to as leprosy or Hansen's Disease. Since M. leprae is the cause of leprosy it is pathogenic. Leprosy has been recorded as early as 600-400 B.C. Leprosy is found in countries world wide, but it is common in many countries with a tropical or sub-tropical climate such as Angola, Brazil, and India. In the United States, there are approximately 1000 cases reported and diagnosed each year. In 2004, according to the World Health Organization (WHO) there were an average of 150 cases of leprosy, with 69 new cases and 131 wide-spread cases. In 2005 the WHO reported that there were 286,063 new cases of leprosy worldwide. ''Mycobacterium leprae'' has two different forms in which it can express itself, Tuberculoid and Lepromatous. The difference between the two is that Tuberculoid is caused by a faster cellular response to the bacterium, causing disfigurement of the skin, sores, peripheral nerve damage, and progressive debilitation. Lepromatous is a slower cellular response large nodules and bumps on the skin. There are medicines today that can treat leprosy and kill the ''M. leprae''. Victims can choose to either take certain medicines as prescribe by the WHO or can get surgery to help prevent further deterioration. The medicines that are on the market for leprosy include Dapsone, Rifampicin, and Clofazimine. Surgery can be used to help increase motor function of the once infected areas as well as increase sensation in nerve degraded areas. Cosmetic surgery can be undertaken to remove excess skin as the result from having leprosy, eyebrow replacement, and nasal reconstruction in case of muscle loss. | |||
==Genome structure== | ==Genome structure== | ||
The M. leprae genome project was sequenced in 2001 by the Sanger Institute. The sequence was found by employing automated DNA sequence analysis of selected cosmids and whole-genome clones. After the completion of this, the genome sequence was found to contain 3,268,203 base pairs (bp), and to have an average of G&C (Guanine and Cytosine) content of 57.8%. However, compared to M. tuberculosis, which has 4,441,529 bp and 65.6% G&C, the numbers are much lower. M. leprae also contains about 1600 genes and more than 1100 pseudogenes, but again, this is relatively small compared to M. tuberculosis, which contains around 4000 genes. All of these smaller numbers in M. leprae suggest that there is massive decay in it; making it the most striking example of genome reduction in a microbial pathogen. | |||
==Cell structure, metabolism & life cycle== | ==Cell structure, metabolism & life cycle== | ||
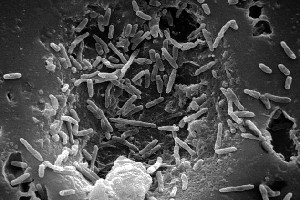
[[Image: Mycobacterium.jpg|thumb|300px|Scanning Electron Microscopy Image of M. leprae (2)]] | |||
M. leprae is a strong acid rod-shaped organism with parallel sides and rounded ends. It is also a gram-positive aerobic and is surrounded by a waxy coating which is unique to Mycobacterium. Because of this waxy coating it is known to have the largest doubling time of all known bacteria (27 hours). And because of this factor, every effort to culture this in the laboratory has proved non-successful. M. leprae is also known to have unique lipids that are linked together with covalent bonding. The waxy coating is created because of this bonding at room temperature. Adding this factor to the slow doubling time makes M. leprae very hard to fight against. The metabolism of M. leprae, that was thought to be self-reliant, has been greatly reduced due to the down-sizing of the genome. Many regulatory elements of metabolism, such as producing siderophores, which is a key part of the oxidative, microaerophilic and anaerobic chains, have been lost altogether. Due to all of this lost, M. leprae has become dependent on its host to receive nutrients and metabolites. It has evolved itself to a parasitic role. M.leprae is aerobic and auxotrophic meaning it requires a nutrient that the normal strain of ''Mycobacterium'' does not. These nutrients come from the host and is why it is parasitic. M. leprae's primary source for ATP is from the Krebs cycle. Ideal metabolism occurs at 33°C and a pH between 5.1 and 5.6. | |||
==Ecology (including pathogenesis)== | ==Ecology (including pathogenesis)== | ||
M. leprae can be typically found in water, soil, or in the air. In fact the DNA from M. leprae has been discovered in several soil samples that are prone to the disease leprosy. But even though it can be found in soil, M. leprae is very selective when picking its hosts. Its ideal conditions are around 27-30°C. Most mammals do not have a body temperature of 33°C, so only a few species are known to be carriers of M. leprae. When the disease does affect humans though, it is usually in the hands and feet because they are the coolest parts of the body. This environment is more suitable for M. leprae to live and thrive. | |||
==Interesting feature== | ==Interesting feature== | ||
===History of Leprosy=== | |||
