Tuberculosis in Russian Prisons: Difference between revisions
No edit summary |
|||
| (99 intermediate revisions by one other user not shown) | |||
| Line 1: | Line 1: | ||
{{Curated}} | |||
==Introduction== | ==Introduction== | ||
<br> | <br> Edited by: Christopher Murphy<br> | ||
<br>Mycobacterium tuberculosis | <br>Mycobacterium tuberculosis is considered one of the most deadly infectious diseases. Russia, particularly in its prisons, has experienced the burden of TB. Prisoners are not the only ones that need to be concerned, tuberculosis can spread to the rest of society via released prisoners and prison and hospital workers.[1] Although the current conditions in Russia are not favorable efforts are being made to reduce the gravity of tuberculosis. The condition of tuberculosis is a major public health concern for not only Russia but for the entire world as globalization interconnects countries more and more.<br> | ||
<br>TB spreads person to person via aerosol transmission when an infected person sneezes, coughs or talks. The bacteria can last in the air for days and can travel great distances, making the disease extremely tenacious. For a successful infection, at least 10 cells of the bacteria need to reach the lungs' alveoli. The lungs provide a conducive environment for infection, TB is aerobic and needs a high concentration of oxygen to survive. In a year's time a person with tuberculosis can infect 10-15 people. Tuberculosis has several stages of development. Latent tuberculosis indicates the existence of bacteria in the body but the bacteria has been suppressed by the immune system. If the immune system becomes compromised active(susceptible) tuberculosis develops. If treated improperly a relatively mild case can become multi-drug resistant (MDR) and/or extensively drug resistant(XDR). Multidrug resistant tuberculosis is resistant to first line drugs. Therefore, more powerful and more expensive second line drugs are needed. Extensively drug resistant tuberculosis is essentially impossible to treat.[2]<br> | |||
<br> | <br>Humans have suffered heavily from this disease throughout history. During the "White Plague" in Europe of 17th and 18th centuries, tuberculosis was responsible for 25% of adult deaths and few people escaped infection. Over time tuberculosis began to disappear with the improvement of living conditions and the development of antibiotics. Yet today roughly 33% percent of the world's population has latent tuberculosis. The advent of tuberculosis was underscored by the World Health Organization's 1993 global emergency declaration concerning tuberculosis. This was in part due to a rise in multidrug resistant TB as well as an increased number of AIDS cases.[2] <br> | ||
==Why Tuberculosis is so prevalent in Russia== | ==Why Tuberculosis is so prevalent in Russia== | ||
<br> Tuberculosis is an opportunistic infection, | <br> Tuberculosis is an opportunistic infection, exploiting compromised immune systems. Factors that compromise immune systems are prevalent in Russia and its prisons, stressful and impoverished environments. Such factors include: large populations, inadequate nutrition, constant stress, poor living conditions, the use of intravenous drugs, alcoholism and co-infections(HIV/AIDS). Severe penal codes and lack of funds have exacerbated these conditions. Penal codes are so severe that the theft of a cell phone resulted in a prison sentence. Little has been done to improve the conditions in prisons, due to the stigma towards prisoners. The quarantine of prisoners is less than ideal, the infected prisoners are housed together causing re-infection.[1] This stigma is further highlighted by the fact that prisoners' cases weren't included in official statistics until 1995.[8]<br> | ||
[[Image:prison.jpg|thumb|350px|right| Figure 1. The bleak conditions in prison are shown in this picture. Source: Scientific American[1]]] | |||
<br>It was not until the 1990s that TB became a real concern for Russia. One factor was the collapse of infrastructure in Russia after the fall of the Soviet Union. Between 1991 and 1999 TB increased 7.5% each year.[8] The other factor was the release of sick prisoners, inadequately treated for TB, back into society. As a result of the collapse of Russian infrastructure the rates of alcoholism, unemployment, crime, incarceration and movement in and out of prison all increased significantly. Furthermore, health and social services stopped exacerbating the problem. Diagnostic tests could not be afforded any more nor could microscopes for sputum examination be afforded. Consequently, much of the treatment was ended prematurely.[1]<br> | |||
