Enterobacter aerogenes: Difference between revisions
No edit summary |
No edit summary |
||
| (16 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
{{Curated}} | |||
{{Biorealm Genus}} | {{Biorealm Genus}} | ||
| Line 48: | Line 49: | ||
Risk factors for nosocomial ''Enterobacter'' species like ''E. aerogenes'' infections include hospitalization of greater than 2 weeks, invasive procedures in the past 72 hours, treatment with antibiotics in the past 30 days, and the presence of a central venous catheter. Specific risk factors for infection with nosocomial multidrug-resistant strains of ''Enterobacter'' species should be taken into account and include the recent use of broad-spectrum cephalosporins or aminoglycosides and ICU care (13). | Risk factors for nosocomial ''Enterobacter'' species like ''E. aerogenes'' infections include hospitalization of greater than 2 weeks, invasive procedures in the past 72 hours, treatment with antibiotics in the past 30 days, and the presence of a central venous catheter. Specific risk factors for infection with nosocomial multidrug-resistant strains of ''Enterobacter'' species should be taken into account and include the recent use of broad-spectrum cephalosporins or aminoglycosides and ICU care (13). | ||
In addition to the expanded spectrum of cephalosporins, ''Enterobacter aerogenes'' was recently shown to develop resistance to carbapenems in a 39-year-old Chinese male following a cadaveric liver transplant. The original infection was thought to be related to the immunosuppressive characteristics of chemotherapy that the man received for liver cancer, facilitating a shift of microorganisms from the intestinal tract into the blood and other parts of the body. Post operation but prior to carbapenem therapy, a carbapenem sensitive strain of ''E. aerogenes'' was extracted from the bile, abdominal dopsy and blood. Despite carbapenem therapy, the patient developed multiple abcesses in the abdominal region, eventually leading to a second liver transplant two months later, at which time carbapenem resistant ''E. aerogenes'' was isolated from the blood and abdominal fluid. The patient subsequently developed septic shock and multiple organ dysfunction syndrome resulting from the immune and systemic response to the resistant bacteria. (18). | |||
Carbapenem resistance can emerge after 40 days of carbapenem resistance and its mechanism can be directly correlated with the loss of the OmpE36 gene along with the production of multiple beta-lactamases that confer its resistance to other broad spectrum antibiotics as well. Overall, these results are unfortunate as carbapenems are “almost a last resort in end-stage infection.” For such scenarios, propositions of using “old” drugs such as colistin have been made, despite their great nephro- and neurotoxicity (18.) | |||
Enterobacteriaceae aerogenes cause a variety of infections, often transmitted in the hospital setting. More importantly, Enterobacteriaceae aerogenes has shown to display multidrug resistance due largely to mutations that encode porins (protein channels) and membrane efflux pumps that pump out antibiotics before they can harm the organism. These have been shown to be non-specific which accounts for their multiple drug resistance. Structurally unrelated molecules such as B-lactam antibiotics, quinolones, tetracyclines, and chloramphenicol are all kept at bay. New drugs targeting this bacterium must focus on this line of bacterial defense, and this specific study focused on several alkoxyquinoline derivatives or 4-alkoxysubstituted quinoline compounds. One of these particular compounds, labeled “compound 905”, was shown to induce the inhibition of the chloramphenicol pump, allowing the chloramphenicol to enter the bacterial membrane, increasing concentrations of it inside the cell. Membrane permeability was tested to ensure that the results were not influenced by compound side-effects increasing membrane permeability. It was shown that the compound did not significantly increase membrane permeability, pointing to a unique and specific effect on chloramphenicol pump activity. Four of the clinical strains tested had increased susceptibility to norfloxacin, tetracycline, and chloramphenicol, which were previously kept outside of the cell by efflux pumps. Compound 905 inhibited these pumps, allowing for the antibiotics to build up significant concentrations inside the cells (23). | |||
==Application to Biotechnology== | ==Application to Biotechnology== | ||
| Line 62: | Line 69: | ||