Leprosy has been around humans since 1550 B.C. The ancient Egyptians were the first to record its presence on ancient papyrus scrolls. In 600 B.C. the ancient Indians also wrote about a disease similar to what we know as leprosy today. Historians believe that the disease was spread to Europe via Alexander The Great when he returned to Greece from a trip to India, and then it spread to Rome in 62 B.C. when the Pompeiin troops returned from Asia Minor. Many people believed that leprosy was in fact a punishment sent down by God. For this people with leprosy were shunned by the church. Even after leprosy was proven to be a biological disease, people were still shunned and stigmatized by the public. The bible mentions leprosy a total of 54 times. The bible compares leprosy to a sin, and it was a punishment from God for transgression; it is for this reason that people associated this disease as a punishment from God. Leprosy patients even had to wear special clothing and carry a bell to warn others that they had leprosy in Europe. Even today people with leprosy are treated at hospitals different from those normal patients are treated in. Leprosy has been so prevalent in various areas as certain times throughout history that is has inspired art work and influenced other cultural practices. | |||
====Leprosy Time Line from the 1900s:==== | |||
1921: U.S. Public Health Service established the Gillis W. Long Hansen’s Disease Center in Carville, Louisiana, which became known as “Carville.” It became a center of research and testing to find a cure for leprosy and a live-in treatment center for leprosy patients. | |||
[[Image: chaulmoogra.jpg|thumb|300px|A Chaulmoogra Nut, supposedly used to cure leprosy (3)]] | |||
1940s: Leprosy doctors all over the world treated patients by injecting them with oil from the chaulmoogra nut. This course of treatment was painful, and although some patients appeared to benefit, its long term efficacy was questionable. | |||
1941: Promin, a sulfone drug, was introduced as a treatment for leprosy. It was first identified and used at Carville. Promin successfully treated leprosy but unfortunately treatment with Promin required many painful injections. | |||
1950s: Dapsone pills, pioneered by Dr. R.G. Cochrane at Carville, became the treatment of choice for leprosy. Dapsone worked wonderfully at first, but unfortunately, M. leprae eventually began developing dapsone resistance. | |||
1970s: The first successful multi-drug treatment (MDT) regimen for leprosy was developed through drug trials on the island of Malta. | |||
1981: The World Health Organization began recommending MDT, a combination of three drugs: dapsone, rifampicin, and clofazimine. MDT with these drugs takes from six months to a year or even more, depending on stregnth of leprosy infection. | |||
Now: MDT with a combination of dapsone, rifampicin, and clofazimine is still the best treatment for preventing nerve damage, deformity, disability and further transmission. Researchers are working on developing a vaccine and ways to detect leprosy sooner in order to start treatment earlier. | |||
==References== | ==References== | ||
[ | 1) [http://www.who.int/lep/en/ "Leprosy Today." World Health Organization. World Health Organization. 10 Oct 2007] | ||
2) [http://www.ncbi.nlm.nih.gov/sites/entrez?Db=genomeprj&Cmd=Retrieve&list_uids=90 National Center for Biotechnology Information. ''Mycobacterium leprae TN'' Genome Project Result. 6 November 2007] | |||
3) [http://www.herbs2000.com/herbs/herbs_chaulmoogra.htm Herbs 2000. "Chaulmoogra" 5 December 2007] | |||
Brennan, J. T. Mycobacteria . In Encyclopedia of Microbiology (pp. | |||
312-327). a. | |||
[http://www.drugs.com/enc/leprosy.html Drugs.com Drug Information Online. (2007, August 17). October 2, 2007] | |||
Kazda, J. (2000). The Ecology of Mycobacteria. Kluwer Academic Publishers. | |||
[http://www.nlm.nih.gov/medlineplus/ency/article/003766.htm Medline Plus. (2007, September 19). October 1, 2007] | |||
[http://pathmicro.med.sc.edu/book/welcome.htm Microbiology, T. D. (2007, August 17). Microbiology and Immunology Online. September 29, 2007, from University of South Carolina School of Medicine] | |||
[http://microbewiki.kenyon.edu/index.php/Mycobacterium_leprae Mycobacterium Leprae. (2007, July 21). September 25, 2007] | |||
[http://www.who.int/mediacentre/factsheets/fs101/en/ WHO. (2007). Leprosy. September 30, 2007] | |||
[http://microbes.historique.net/leprae.html Infectious Disease. (2007). ''Mycobacterium leprae''. November 6, 2007] | |||
[http://www.itg.be/itg/DistanceLearning/LectureNotesVandenEndenE/22_Leprosyp4.htm Institute of Tropical Medicine Antwerp. (2007). 4 ''MYCOBACTERIUM LEPRAE''. November 6, 2007] | |||
[http://www.sanger.ac.uk/Projects/M_leprae/ The Welcome Trust Sanger Institute. (2007). Mycobacterium leprae Genome Project. November 6, 2007] | |||
[http://www.who.int/lep/microbiology/en/print.html World Health Organization. (2007). November 6, 2007] | |||