<br>It is likely that when the prison populations increased in the 1990s many of the new inmates were TB carriers. Moreover, a large amount of people was quickly crowded together in extremely uncleanly conditions, contributing to a uniquely high stress level. Prisoners' immune systems could no longer suppress the latent infection causing widespread transmission.[1] <br> | |||
<br>The prisoners face very high risks of contraction. Prisoners are 58 times likelier to contract tuberculosis than the average Russian citizen and are 28 times likelier to die from the disease.[1] In 2004 prisoners accounted for 12% of Russia's TB cases; in 2005 it had reached 27%.[8] As of 1999, the Russian prison population neared 1.1 million prisoners, in which 1 in 11 prisoners had tuberculosis. As a consequence of sporadic treatment MDR strains have arisen affecting 20,000 prisoners.[1]<br> | |||
<br>Russian prisons are considered "epidemiological pumps" for the rest of Russian society. Prisoners return home to equally small apartment blocs. These unventilated apartments serve as breeding grounds for TB during wintertime. Additionally, there is the risk of prison and hospital workers will becoming infected and transmitting the disease to the rest of society. Figure 1. exemplifies the conditions in Russian prisons. Prisoners, separated from nurses by iron bars, line up for inoculation. This intentional distance amplifies both the fear and risk of contracting TB.[1]<br> | |||
<br> | |||
==Attempts of Fighting off Tuberculosis== | ==Attempts of Fighting off Tuberculosis== | ||
<br>Russia continued to struggle with | ===History=== | ||
<br>Due to the lack of funds Russia has continued to struggle with tuberculosis until recently. Russia had previously its satellites to produce antibiotics but with the collapse drugs and funding were both in short supply. The newly independent satellite republics no longer continued the barter trade with Russia for antibiotics. In the late 1990s George Soros became a key benefactor to the treatment of tuberculosis. In addition, Medical Emergency Relief International and Partners in Health have done work in Russia to develop a new TB program which has alleviated some of the disease.[1]<br> | |||
<br> | <br>Russia has also heavily relied on the Eli Lilly and Company Foundation and the Global Fund to Fight AIDS, TB and Malaria. The creation of the Green Light Committee, a drug procurement consortium, has been crucial to the fight against Tuberculosis. Green Light Committee is comprised of WHO, U.S. CDC, ngos and pharmaceutical firms. The effectiveness of this program is highlighted by the drop in cost of patient care. Previously, treatment cost $10,000 to $15,000 and currently runs around $3,000 to $4,000. Through this committee countries such as Russia can afford medication, including the more expensive second line drugs to treat MDR-TB. This was the direct consequence of purchase contracts and subsidies. The general condition of hospitals has improved with increased funding from organizations such as Global Fund to Fight AIDS, TB and Malaria. Improvements include new lab equipment such as airtight closets to house sputum and technology for culturing. The handling of cases has also changed for the better, those with TB are sent back to the barracks while MDR-TB prisoners are isolated in the hospitals, 6 to 8 prisoners to a room. The goal of the international organizations is to counsel, help develop an infrastructure and empower Russia to be self-reliant.[1]<br> | ||
<br>Russia first started using DOTS in 1994;however, it was not until 1999 that the strategy proved useful. Moreover, in the time between 1994 and 1999, WHO and Russian officials to agree on a strategy that used DOTS along with radiology, microscopy and culture examination. By 2004, the cooperation had proven so effective that 37 regions in Russia were covered by DOTS which accounts for 45% of the country's population. One region in particular that has seen improvement is Tomsk, Russia. This region has been the test site for many of Merlin(UK) and the Public Health Research Institute's(US) work.[8]<br> | |||
<br>The are additional examples of success in the region in the fight against tuberculosis. The federal government has proved itself committed to the issue through its laws and regulations. WHO works along with the Russian Ministry of Justice to focus on AIDS and MDR-TB. One law passed in 2001 mandates that TB detection and treatment be free of charge. This measure has only been successfully implemented in prisons. The prison systems have also benefited in that by 2005 37 hospitals and 57 facilities were functional to take care of tuberculosis in the penal system.[8]<br> | |||
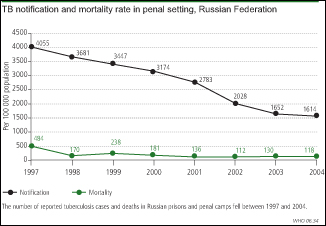
<br>Figure 2 illustrates the success of treatment, particularly DOTS, as the tuberculosis prevalence has decreased in prisons over time. Both the notification of TB cases and the consequent deaths have fallen.[8]<br> | |||