Other ''Enterobacter'' are being observed especially those concerning the species ''Enterobacter sakazakii'' which is an infant formula-borne pathogen that causes severe meningitis, meningoencephalitis, sepsis, and necrotizing enterocolitis in neonates and infants, creating a high fatality rate. The outer membrane protein A gene (ompA) and sequences from ''E. sakazakii'' (ATCC 51329), were cloned in the pGEM-T Easy vector and sequenced. A high degree of homology with ompA genes of other gram-negative bacteria belonging to the Enterobacteriaceae was discovered when the nucleotide and deduced amino acid sequences were compared to those in GenBank. The proteins were found to have an identity of 89% and a sequence conservation of 94% at the amino acid level. Similarly, the ompA gene of ''E. sakazakii'' had sequence identities of 86% and 88% at the nucleic acid and amino acid levels. Additionally, with ''Enterobacter aerogenes'', 87% and 90% with ''serovar Typhimurium'', and 85% and 88% with ''Shigella flexneri''. A signal peptide cleavage site prediction analysis thus revealed a 21-amino-acid N-terminal signal sequence similar to those found in ''E. coli, E. aerogenes, S. flexneri'', and ''S. enterica serovar Typhi'' (16). | Other ''Enterobacter'' are being observed especially those concerning the species ''Enterobacter sakazakii'' which is an infant formula-borne pathogen that causes severe meningitis, meningoencephalitis, sepsis, and necrotizing enterocolitis in neonates and infants, creating a high fatality rate. The outer membrane protein A gene (ompA) and sequences from ''E. sakazakii'' (ATCC 51329), were cloned in the pGEM-T Easy vector and sequenced. A high degree of homology with ompA genes of other gram-negative bacteria belonging to the Enterobacteriaceae was discovered when the nucleotide and deduced amino acid sequences were compared to those in GenBank. The proteins were found to have an identity of 89% and a sequence conservation of 94% at the amino acid level. Similarly, the ompA gene of ''E. sakazakii'' had sequence identities of 86% and 88% at the nucleic acid and amino acid levels. Additionally, with ''Enterobacter aerogenes'', 87% and 90% with ''serovar Typhimurium'', and 85% and 88% with ''Shigella flexneri''. A signal peptide cleavage site prediction analysis thus revealed a 21-amino-acid N-terminal signal sequence similar to those found in ''E. coli, E. aerogenes, S. flexneri'', and ''S. enterica serovar Typhi'' (16). | ||
Recent research has been conducted in hopes to identify a correlation between presence of extended spectrum beta lactamase encoded plasmids (“ESBL”) and the drug resistance of different gram negative bacteria. Using six different species, including “Enterobacter aerogenes”, data was collected to try to assay the effect of ESBL. Of the six species studied, all of them except for one were positive for the ESBL plasmid. In turn, they displayed resistance to "gentamicin, amikacin, and ciproflaxin" as well as a resistance to beta lactam antibiotics. Some of the bacteria only had one copy of the plasmid, however, others had as many as thirteen. A correlation was seen with the number of copies of the gene and the resistance to the antibiotics. Authors of the study believed that the use of antibiotic put selective pressure on the bacteria, and that the plasmids often code for multiple resistances. So, the bacteria that are selected for not only have a resistance to the antibiotic being used but also to possible other unrelated antibiotics. The results of this research leaves the authors hopeful that continued research will be conducted to analyze the importance of these ESBL plasmids (20). | |||
A recent case study investigated five isolates of E. aerogenes showing resistance to β-lactam and fluoroquinolones during therapy of a patient who underwent myocardial revascularization. The patient was administered broad-spectrum antibiotics including imipenem and polymyxin, consequently giving rise to imipenem and polymyxin-resistant mutants of E. aerogenes due to modifications in porin synthesis and LPS balance. Five isolates of these resistant strains termed A,B,C,D, and E were compared using PFGE (Pulse-Field Gel Electrophoresis) to parental strand ATCC13048. A correlation was reported between the isolates with the presence of Omp36 coding for porin synthesis seen in isolate A, and those that had the OmpX gene which down-regulated porin expression (isolates B and C) so that isolates with OmpX conferred resistance to impenem. Previous studies have shown that modifications in the LPS have contributed to antibiotic resistance. These results show that the OmpA gene responsible for LPS modifications were present in all five isolates, including the parental strand ATCC13048. Isolates D and E have shown deviations in LPS balance from ATCC13048, causing resistance to colistin shortly after administration. Since PFGE profiles of all five isolates show similarity, researchers have suggested that isolates B through E are variants of isolate A, arising in response to antibiotics given to the patient during the time period of therapy (22). | |||
==Other members of same genus== | |||