[http://www.who.int/tdr/research/progress/lep_afr/treatment.htm World Health Organization. Treatment of Leprosy. (2007). December 5, 2007] | |||
<b>Edited by the NC State University MB 103 class of 2007.</b> | <b>Edited by the NC State University MB 103 class of 2007.</b> | ||
<!-- Do not edit or remove this line --> [[Category:Pages edited by the NC State University MB 103 class of 2007]] | |||
Latest revision as of 20:08, 26 August 2010
A Microbial Biorealm page on the genus Mycobacterium leprae*
Classification
Higher order taxa
Bacteria; Actinobacteria; Actinobacteria; Actinobacteridae; Actinomycetale; Corynebacterineae; Mycobacteriaceae
Species
|
NCBI: Taxonomy |
Mycobacterium leprae
Description and Significance
Mycobacterium leprae, also known as "Hansen's Bacillus", was discovered by Doctor Gerhard Armauer Hansen in 1873. Dr. Hansen discovered the bacteria in the nodules of leprosy patients and determined that it was the cause of the leprosy. The disease that M. leprae causes is referred to as leprosy or Hansen's Disease. Since M. leprae is the cause of leprosy it is pathogenic. Leprosy has been recorded as early as 600-400 B.C. Leprosy is found in countries world wide, but it is common in many countries with a tropical or sub-tropical climate such as Angola, Brazil, and India. In the United States, there are approximately 1000 cases reported and diagnosed each year. In 2004, according to the World Health Organization (WHO) there were an average of 150 cases of leprosy, with 69 new cases and 131 wide-spread cases. In 2005 the WHO reported that there were 286,063 new cases of leprosy worldwide. Mycobacterium leprae has two different forms in which it can express itself, Tuberculoid and Lepromatous. The difference between the two is that Tuberculoid is caused by a faster cellular response to the bacterium, causing disfigurement of the skin, sores, peripheral nerve damage, and progressive debilitation. Lepromatous is a slower cellular response large nodules and bumps on the skin. There are medicines today that can treat leprosy and kill the M. leprae. Victims can choose to either take certain medicines as prescribe by the WHO or can get surgery to help prevent further deterioration. The medicines that are on the market for leprosy include Dapsone, Rifampicin, and Clofazimine. Surgery can be used to help increase motor function of the once infected areas as well as increase sensation in nerve degraded areas. Cosmetic surgery can be undertaken to remove excess skin as the result from having leprosy, eyebrow replacement, and nasal reconstruction in case of muscle loss.
Genome structure
The M. leprae genome project was sequenced in 2001 by the Sanger Institute. The sequence was found by employing automated DNA sequence analysis of selected cosmids and whole-genome clones. After the completion of this, the genome sequence was found to contain 3,268,203 base pairs (bp), and to have an average of G&C (Guanine and Cytosine) content of 57.8%. However, compared to M. tuberculosis, which has 4,441,529 bp and 65.6% G&C, the numbers are much lower. M. leprae also contains about 1600 genes and more than 1100 pseudogenes, but again, this is relatively small compared to M. tuberculosis, which contains around 4000 genes. All of these smaller numbers in M. leprae suggest that there is massive decay in it; making it the most striking example of genome reduction in a microbial pathogen.
Cell structure, metabolism & life cycle
M. leprae is a strong acid rod-shaped organism with parallel sides and rounded ends. It is also a gram-positive aerobic and is surrounded by a waxy coating which is unique to Mycobacterium. Because of this waxy coating it is known to have the largest doubling time of all known bacteria (27 hours). And because of this factor, every effort to culture this in the laboratory has proved non-successful. M. leprae is also known to have unique lipids that are linked together with covalent bonding. The waxy coating is created because of this bonding at room temperature. Adding this factor to the slow doubling time makes M. leprae very hard to fight against. The metabolism of M. leprae, that was thought to be self-reliant, has been greatly reduced due to the down-sizing of the genome. Many regulatory elements of metabolism, such as producing siderophores, which is a key part of the oxidative, microaerophilic and anaerobic chains, have been lost altogether. Due to all of this lost, M. leprae has become dependent on its host to receive nutrients and metabolites. It has evolved itself to a parasitic role. M.leprae is aerobic and auxotrophic meaning it requires a nutrient that the normal strain of Mycobacterium does not. These nutrients come from the host and is why it is parasitic. M. leprae's primary source for ATP is from the Krebs cycle. Ideal metabolism occurs at 33°C and a pH between 5.1 and 5.6.