[[Image:Tb_graphlrg.jpg|thumb|350px|right| Figure 2. Graph showing the decrease in the number of cases of tuberculosis for prisons. Source:World Health Organization[8]]] | |||
<br> | ===DOTS Strategy=== | ||
<br> | <br>The DOTS program is usually the strategy of choice. A daily procedure involving 4 antibiotics for 6 to 9 months under the care of a health official. The treatment is lengthy because tuberculosis is slow growing, only reproducing once a day. It was first believed in the 1940s that the drug streptomycin was the cure. However, it was discovered that tuberculosis mutates and that multiple drugs were necessary. The drugs attack the tuberculosis in several different places simultaneously.[2]<br> | ||
<br>One new idea of treatment is to direct more attention to MDR-TB than susceptible TB. The strategy is used by Russia and many of its former satellite republics. It is hoped that this method will begin to be adopted by other countries around the world as well as help reach the 2015 goal of cutting the TB's global prevalence and mortality in half. Partners in Health developed this technique called DOTS Plus, in which all MDR-TB cases are treated. Local doctors were encouraged first in the prison system and then all throughout the region. This program takes up to two years and requires 6 to 8 drugs. MDR-TB and TB are similar in their capability to be lethal, the main difference is that MDR-TB is much harder to treat than TB. There is more and more agreement that MDR-TB should be the form of TB to be concentrated on because in treating MDR-TB then TB will also be treated.[1]<br> | |||
[[Image:Bed day.jpeg|thumb|200px|left| Figure 3. Graph showing decline in average bed occupancy for tuberculosis. Source: Oxford Journal[7]]] | |||
<br>Successful recovery from tuberculosis relies on full completion of the treatment. Full completion may not occur for two reasons. During the beginning months the majority of the tuberculosis bacteria is killed and the symptoms go away. Many patients stop treatment with the belief that they are cured. However, some tuberculosis survives, makes a waxy coat and buries away in the lung.[2] The surviving bacteria contain mutant strains that are resistant to the drugs. These strains take over causing the tuberculosis to be more virulent when treatment is ended prematurely. Another reason for incomplete treatment is the risk of adverse side affects. Such side effects include: hallucinations, nightmares and vomiting.[1]<br> | |||
<br>Figure 3. shows average number of days an adult TB patient spent in the hospital. The information was collected from 89 regions in Russia, the regions that used DOTS are darkened. In the year 2001, the average patient was likely to stay 86 days, the range was from 53 days to 132 days. The regions using DOTS tend to have lower hospital durations than non-DOTS regions proving the usefulness of DOTS.[7]<br> | |||
==Tuberculosis Studies== | ==Tuberculosis Studies== | ||
===Introduction=== | |||
<br> | <br>Many studies have been conducted in Russia in attempt to further understand the issue to effectively address the situation. The following studies each highlight a different aspect of the tuberculosis dilemma in Russia.<br> | ||
<br> | ===Study 1=== | ||
<br>In the study "Rates of latent tuberculosis in health care staff in Russia" the goal was to find individuals with latent tuberculosis infections and the rates of infection to treat through chemo prophylaxis and cross-infection strategies. In a cross sectional study, risk of tb was compared between unexposed students, medical students, primary health care providers and TB hospital health providers. Results showed that the amount of exposure could be linked to the likelihood of having LTBI. Primary health care providers were more likely to have TB than students and TB hospital health providers were more likely to have TB than the primary health care providers. In addition, TB laboratory workers also had high levels of tuberculosis. | <br>Some of the most convincing evidence of the general risk factors of Tuberculosis and varying importance in Russia comes from the study "Risk factors for pulmonary tuberculosis in Russia: case-control". The study was a case-control study in which existing cases of a medical condition are compared with a control group of the same number and similar composition. The goal of the study was to find and rank the risk factors for pulmonary tuberculosis. The leading risk factors were low accumulated wealth, financial insecurity, consumption of unpasteurized milk, diabetes, living with a relative with tuberculosis, unemployment, overcrowded living conditions, illicit drug use and incarceration. Of these leading risk factors when considering the amount of exposure, consumption of unpasteurized milk and unemployment.[3]<br> | ||