We found an interesting article on the bacteria Enterobacter cloacae. This article talks about Enterobacter cloacae and how it is resistant to third generation cephalosporins. Cephalosporins are under the class of B-Lactam antibiotics and these type of antibiotics work by inhibiting bacterial cell wall synthesis. B-Lactams covalently binds to and inactivates transpeptidase enzymes (which are responsible for cross-linking the amino acid that form the peptidoglycan layer of the cell wall). Since the the transpeptidase enzyme is now inactivated by the antibiotic, and the cell wall can no longer form crosslinkages, the cell will eventually burst and lyse, thus killing the bacteria. However, bacteria have developed different types of resistance to antibiotics. For example, the enzyme B-lactamase serves to hydrolyze and break the B-Lactam rings of antibiotics and therefore nullifies the antibiotics effects. This article shows that research shows that the B-Lactamase of Enterobacter cloacae play a different role. They do not hydrolyze the B-Lactam rings. Instead Enterobacter cloacae’s resistance to cephalosporins arises from mutation due to constitutive production of B-Lactamases. The article concludes that after many experiments done, the resistance mechanism for Enterobacter cloacae is still yet to be determined but it is a fact that there is no hydrolysis of the B-Lactam ring and that some sort of mutation is causing the prevention of the binding of the drug to the enzyme or that there is some sort of permeation barrier that is responsible for the resistance. | |||
==Energy Source== | ==Energy Source== | ||
| Line 105: | Line 121: | ||
17. Yokoi, Haruhiko, et al. “Characteristics of Hydrogen Production by Aciduric Enterobacter aerogenes Strain HO-39.” Journal of Fermentation and Bioengineering Vol. 80 No. 6 (1995): 571-574. Print. | 17. Yokoi, Haruhiko, et al. “Characteristics of Hydrogen Production by Aciduric Enterobacter aerogenes Strain HO-39.” Journal of Fermentation and Bioengineering Vol. 80 No. 6 (1995): 571-574. Print. | ||
Thiolas, Aurélie, Claude Bollet,[et al.] Successive Emergence of ''Enterobacter aerogenes'' Strains Resistant to Imipenem and Colistin in a Patient. Antimicrobial Agents and Chemotherapy, 2005 April; 49 (4): 1354-1358. | 18. Chen, Hao, Ying Zhang, Ya-Gang Chen, Yun-Song Yu, and Shu-Sen Zheng. "Sepsis resulting from Enterobacter aerogenes resistant to carbapenems after liver transplantation." Hepatobiliary & Pancreatic Diseases International 8.3 (2009): 320-322. Web. 23 Apr 2010. <www.hbpdint.com/pdfdown.asp?id=1243>. | ||
19. Thiolas, Aurélie, Claude Bollet,[et al.] Successive Emergence of ''Enterobacter aerogenes'' Strains Resistant to Imipenem and Colistin in a Patient. Antimicrobial Agents and Chemotherapy, 2005 April; 49 (4): 1354-1358. | |||
20. Sharma J, Ray P, Sharma M. Plasmid profile of ESBL producing Gram-negative bacteria and correlation with susceptibility to β-lactam drugs. Indian J Pathol Microbiol 2010;53:83-6 | |||
21.A H Seeberg, R M Tolxdorff-Neutzling, and B Wiedemann Chromosomal beta-lactamases of Enterobacter cloacae are responsible for resistance to third-generation cephalosporins.Antimicrob. Agents Chemother., Jun 1983; 23: 918 - 925. | |||
22. Thiolas, Aurélie, Claude Bollet,[et al.] Successive Emergence of Enterobacter aerogenes Strains Resistant to Imipenem and Colistin in a Patient. Antimicrobial Agents and Chemotherapy, 2005 April; 49 (4): 1354-1358. | |||
23. Chevalier, J., Bredin, J., Mahamoud, A., Mallea, M., Barbe, J., & Pages, J.” Inhibitors of Antibiotic Efflux in Resistant Enterobacter aerogenes and Klebsiella pneumoniae Strains” Antimicrobial Agents And Chemotherapy, 2004. Volume 48, Issue 3. p. 1043-1046. | |||
Parts of this page were created by Tiffany M. Liu, a student of Professor [mailto:ralarsen@ucsd.edu Rachel Larsen] at the University of California, San Diego. | Parts of this page were created by Tiffany M. Liu, a student of Professor [mailto:ralarsen@ucsd.edu Rachel Larsen] at the University of California, San Diego. | ||
Edited by students of [mailto:mglogow@luc.edu M Glogowski] at Loyola University | Edited by Paul Erpelo/ Salvatore Grasso /Everardo Mojica/ Joseph Truong and Frank Wolf/ Kimberly Klages and Sandra Montes/ Daisy Mendez students of [mailto:mglogow@luc.edu M Glogowski] at Loyola University | ||
<!-- Do not edit or remove this line-->[[Category:Pages edited by students of Mary Glogowski at Loyola University]] | |||
Latest revision as of 19:22, 22 April 2011
A Microbial Biorealm page on the genus Enterobacter aerogenes
Classification
Higher order taxa
Bacteria; Proteobacteria; Gammaproteobacteria; Enterobacteriales; Enterobacteriaceae; Enterobacter
Species
Enterobacter aerogenes
Discussions on the true taxonomy of E. aerogenes presently exist due to the genomic distance between E. cloacae and Klebsiella. Research shows that E. aerogenes is more closely related to Klebsiella (47-64%) than E. cloacae (44%).
Description and significance
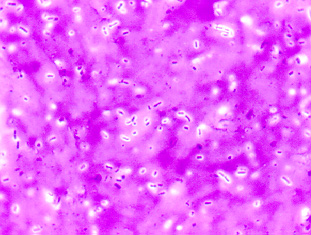
The Enterobacteriaceae family includes genera of Escherichia, Shilgella, Salmonella, Enterobacter, Klebsiella, Serratia, Proteus, amongst others. The gram-negative bacteria resides in soil, water, dairy products and inhabits a natural flora in the gastrointestinal tract of animals as well as humans. The rod shaped Enterobacteriaceae exists in a variety of sizes; are not spore forming; are both motile (with peritrichous flagella) or nonmotile; grow both aerobically and anaerobically; are active biochemically; ferment (versus oxidize) D-glucose as well as other sugars, often with gas production; reduce nitrate to nitrite; contain the enterobacter common antigen; and have a 39-59% guanine-plus-cytosine (G + C) content of DNA (2).