Ecology (including pathogenesis)
M. leprae can be typically found in water, soil, or in the air. In fact the DNA from M. leprae has been discovered in several soil samples that are prone to the disease leprosy. But even though it can be found in soil, M. leprae is very selective when picking its hosts. Its ideal conditions are around 27-30°C. Most mammals do not have a body temperature of 33°C, so only a few species are known to be carriers of M. leprae. When the disease does affect humans though, it is usually in the hands and feet because they are the coolest parts of the body. This environment is more suitable for M. leprae to live and thrive.
Interesting feature
History of Leprosy
Leprosy has been around humans since 1550 B.C. The ancient Egyptians were the first to record its presence on ancient papyrus scrolls. In 600 B.C. the ancient Indians also wrote about a disease similar to what we know as leprosy today. Historians believe that the disease was spread to Europe via Alexander The Great when he returned to Greece from a trip to India, and then it spread to Rome in 62 B.C. when the Pompeiin troops returned from Asia Minor. Many people believed that leprosy was in fact a punishment sent down by God. For this people with leprosy were shunned by the church. Even after leprosy was proven to be a biological disease, people were still shunned and stigmatized by the public. The bible mentions leprosy a total of 54 times. The bible compares leprosy to a sin, and it was a punishment from God for transgression; it is for this reason that people associated this disease as a punishment from God. Leprosy patients even had to wear special clothing and carry a bell to warn others that they had leprosy in Europe. Even today people with leprosy are treated at hospitals different from those normal patients are treated in. Leprosy has been so prevalent in various areas as certain times throughout history that is has inspired art work and influenced other cultural practices.
Leprosy Time Line from the 1900s:
1921: U.S. Public Health Service established the Gillis W. Long Hansen’s Disease Center in Carville, Louisiana, which became known as “Carville.” It became a center of research and testing to find a cure for leprosy and a live-in treatment center for leprosy patients.
1940s: Leprosy doctors all over the world treated patients by injecting them with oil from the chaulmoogra nut. This course of treatment was painful, and although some patients appeared to benefit, its long term efficacy was questionable.
1941: Promin, a sulfone drug, was introduced as a treatment for leprosy. It was first identified and used at Carville. Promin successfully treated leprosy but unfortunately treatment with Promin required many painful injections.
1950s: Dapsone pills, pioneered by Dr. R.G. Cochrane at Carville, became the treatment of choice for leprosy. Dapsone worked wonderfully at first, but unfortunately, M. leprae eventually began developing dapsone resistance.
1970s: The first successful multi-drug treatment (MDT) regimen for leprosy was developed through drug trials on the island of Malta.
1981: The World Health Organization began recommending MDT, a combination of three drugs: dapsone, rifampicin, and clofazimine. MDT with these drugs takes from six months to a year or even more, depending on stregnth of leprosy infection.
Now: MDT with a combination of dapsone, rifampicin, and clofazimine is still the best treatment for preventing nerve damage, deformity, disability and further transmission. Researchers are working on developing a vaccine and ways to detect leprosy sooner in order to start treatment earlier.
References
1) "Leprosy Today." World Health Organization. World Health Organization. 10 Oct 2007
3) Herbs 2000. "Chaulmoogra" 5 December 2007
Brennan, J. T. Mycobacteria . In Encyclopedia of Microbiology (pp. 312-327). a.
Drugs.com Drug Information Online. (2007, August 17). October 2, 2007
Kazda, J. (2000). The Ecology of Mycobacteria. Kluwer Academic Publishers.
Medline Plus. (2007, September 19). October 1, 2007
Mycobacterium Leprae. (2007, July 21). September 25, 2007
WHO. (2007). Leprosy. September 30, 2007
Infectious Disease. (2007). Mycobacterium leprae. November 6, 2007
Institute of Tropical Medicine Antwerp. (2007). 4 MYCOBACTERIUM LEPRAE. November 6, 2007
The Welcome Trust Sanger Institute. (2007). Mycobacterium leprae Genome Project. November 6, 2007
World Health Organization. (2007). November 6, 2007
World Health Organization. Treatment of Leprosy. (2007). December 5, 2007
Edited by the NC State University MB 103 class of 2007.