===Study 2=== | |||
<br>In the study "Rates of latent tuberculosis in health care staff in Russia" the goal was to find individuals with latent tuberculosis infections and the rates of infection to treat through chemo prophylaxis and cross-infection strategies. In a cross sectional study, risk of tb was compared between unexposed students, medical students, primary health care providers and TB hospital health providers. Results showed that the amount of exposure could be linked to the likelihood of having LTBI. Primary health care providers were more likely to have TB(39.1% or 90/230) than students (8.7% or 32/368) and TB hospital health providers (46.9% or 45/96) were more likely to have TB than the primary health care providers (29.3% or 34/115). In addition, TB laboratory workers also had high levels of tuberculosis (61.1% or 11/18). From the results it can be concluded that TB Health Care Workers are have the highest risk and precautionary measures need to be taken.[5]<br> | |||
===Study 3=== | |||
<br>A major concern for using second line drugs to treat MDR Tuberculosis is that many of them cause adverse reactions because of their toxicity. Through a retrospective case series "Adverse Reactions among patients being treated for MDR-TB in Tomsk, Russia" explored this question. Of the 244 cases 76% were cured, 6.6 % failed, 4.9 % died and 11.5 % defaulted. 73.3% of all cases showed adverse reactions, 74.8% in patients that adhered (at minimum took 80% of prescribed doses) and 59.1% of those that did not adhere. It was found that these adverse reactions varied on the amount of drugs taken but had no effect on the outcome. [4] <br> | |||
===Study 4=== | |||
<br>The study "Barriers to successful tuberculosis treatment in Tomsk, Russian Federation: non-adherence, default and the acquisition of multidrug resistance" found substance abuse to be the main barrier. Substance abuse was linked to non-adherence and defaulting and thus poor outcomes. However, MDR-TB strain development was not linked to substance abuse. MDR-TB was more likely to be found in patients that had been hospitalized than in patients receiving outpatient care. The study concluded that substance abuse, mainly alcohol, needs to be addressed by public health officials. The study also concluded that the MDR-TB increase needs to be investigated.[6]<br> | |||
===Summary of Studies=== | |||
<br> | <br>Each of these studies addresses a specific concern regarding tuberculosis. The first study outlined the general risk factors for tuberculosis. In the second study, the risk of contracting tuberculosis for health care workers is examined. The third study investigates the question of whether or not second line drugs inherent qualities jeopardize the success of a patient's outcome. The fourth study examines potential barriers to successful treatment.<br> | ||
==Conclusion== | ==Conclusion== | ||
<br> | <br>There has been success in treating tuberculosis in Russia, a direct result of DOTS. The Russian government is committed to improving the situation. More laws, regulations and money have all helped to mitigate the situation. However, because prisoners are at a higher risk for TB than other demographics they need to continue to be the focus of the government's efforts. With international help along with internal effort, Russia will begin to be able to eradicate tuberculosis and improve its standard of living. In the mean time great care must be taken with the DOTS procedure and health care personnel exposure so that tuberculosis in Russia will remain under control.<br> | ||
==References== | ==References== | ||
[ | <br>[1] ["Multidrug Resistant Tuberculosis in Russia". www.scientificamerican.com/report.cfm?id=tuberculosis-in-russia. 5 Dec. 2009]<br> | ||
<br>[2] ["Tuberculosis-can the spread of this killer disease be halted?". Microbes and Diseases Fact file 1]<br> | |||
<br>[3] [Richard Coker, Martin McKee, Rifat Atun, Boika Dimitrova, Ekaterina Dodonova, Sergei Kuznetsov, and Francis Drobniewski | |||
Risk factors for pulmonary tuberculosis in Russia: case-control study | |||
BMJ, Jan 2006; 332: 85 - 87. ]<br> | |||
<br>[4] [Adverse reactions among patients being treated for MDR-TB in Tomsk, Russia. | |||
S. S. Shin, A. D. Pasechnikov, I. Y. Gelmanova, G. G. Peremitin, A. K. Strelis, S. Mishustin, A. Barnashov, Y. Karpeichik, Y. G. Andreev, V. T. Golubchikova, T. P. Tonkel, G. V. Yanova, A. Yedilbayev, M. L. Rich, J. S. Mukherjee, J. J. Furin, S. Atwood, P. E. Farmer, and S. Keshavjee | |||
Int J Tuberc Lung Dis. 2007 December; 11(12): 1314–1320.]<br> | |||
<br>[5] [Rates of Latent Tuberculosis in Health Care Staff in Russia | |||
Francis Drobniewski, Yanina Balabanova, Elena Zakamova, Vladyslav Nikolayevskyy, and Ivan Fedorin | |||