The genus Enterobacter is more specifically a nosocomial opportunistic pathogen and is sought out to be one of the many key causes for extraintestinal infections next to E. coli. Infections commonly attributed to E. aerogenes are respiratory, gastrointesntinal, and urinary tract infections, specifically cystits, in addition to wound, bloodstream, and central nervous system infections (1,2,3). Furthermore, E. cloacea and E. aerogenes are the species most commonly associated with aduilt cases of meningitis. Colonies of Enterobacter strains may be slightly mucoid.
In the clinical setting, Enterobacter aerogenes and Enterobacter cloacae are the most frequently isolated in samples of infected hospitalized patients. The majority of the infections are etiologically due to inadvertent transfer of bacteria during surgery or prolonged treatment in hospitals in patients who use venous or urethral catheters. Enterobacteriaceae may account for 80% of clinically significant isolates of gram-negative bacilli and for 50% of clinically significant bacteria in clinical microbiology laboratories. Additionally, they account for nearly 50% of septicemia cases and more than 70% of urinary and intestinal tract infections. The severity of these infections thus create an importance to target, isolate, identify and test for susceptibility for the causes of these nosocomial infections (2).
Genome structure
E. aerogenes are smaller, rod-shaped cells that are motile and encapsulated compared to others in the same family of Enterobacteriaceae. The complete genomic information (88% is coded) has not been entirely sequenced as of yet, however, there is some research that shows studies on mutations as well as show evidence of replication through plasmids. E. cloacae and E. aerogenes stain samples had no extrachromosomal elements (9). Plasmid analysis remains as one of the most utilized laboratory techniques used, but PFGE, RAPD, ribotyping, enterobacterial repetitive intergenic consensus (ERIC), PCR, and amplified fragment length polymorphism is also used. The replicon name is R751. The bacteria consists of DNA and is circular. Its length is recorded as 53,435 basepairs long and contains no structural RNAs. The G + C content is 64% and no psuedo genes are recorded for E. aerogenes (9).
Cell structure and metabolism
Enterbacter aerogenes is a gram-negative, rod shaped bacterium that contains flagella surrounding it's outer surface. E. aerogenes as well as others in its genus are known to be resistant to antibiotics, especially E. aerogenes and E. cloacae. Research shows that two clinical strains of E. aerogenes exhibited phenotypes of multiresistance to β-lactam antibiotics, fluoroquinolones, chloramphenicol, tetracycline, and kanamycin. Both strains showed a porin pattern different from that of a susceptible strain. They had a drastic reduction in the amount of the major porin but with an apparently conserved normal structure (size and immunogenicity), together with overproduction of two known outer membrane proteins, OmpX and LamB (8).
Ecology
Enterobacter are found in the soil, water, dairy products, and in the intestines of animals as well as humans. They are most frequently found in the gastrointestinal tract and are studied in clinical sites in stool samples. The minimum, optimum and maximum pH for E. aerogenes replication is 4.4, 6.0-7.0, and 9.0 (6).
Enterobacter aerogenes has been plated on several different medias and have been observed under several types of testing. The results are as follows- E. aerogenes tested negative when treated with/for: Indol, Methyl red, Hydrogen sulfide (by way of TSI), Urease, Arginine dihydrolase, Phenylalanine deaminase, and Dulcitol. E. aerogenes tested positive when treated with/for: Voges-Proskauer, Simmons' citrate, KCN, Motility, Lysine decarboxylase, Ornithine decarboxylase, Gas from glucose, Lactose, Sucrose, Manntiol, Salicin, Adonitol, Inositol, Sorbitol, Arabinose, Raffinose, and Rhamnose. Delayed positive results were obtained from: Gelatin (22°C) and Malonate (11). In other words, E. aerogenes resembles E. cloacae but the leusine decarboxylase test is positive and gelatin liquification is late. E. aerogenes is also, often times confused with Klebsiella aerogenes. However, E. aerogenes is motile and urease negative while K. aerogenes is nonmotile and urease positive (5). In actuality, research shows that "E. aerogenes is more related to Klebsiella aerogenes (47-64%) than it is to E. cloacae (44%) (9).
Different species of Enterobacter like E. cloacae are known to be found on a number of seeds and plants while E. sakazakii is commonly seen in infants who were given infant milk-based powder formulas (9).
Pathology
Enterobacter aerogenes causes disease in humans through inadvertent bacteria transfer in hospital settings. A selection of enteric bacteria like E. aerogenes are opportunistic and only infect those who already have suppressed host immunity defenses. Infants, the elderly, and those who are in the terminal stages of other disease or are immunosuppressed are prime candidates for such infections (9).