PLoS Med. 2007 February; 4(2): e55. Published online 2007 February 13. doi: 10.1371/journal.pmed.0040055. | |||
PMCID: PMC1796908]<br> | |||
<br>[6]["Barriers to successful tuberculosis treatment in Tomsk, Russian Federation: non-adherence, default and the acquisition of multidrug resistance". http://www.who.int/bulletin/volumes/85/9/06-038331-ab/en/index.html. 5 Dec. 2009]<br> | |||
<br>[7][Eur J Public Health. 2007 Feb;17(1):98-103. Epub 2006 Jul 12. | |||
Reform of tuberculosis control and DOTS within Russian public health systems: an ecological study. | |||
Marx FM, Atun RA, Jakubowiak W, McKee M, Coker RJ. | |||
Department of Public Health and Policy, London School of Hygiene and Tropical Medicine Keppel Street, London, UK.]<br> | |||
<br>[8]["Tough measures in Russian prisons slow spread of TB". http://www.who.int/bulletin/volumes/84/4/news30406/en/index.html. 5 Dec. 2009]<br> | |||
Edited by student of [mailto:slonczewski@kenyon.edu Joan Slonczewski] for [http://biology.kenyon.edu/courses/BIOL191_09/BIOL_191_Global_Health_Syllabus.htm BIOL 191 Microbiology], 2009, [http://www.kenyon.edu/index.xml Kenyon College]. | Edited by student of [mailto:slonczewski@kenyon.edu Joan Slonczewski] for [http://biology.kenyon.edu/courses/BIOL191_09/BIOL_191_Global_Health_Syllabus.htm BIOL 191 Microbiology], 2009, [http://www.kenyon.edu/index.xml Kenyon College]. | ||
Latest revision as of 19:55, 11 August 2010
Introduction
Edited by: Christopher Murphy
Mycobacterium tuberculosis is considered one of the most deadly infectious diseases. Russia, particularly in its prisons, has experienced the burden of TB. Prisoners are not the only ones that need to be concerned, tuberculosis can spread to the rest of society via released prisoners and prison and hospital workers.[1] Although the current conditions in Russia are not favorable efforts are being made to reduce the gravity of tuberculosis. The condition of tuberculosis is a major public health concern for not only Russia but for the entire world as globalization interconnects countries more and more.
TB spreads person to person via aerosol transmission when an infected person sneezes, coughs or talks. The bacteria can last in the air for days and can travel great distances, making the disease extremely tenacious. For a successful infection, at least 10 cells of the bacteria need to reach the lungs' alveoli. The lungs provide a conducive environment for infection, TB is aerobic and needs a high concentration of oxygen to survive. In a year's time a person with tuberculosis can infect 10-15 people. Tuberculosis has several stages of development. Latent tuberculosis indicates the existence of bacteria in the body but the bacteria has been suppressed by the immune system. If the immune system becomes compromised active(susceptible) tuberculosis develops. If treated improperly a relatively mild case can become multi-drug resistant (MDR) and/or extensively drug resistant(XDR). Multidrug resistant tuberculosis is resistant to first line drugs. Therefore, more powerful and more expensive second line drugs are needed. Extensively drug resistant tuberculosis is essentially impossible to treat.[2]
Humans have suffered heavily from this disease throughout history. During the "White Plague" in Europe of 17th and 18th centuries, tuberculosis was responsible for 25% of adult deaths and few people escaped infection. Over time tuberculosis began to disappear with the improvement of living conditions and the development of antibiotics. Yet today roughly 33% percent of the world's population has latent tuberculosis. The advent of tuberculosis was underscored by the World Health Organization's 1993 global emergency declaration concerning tuberculosis. This was in part due to a rise in multidrug resistant TB as well as an increased number of AIDS cases.[2]
Why Tuberculosis is so prevalent in Russia
Tuberculosis is an opportunistic infection, exploiting compromised immune systems. Factors that compromise immune systems are prevalent in Russia and its prisons, stressful and impoverished environments. Such factors include: large populations, inadequate nutrition, constant stress, poor living conditions, the use of intravenous drugs, alcoholism and co-infections(HIV/AIDS). Severe penal codes and lack of funds have exacerbated these conditions. Penal codes are so severe that the theft of a cell phone resulted in a prison sentence. Little has been done to improve the conditions in prisons, due to the stigma towards prisoners. The quarantine of prisoners is less than ideal, the infected prisoners are housed together causing re-infection.[1] This stigma is further highlighted by the fact that prisoners' cases weren't included in official statistics until 1995.[8]
It was not until the 1990s that TB became a real concern for Russia. One factor was the collapse of infrastructure in Russia after the fall of the Soviet Union. Between 1991 and 1999 TB increased 7.5% each year.[8] The other factor was the release of sick prisoners, inadequately treated for TB, back into society. As a result of the collapse of Russian infrastructure the rates of alcoholism, unemployment, crime, incarceration and movement in and out of prison all increased significantly. Furthermore, health and social services stopped exacerbating the problem. Diagnostic tests could not be afforded any more nor could microscopes for sputum examination be afforded. Consequently, much of the treatment was ended prematurely.[1]
It is likely that when the prison populations increased in the 1990s many of the new inmates were TB carriers. Moreover, a large amount of people was quickly crowded together in extremely uncleanly conditions, contributing to a uniquely high stress level. Prisoners' immune systems could no longer suppress the latent infection causing widespread transmission.[1]
The prisoners face very high risks of contraction. Prisoners are 58 times likelier to contract tuberculosis than the average Russian citizen and are 28 times likelier to die from the disease.[1] In 2004 prisoners accounted for 12% of Russia's TB cases; in 2005 it had reached 27%.[8] As of 1999, the Russian prison population neared 1.1 million prisoners, in which 1 in 11 prisoners had tuberculosis. As a consequence of sporadic treatment MDR strains have arisen affecting 20,000 prisoners.[1]
Russian prisons are considered "epidemiological pumps" for the rest of Russian society. Prisoners return home to equally small apartment blocs. These unventilated apartments serve as breeding grounds for TB during wintertime. Additionally, there is the risk of prison and hospital workers will becoming infected and transmitting the disease to the rest of society. Figure 1. exemplifies the conditions in Russian prisons. Prisoners, separated from nurses by iron bars, line up for inoculation. This intentional distance amplifies both the fear and risk of contracting TB.[1]
Attempts of Fighting off Tuberculosis
History
Due to the lack of funds Russia has continued to struggle with tuberculosis until recently. Russia had previously its satellites to produce antibiotics but with the collapse drugs and funding were both in short supply. The newly independent satellite republics no longer continued the barter trade with Russia for antibiotics. In the late 1990s George Soros became a key benefactor to the treatment of tuberculosis. In addition, Medical Emergency Relief International and Partners in Health have done work in Russia to develop a new TB program which has alleviated some of the disease.[1]
Russia has also heavily relied on the Eli Lilly and Company Foundation and the Global Fund to Fight AIDS, TB and Malaria. The creation of the Green Light Committee, a drug procurement consortium, has been crucial to the fight against Tuberculosis. Green Light Committee is comprised of WHO, U.S. CDC, ngos and pharmaceutical firms. The effectiveness of this program is highlighted by the drop in cost of patient care. Previously, treatment cost $10,000 to $15,000 and currently runs around $3,000 to $4,000. Through this committee countries such as Russia can afford medication, including the more expensive second line drugs to treat MDR-TB. This was the direct consequence of purchase contracts and subsidies. The general condition of hospitals has improved with increased funding from organizations such as Global Fund to Fight AIDS, TB and Malaria. Improvements include new lab equipment such as airtight closets to house sputum and technology for culturing. The handling of cases has also changed for the better, those with TB are sent back to the barracks while MDR-TB prisoners are isolated in the hospitals, 6 to 8 prisoners to a room. The goal of the international organizations is to counsel, help develop an infrastructure and empower Russia to be self-reliant.[1]
Russia first started using DOTS in 1994;however, it was not until 1999 that the strategy proved useful. Moreover, in the time between 1994 and 1999, WHO and Russian officials to agree on a strategy that used DOTS along with radiology, microscopy and culture examination. By 2004, the cooperation had proven so effective that 37 regions in Russia were covered by DOTS which accounts for 45% of the country's population. One region in particular that has seen improvement is Tomsk, Russia. This region has been the test site for many of Merlin(UK) and the Public Health Research Institute's(US) work.[8]