Additionally, E. aerogenes as well as other enteric bacteria, is known to have drug-resistant characteristics. There has been some success in dealing with infections through antibiotics, however, the fast development of multidrug resistence has become an increasingly growing problem (3). These multiresistant strains have caused outbreaks in intensive care units (ICUs) in Belgium, France, Austria, and the United States and has further become more emergent than its sister species E. cloacaw (12). Research has shown that E. aerogenes is resistant to ampicillin and it has been more recently discovered that it is resistant to imipenem (11).
In general, the pathogenic mechanisms expressed by strains of Enterobacter are unknown. Like other strains such as Klebsiella, they express type 1 and type 3 fimbraie. Most strains also express an aerobactin-mediated iron uptake systems, commonly associated with extra-intestinal human bacterial pathogens. Some strains may produce a haemolysin resembling the α-haemolysin produced by strains of E. coli. Additionally, an outer membrane protein, OmpX, may be a pathogenic factor for strains E. cloacae. This particular protein appears to reduce the production of porins on the gram-negative bacteria, leading to decreased sensitivity to β-lactam antibiotics and therefore might play a role in cell invasion of the host (7).
Enterobacter species produce type 1 or type 3 mannose sensitive hemagglutinins (MSHA) and rarely produce mannnose-resistant hemagglutinins. The only exception being E. gergoviae. Additionally, production of a variety of siderophores by enterobacters is also commonly seen. E. cloacae generate the hydroxyamate siderophore aerobactin, which is commonly used with microbial species that cause invasion disease. Additionally, several toxins have been found to be produced by Enterobacter species. Usually these toxins are described to having single strains or are limited in the number of isolates (9).
Preventative measures can be taken to reduce infection of E. aerogenes by monitoring careful, aseptic surgical techniques (3). Catheters should be removed and venous needles and tubing should be taken out and put in new locations. Treatment for E. aerogenes is difficult due to the highly resistant nature of the species. Enterobacter strains are resistant to penicillins and other cephalosporins because of the production of chromosomal beta-lactamase with cepholosprinase activity. Additionally, many are resistant to tetracycline, chloramphenicol and to streptomycin, as well as other aminoglycosides (such as gentamicin and fluoroquinolones). Most strains may appear to be susceptible to cefotaxime on primary testing, however, they often possess an inducible chromosomal cephalosporinase, allowing for the rapid development of resistance during treatment or therapy (7).
Risk factors for nosocomial Enterobacter species like E. aerogenes infections include hospitalization of greater than 2 weeks, invasive procedures in the past 72 hours, treatment with antibiotics in the past 30 days, and the presence of a central venous catheter. Specific risk factors for infection with nosocomial multidrug-resistant strains of Enterobacter species should be taken into account and include the recent use of broad-spectrum cephalosporins or aminoglycosides and ICU care (13).
In addition to the expanded spectrum of cephalosporins, Enterobacter aerogenes was recently shown to develop resistance to carbapenems in a 39-year-old Chinese male following a cadaveric liver transplant. The original infection was thought to be related to the immunosuppressive characteristics of chemotherapy that the man received for liver cancer, facilitating a shift of microorganisms from the intestinal tract into the blood and other parts of the body. Post operation but prior to carbapenem therapy, a carbapenem sensitive strain of E. aerogenes was extracted from the bile, abdominal dopsy and blood. Despite carbapenem therapy, the patient developed multiple abcesses in the abdominal region, eventually leading to a second liver transplant two months later, at which time carbapenem resistant E. aerogenes was isolated from the blood and abdominal fluid. The patient subsequently developed septic shock and multiple organ dysfunction syndrome resulting from the immune and systemic response to the resistant bacteria. (18).
Carbapenem resistance can emerge after 40 days of carbapenem resistance and its mechanism can be directly correlated with the loss of the OmpE36 gene along with the production of multiple beta-lactamases that confer its resistance to other broad spectrum antibiotics as well. Overall, these results are unfortunate as carbapenems are “almost a last resort in end-stage infection.” For such scenarios, propositions of using “old” drugs such as colistin have been made, despite their great nephro- and neurotoxicity (18.)
Enterobacteriaceae aerogenes cause a variety of infections, often transmitted in the hospital setting. More importantly, Enterobacteriaceae aerogenes has shown to display multidrug resistance due largely to mutations that encode porins (protein channels) and membrane efflux pumps that pump out antibiotics before they can harm the organism. These have been shown to be non-specific which accounts for their multiple drug resistance. Structurally unrelated molecules such as B-lactam antibiotics, quinolones, tetracyclines, and chloramphenicol are all kept at bay. New drugs targeting this bacterium must focus on this line of bacterial defense, and this specific study focused on several alkoxyquinoline derivatives or 4-alkoxysubstituted quinoline compounds. One of these particular compounds, labeled “compound 905”, was shown to induce the inhibition of the chloramphenicol pump, allowing the chloramphenicol to enter the bacterial membrane, increasing concentrations of it inside the cell. Membrane permeability was tested to ensure that the results were not influenced by compound side-effects increasing membrane permeability. It was shown that the compound did not significantly increase membrane permeability, pointing to a unique and specific effect on chloramphenicol pump activity. Four of the clinical strains tested had increased susceptibility to norfloxacin, tetracycline, and chloramphenicol, which were previously kept outside of the cell by efflux pumps. Compound 905 inhibited these pumps, allowing for the antibiotics to build up significant concentrations inside the cells (23).