The are additional examples of success in the region in the fight against tuberculosis. The federal government has proved itself committed to the issue through its laws and regulations. WHO works along with the Russian Ministry of Justice to focus on AIDS and MDR-TB. One law passed in 2001 mandates that TB detection and treatment be free of charge. This measure has only been successfully implemented in prisons. The prison systems have also benefited in that by 2005 37 hospitals and 57 facilities were functional to take care of tuberculosis in the penal system.[8]
Figure 2 illustrates the success of treatment, particularly DOTS, as the tuberculosis prevalence has decreased in prisons over time. Both the notification of TB cases and the consequent deaths have fallen.[8]
DOTS Strategy
The DOTS program is usually the strategy of choice. A daily procedure involving 4 antibiotics for 6 to 9 months under the care of a health official. The treatment is lengthy because tuberculosis is slow growing, only reproducing once a day. It was first believed in the 1940s that the drug streptomycin was the cure. However, it was discovered that tuberculosis mutates and that multiple drugs were necessary. The drugs attack the tuberculosis in several different places simultaneously.[2]
One new idea of treatment is to direct more attention to MDR-TB than susceptible TB. The strategy is used by Russia and many of its former satellite republics. It is hoped that this method will begin to be adopted by other countries around the world as well as help reach the 2015 goal of cutting the TB's global prevalence and mortality in half. Partners in Health developed this technique called DOTS Plus, in which all MDR-TB cases are treated. Local doctors were encouraged first in the prison system and then all throughout the region. This program takes up to two years and requires 6 to 8 drugs. MDR-TB and TB are similar in their capability to be lethal, the main difference is that MDR-TB is much harder to treat than TB. There is more and more agreement that MDR-TB should be the form of TB to be concentrated on because in treating MDR-TB then TB will also be treated.[1]
Successful recovery from tuberculosis relies on full completion of the treatment. Full completion may not occur for two reasons. During the beginning months the majority of the tuberculosis bacteria is killed and the symptoms go away. Many patients stop treatment with the belief that they are cured. However, some tuberculosis survives, makes a waxy coat and buries away in the lung.[2] The surviving bacteria contain mutant strains that are resistant to the drugs. These strains take over causing the tuberculosis to be more virulent when treatment is ended prematurely. Another reason for incomplete treatment is the risk of adverse side affects. Such side effects include: hallucinations, nightmares and vomiting.[1]
Figure 3. shows average number of days an adult TB patient spent in the hospital. The information was collected from 89 regions in Russia, the regions that used DOTS are darkened. In the year 2001, the average patient was likely to stay 86 days, the range was from 53 days to 132 days. The regions using DOTS tend to have lower hospital durations than non-DOTS regions proving the usefulness of DOTS.[7]
Tuberculosis Studies
Introduction
Many studies have been conducted in Russia in attempt to further understand the issue to effectively address the situation. The following studies each highlight a different aspect of the tuberculosis dilemma in Russia.
Study 1
Some of the most convincing evidence of the general risk factors of Tuberculosis and varying importance in Russia comes from the study "Risk factors for pulmonary tuberculosis in Russia: case-control". The study was a case-control study in which existing cases of a medical condition are compared with a control group of the same number and similar composition. The goal of the study was to find and rank the risk factors for pulmonary tuberculosis. The leading risk factors were low accumulated wealth, financial insecurity, consumption of unpasteurized milk, diabetes, living with a relative with tuberculosis, unemployment, overcrowded living conditions, illicit drug use and incarceration. Of these leading risk factors when considering the amount of exposure, consumption of unpasteurized milk and unemployment.[3]
Study 2
In the study "Rates of latent tuberculosis in health care staff in Russia" the goal was to find individuals with latent tuberculosis infections and the rates of infection to treat through chemo prophylaxis and cross-infection strategies. In a cross sectional study, risk of tb was compared between unexposed students, medical students, primary health care providers and TB hospital health providers. Results showed that the amount of exposure could be linked to the likelihood of having LTBI. Primary health care providers were more likely to have TB(39.1% or 90/230) than students (8.7% or 32/368) and TB hospital health providers (46.9% or 45/96) were more likely to have TB than the primary health care providers (29.3% or 34/115). In addition, TB laboratory workers also had high levels of tuberculosis (61.1% or 11/18). From the results it can be concluded that TB Health Care Workers are have the highest risk and precautionary measures need to be taken.[5]