Application to Biotechnology
Studies show that E. aerogenes has an increasing drug resistance rate. High levels of drug resistance in enterobacteria were found in accordance to aminoglycosides and broad-spectrum and fourth generation ceftazidime (>40%) and cefepime (15%). E. aerogenes stains showed production of extended-spectrum β-lactamases (ESBLs). A resistance such as this one often arises de novo in patients receiving empiric therapy for systemic infections. These drug resistant enterobacters can later emerge to produce severe or fulminant illnesses in immunosuppressed patients (9). Drug resistance such as these are common products of Enterobacter. Several drug therapies appear to be effective, however, after prolonged treatment, resistance arises and new drugs must be administered.
The involved resistance mechanisms exhibited by strains of E. aerogenes are associated with alterations of the outer membrane that cause a porin decrease and lipopolysaccharide modifications. As a result of its antibiotic resistance, many researchers have reverted back to "old drugs" such as colistin in addition to imipenem to treat severe E. aerogenes infections.
Current Research
In a case study used to determine the cause of infections in the aorta, isolation of two strains: S. pneumoniae and E. aerogenes were discovered and extracted from a 72 year old male suffering from epigastric pain, fevers, and chills. The orgin of E. aerogenes is unknown but is thought to be a result from and undiagnosed urinary tract infection or pneumonia. Research prior to this indicate that this case study is only the second report in the literature noting multiple organisms in infectious aortitis concerning E. aerogenes and S. pneumoniae. In addition to this, Enterobacter has only been reported as a cause of infectious aortitis in the setting of aortic grafts. This is the first time that Enterobacter has been reported in cryptogenic infectious aortitis. The study concluded that infections of the aorta are rare, are caused by various pathogens, and are difficult to diagnose. Symptoms that the patients may experience include fever and abdominal pain (and a palpable, pulsatile abdominal mass if the aorta is aneurysmal). Blood cultures, if positive, can be helpful, as are CTA, and leukocyte scintigraphic imaging. A high index of suspicion is necessary as the mortality, if only treated medically, approaches 100%. Combined surgical and medical therapy is superior, reducing the mortality rate to between 20% and 60% (14).
The Enterobacter aerogenes eefABC locus, which encodes a tripartite efflux pump, was cloned by complementation of an Escherichia coli tolC mutant. E. aerogenes became less susceptible to a wide range of antibiotics. Data from eef::lacZ fusions showed that eefABC was not transcribed in the various laboratory conditions tested, but instead increased transcription from Peef (from an E. coli hns mutant). Additionally, EefA was detected in E. aerogenes expressing a dominant negative E. coli hns allele. Research concluded that many H-NS target genes are involved in bacterial adaptation to stressful environmental conditions and virulence. The biological relevance of the eef operon silencing is still not known. However, like other commensal or pathogenic bacteria, E. aerogenes has to undergo drastic changes in its gene expression profile in order to adapt to the host-associated conditions (15).
Other Enterobacter are being observed especially those concerning the species Enterobacter sakazakii which is an infant formula-borne pathogen that causes severe meningitis, meningoencephalitis, sepsis, and necrotizing enterocolitis in neonates and infants, creating a high fatality rate. The outer membrane protein A gene (ompA) and sequences from E. sakazakii (ATCC 51329), were cloned in the pGEM-T Easy vector and sequenced. A high degree of homology with ompA genes of other gram-negative bacteria belonging to the Enterobacteriaceae was discovered when the nucleotide and deduced amino acid sequences were compared to those in GenBank. The proteins were found to have an identity of 89% and a sequence conservation of 94% at the amino acid level. Similarly, the ompA gene of E. sakazakii had sequence identities of 86% and 88% at the nucleic acid and amino acid levels. Additionally, with Enterobacter aerogenes, 87% and 90% with serovar Typhimurium, and 85% and 88% with Shigella flexneri. A signal peptide cleavage site prediction analysis thus revealed a 21-amino-acid N-terminal signal sequence similar to those found in E. coli, E. aerogenes, S. flexneri, and S. enterica serovar Typhi (16).
Recent research has been conducted in hopes to identify a correlation between presence of extended spectrum beta lactamase encoded plasmids (“ESBL”) and the drug resistance of different gram negative bacteria. Using six different species, including “Enterobacter aerogenes”, data was collected to try to assay the effect of ESBL. Of the six species studied, all of them except for one were positive for the ESBL plasmid. In turn, they displayed resistance to "gentamicin, amikacin, and ciproflaxin" as well as a resistance to beta lactam antibiotics. Some of the bacteria only had one copy of the plasmid, however, others had as many as thirteen. A correlation was seen with the number of copies of the gene and the resistance to the antibiotics. Authors of the study believed that the use of antibiotic put selective pressure on the bacteria, and that the plasmids often code for multiple resistances. So, the bacteria that are selected for not only have a resistance to the antibiotic being used but also to possible other unrelated antibiotics. The results of this research leaves the authors hopeful that continued research will be conducted to analyze the importance of these ESBL plasmids (20).
A recent case study investigated five isolates of E. aerogenes showing resistance to β-lactam and fluoroquinolones during therapy of a patient who underwent myocardial revascularization. The patient was administered broad-spectrum antibiotics including imipenem and polymyxin, consequently giving rise to imipenem and polymyxin-resistant mutants of E. aerogenes due to modifications in porin synthesis and LPS balance. Five isolates of these resistant strains termed A,B,C,D, and E were compared using PFGE (Pulse-Field Gel Electrophoresis) to parental strand ATCC13048. A correlation was reported between the isolates with the presence of Omp36 coding for porin synthesis seen in isolate A, and those that had the OmpX gene which down-regulated porin expression (isolates B and C) so that isolates with OmpX conferred resistance to impenem. Previous studies have shown that modifications in the LPS have contributed to antibiotic resistance. These results show that the OmpA gene responsible for LPS modifications were present in all five isolates, including the parental strand ATCC13048. Isolates D and E have shown deviations in LPS balance from ATCC13048, causing resistance to colistin shortly after administration. Since PFGE profiles of all five isolates show similarity, researchers have suggested that isolates B through E are variants of isolate A, arising in response to antibiotics given to the patient during the time period of therapy (22).
Other members of same genus
We found an interesting article on the bacteria Enterobacter cloacae. This article talks about Enterobacter cloacae and how it is resistant to third generation cephalosporins. Cephalosporins are under the class of B-Lactam antibiotics and these type of antibiotics work by inhibiting bacterial cell wall synthesis. B-Lactams covalently binds to and inactivates transpeptidase enzymes (which are responsible for cross-linking the amino acid that form the peptidoglycan layer of the cell wall). Since the the transpeptidase enzyme is now inactivated by the antibiotic, and the cell wall can no longer form crosslinkages, the cell will eventually burst and lyse, thus killing the bacteria. However, bacteria have developed different types of resistance to antibiotics. For example, the enzyme B-lactamase serves to hydrolyze and break the B-Lactam rings of antibiotics and therefore nullifies the antibiotics effects. This article shows that research shows that the B-Lactamase of Enterobacter cloacae play a different role. They do not hydrolyze the B-Lactam rings. Instead Enterobacter cloacae’s resistance to cephalosporins arises from mutation due to constitutive production of B-Lactamases. The article concludes that after many experiments done, the resistance mechanism for Enterobacter cloacae is still yet to be determined but it is a fact that there is no hydrolysis of the B-Lactam ring and that some sort of mutation is causing the prevention of the binding of the drug to the enzyme or that there is some sort of permeation barrier that is responsible for the resistance.
Energy Source
One of the bi-products of fermentation is hydrogen gas. The ability of Enterobacter aerogenes to produce hydrogen through the fermentation of a variety of sugars, including glucose, galactose, fructose, mannose, mannitol, sucrose, maltose, and lactose, has led scientists to investigate the use of this bacteria’s metabolism as a means of acquiring clean energy. Many bacteria can produce hydrogen through fermentation at a neutral pH, and E. aerogenes is no exception. Its optimal pH for hydrogen production is between 6 and 7. However, maintaining that high of a pH is difficult during fermentation because the process yields acidic products such as acetic acid, succinic acid, and lactic acid, and the accumulation of those products causes a decrease in pH. Typically, bacteria cease fermentation and thus cease the production of hydrogen at such low pH levels. However, one strain of E. aerogenes, HO-39, has the ability to continue fermentation at pH levels as low as 4. This quality makes strain HO-39 desirable as an energy source because it will continue energy production without much regulation of the bacterial environment. When bacterial fermentation is inhibited at low pH levels, alkali must continually be added to the bacterial culture in order to counteract the low pH that is caused by the accumulation of the organic acids. Alkali is expensive and, consequently, is uneconomical for the harnessing of energy. Using an aciduric facultative anaerobe such as E. aerogenes will reduce the amount of alkali that is necessary to maintain hydrogen production. Thus, this bacterium could be used as a cost-effective, clean energy source (17).
References
1. Brooks, Geo F., MD; Karen C. Carrol, MD; Janet S. Butel, PhD; Stephen A. Morse, PhD. Jawetz, melnick, & Adelberg’s Medical Microbiology. 24th ed. New York: McGraw Hill, 2007.