Study 3
A major concern for using second line drugs to treat MDR Tuberculosis is that many of them cause adverse reactions because of their toxicity. Through a retrospective case series "Adverse Reactions among patients being treated for MDR-TB in Tomsk, Russia" explored this question. Of the 244 cases 76% were cured, 6.6 % failed, 4.9 % died and 11.5 % defaulted. 73.3% of all cases showed adverse reactions, 74.8% in patients that adhered (at minimum took 80% of prescribed doses) and 59.1% of those that did not adhere. It was found that these adverse reactions varied on the amount of drugs taken but had no effect on the outcome. [4]
Study 4
The study "Barriers to successful tuberculosis treatment in Tomsk, Russian Federation: non-adherence, default and the acquisition of multidrug resistance" found substance abuse to be the main barrier. Substance abuse was linked to non-adherence and defaulting and thus poor outcomes. However, MDR-TB strain development was not linked to substance abuse. MDR-TB was more likely to be found in patients that had been hospitalized than in patients receiving outpatient care. The study concluded that substance abuse, mainly alcohol, needs to be addressed by public health officials. The study also concluded that the MDR-TB increase needs to be investigated.[6]
Summary of Studies
Each of these studies addresses a specific concern regarding tuberculosis. The first study outlined the general risk factors for tuberculosis. In the second study, the risk of contracting tuberculosis for health care workers is examined. The third study investigates the question of whether or not second line drugs inherent qualities jeopardize the success of a patient's outcome. The fourth study examines potential barriers to successful treatment.
Conclusion
There has been success in treating tuberculosis in Russia, a direct result of DOTS. The Russian government is committed to improving the situation. More laws, regulations and money have all helped to mitigate the situation. However, because prisoners are at a higher risk for TB than other demographics they need to continue to be the focus of the government's efforts. With international help along with internal effort, Russia will begin to be able to eradicate tuberculosis and improve its standard of living. In the mean time great care must be taken with the DOTS procedure and health care personnel exposure so that tuberculosis in Russia will remain under control.
References
[1] ["Multidrug Resistant Tuberculosis in Russia". www.scientificamerican.com/report.cfm?id=tuberculosis-in-russia. 5 Dec. 2009]
[2] ["Tuberculosis-can the spread of this killer disease be halted?". Microbes and Diseases Fact file 1]
[3] [Richard Coker, Martin McKee, Rifat Atun, Boika Dimitrova, Ekaterina Dodonova, Sergei Kuznetsov, and Francis Drobniewski
Risk factors for pulmonary tuberculosis in Russia: case-control study
BMJ, Jan 2006; 332: 85 - 87. ]
[4] [Adverse reactions among patients being treated for MDR-TB in Tomsk, Russia.
S. S. Shin, A. D. Pasechnikov, I. Y. Gelmanova, G. G. Peremitin, A. K. Strelis, S. Mishustin, A. Barnashov, Y. Karpeichik, Y. G. Andreev, V. T. Golubchikova, T. P. Tonkel, G. V. Yanova, A. Yedilbayev, M. L. Rich, J. S. Mukherjee, J. J. Furin, S. Atwood, P. E. Farmer, and S. Keshavjee
Int J Tuberc Lung Dis. 2007 December; 11(12): 1314–1320.]
[5] [Rates of Latent Tuberculosis in Health Care Staff in Russia
Francis Drobniewski, Yanina Balabanova, Elena Zakamova, Vladyslav Nikolayevskyy, and Ivan Fedorin
PLoS Med. 2007 February; 4(2): e55. Published online 2007 February 13. doi: 10.1371/journal.pmed.0040055.
PMCID: PMC1796908]
[6]["Barriers to successful tuberculosis treatment in Tomsk, Russian Federation: non-adherence, default and the acquisition of multidrug resistance". http://www.who.int/bulletin/volumes/85/9/06-038331-ab/en/index.html. 5 Dec. 2009]
[7][Eur J Public Health. 2007 Feb;17(1):98-103. Epub 2006 Jul 12.
Reform of tuberculosis control and DOTS within Russian public health systems: an ecological study.
Marx FM, Atun RA, Jakubowiak W, McKee M, Coker RJ.
Department of Public Health and Policy, London School of Hygiene and Tropical Medicine Keppel Street, London, UK.]
[8]["Tough measures in Russian prisons slow spread of TB". http://www.who.int/bulletin/volumes/84/4/news30406/en/index.html. 5 Dec. 2009]
Edited by student of Joan Slonczewski for BIOL 191 Microbiology, 2009, Kenyon College.