2. Lederberg, Joshua; Martin Alexander [et al.]. Encyclopedia of Microbiology. 2nd ed. San Diego, Ca.: Academic Press, 2000
3. Sankaran, Neeraja. Microbes and People an A-Z of Microorganisms in Our Lives. Phoenix, Az.: Oryx Press, 2000
4. National Center for Biotechnology Information site: http://www.ncbi.nlm.nih.gov/sites/entrez?Db=genome&Cmd=ShowDetailView&TermToSearch=11232
5. Collins, C.G.; P.M. Lune, J.M. Grange, J.O Falkinham III. Microbiological Methods. 8th ed. London: Arnold, 2004
6. Atlas, Ronald M.; Richard Bartha. Microbial Ecology Fundamentals and Applications. 4th ed. Menlo Park, Ca.: Bemjammin/Cummings Publishing Company, Inc., 1998
7. Greenwood, David; Richard C.B. Slack; John F. Peuthere. Medical Microbiology, a Guide to Microbial Infections: Pathogens, Immunity, Laboratory Diagnosis and Control. Edinburgh: Churchill Livingstone, 2002
8. National Center for Biotechnology Information site: http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=153306
9. Janda, J. Michael; Sharon L. Abbott. The Enterobacteria 2nd ed. Washington D.C.: ASM press, 2006
10. National Center for Biotechnology Information site: http://www.ncbi.nlm.nih.gov/sites/entrez?Db=genome&Cmd=ShowDetailView&TermToSearch=11232
11. Bailey, W.R. and E.G. Scott. Diagnostic Microbiology, 4th ed. St. Louis, Mo.: The C.V. Mosby Co., 1974
12. De Gheldre, Y. [et al.]. National Epidemiologic Surveys of Enterobacter aerogenes in Belgian Hospitals from 1996 to 1998. J Clin Microbiol. 2001 March 39(3): 889–896
13. Fraser, Susan L. MD, [et al.]. Enterobacter Infections. eMedicine. 2007 Jan.
14. Rhondina, Matthew T. [et al.]. Abdominal Aortitis due to Streptococcus pneumoniae and Enterobacter aerogenes A Case Report and Review. J Gen Intern Med. 2006 July; 21(7): C1–C3.
15. Masi, Muriel, [et al.]. The eefABC Multidrug Efflux Pump Operon Is Repressed by H-NS in Enterobacter aerogenes. J Bacteriol. 2005 June; 187(11): 3894–3897.
16. Kumar Mohan Nair, Monoj [et al.]. Cloning and Sequencing of the ompA Gene of Enterobacter sakazakii and Development of an ompA-Targeted PCR for Rapid Detection of Enterobacter sakazakii in Infant Formula. Appl Environ Microbiol. 2006 April; 72(4): 2539–2546.
17. Yokoi, Haruhiko, et al. “Characteristics of Hydrogen Production by Aciduric Enterobacter aerogenes Strain HO-39.” Journal of Fermentation and Bioengineering Vol. 80 No. 6 (1995): 571-574. Print.
18. Chen, Hao, Ying Zhang, Ya-Gang Chen, Yun-Song Yu, and Shu-Sen Zheng. "Sepsis resulting from Enterobacter aerogenes resistant to carbapenems after liver transplantation." Hepatobiliary & Pancreatic Diseases International 8.3 (2009): 320-322. Web. 23 Apr 2010. <www.hbpdint.com/pdfdown.asp?id=1243>.
19. Thiolas, Aurélie, Claude Bollet,[et al.] Successive Emergence of Enterobacter aerogenes Strains Resistant to Imipenem and Colistin in a Patient. Antimicrobial Agents and Chemotherapy, 2005 April; 49 (4): 1354-1358.
20. Sharma J, Ray P, Sharma M. Plasmid profile of ESBL producing Gram-negative bacteria and correlation with susceptibility to β-lactam drugs. Indian J Pathol Microbiol 2010;53:83-6
21.A H Seeberg, R M Tolxdorff-Neutzling, and B Wiedemann Chromosomal beta-lactamases of Enterobacter cloacae are responsible for resistance to third-generation cephalosporins.Antimicrob. Agents Chemother., Jun 1983; 23: 918 - 925.
22. Thiolas, Aurélie, Claude Bollet,[et al.] Successive Emergence of Enterobacter aerogenes Strains Resistant to Imipenem and Colistin in a Patient. Antimicrobial Agents and Chemotherapy, 2005 April; 49 (4): 1354-1358.
23. Chevalier, J., Bredin, J., Mahamoud, A., Mallea, M., Barbe, J., & Pages, J.” Inhibitors of Antibiotic Efflux in Resistant Enterobacter aerogenes and Klebsiella pneumoniae Strains” Antimicrobial Agents And Chemotherapy, 2004. Volume 48, Issue 3. p. 1043-1046.
Parts of this page were created by Tiffany M. Liu, a student of Professor Rachel Larsen at the University of California, San Diego.
Edited by Paul Erpelo/ Salvatore Grasso /Everardo Mojica/ Joseph Truong and Frank Wolf/ Kimberly Klages and Sandra Montes/ Daisy Mendez students of M Glogowski at Loyola University
