Y. enterocolitica: Difference between revisions
| Line 21: | Line 21: | ||
===Invasion=== | ===Invasion=== | ||
<i> Y. enterocolitica </i> can efficiently colonize the small intestine. After entering the host, bacteria colonize on the lumen and invade the epithelial lining—resulting in peyer patches [1]. <i> Y. enterocolitica </i> colonization requires the transfer of the bacteria across the epithelial tissue barrier. Produces 3 invasions proteins—Ail, YadA and invasin [1]. These proteins promote adherence and invasion of M cells, a type of antigen-sampling intestinal epithelial cells. | <i> Y. enterocolitica </i> can efficiently colonize the small intestine. After entering the host, bacteria colonize on the lumen and invade the epithelial lining—resulting in peyer patches [[#References|[1]]]. <i> Y. enterocolitica </i> colonization requires the transfer of the bacteria across the epithelial tissue barrier. Produces 3 invasions proteins—Ail, YadA and invasin [[#References|[1]]]. These proteins promote adherence and invasion of M cells, a type of antigen-sampling intestinal epithelial cells. | ||
===Infectious dose, incubation, and colonization=== | ===Infectious dose, incubation, and colonization=== | ||
Revision as of 10:25, 17 July 2014
Etiology/Bacteriology
Taxonomy
| Domain = Bacteria | Phylum = Proteobacteria | Class = Gammaproteobacteria | Order = Enterobacteriales | Family = Enterobacteriaceae | Genus = Yersinia | species = Y. enterocolitica
Description
Yersinia enterocolitica is a Gram negative coccobacillus-shaped bacterium, a facultative anaerobe motile at temperatures ranging from 22 to 30°C, and is not part of the human microbiota, but has been isolated from clinical specimens along with many other animals including pigs, cattle, birds, and domestic animals. Y. enterocolitica is psychrotrophic meaning it can flourish in lower temperatures, even below 4°C, meaning it can survive freezing and in frozen foods for a long period. There are several different types of Yersinia enterocolitica based by the same surface antigens they share and are categorized according to which O-antigen they express on their surface, however only certain types are pathogenic for human. Yersinia enterocolitica infection is common year-round, but reaches its peak in fall and winter and certain types also depend upon different geographical areas, such as type O:3 and O:9 are responsible for outbreaks in Europe, while type O:8 is found in the United States, and O:5 and O:27 are found in Canada and Japan. Yersinia enterocolitica is a common cause of food-borne gastrointestinal disease in moderate and subtropical climates around the world. An infection may present itself as enteritis, terminal ileitis, or mesenteric lyphadenitis, which is pseudoappendicitis meaning it was mistaken as appendicitis. As a zoonotic pathogen,Y. enterocolitica can infect the host after ingestion of contaminated food or water, and although host gastric acid act as a substantial barrier to infection of the pathogen it utilizes plasmids affecting pathogenesis. These include an outer membrane protein, YadA, used for adhesion and it can also resist phagocytosis by host cell by the help of Yops proteins. Yersiniosis, a disease caused by this organism has symptoms of abdominal pain and fever along with diarrhea that occurs in 80% of cases. Patients usually recover within three weeks of infection on their own, unless it becomes chronic entercolitis, which may last up to months, however nonetheless fatalities are extremely rare with an infection of Yersinia entercolitica. Infection by this pathogen can be easily prevented using proper sterilization techinques when dealing with food, and just having good hygiene in general, as well as avoiding raw milk or undercooked pork products.
Pathogenesis
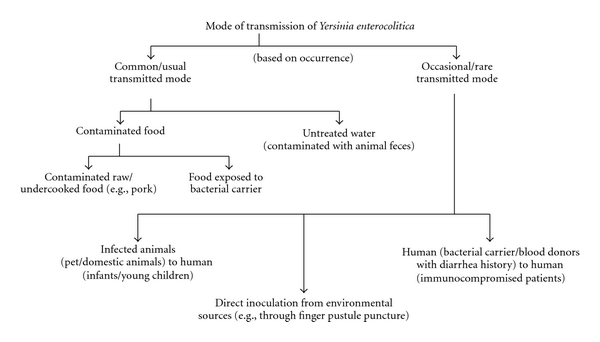
Transmission
Yersinia enterocolitica is found in meats (pork, beef lamb ect) fish, and raw milk. Exact reason for food contamination is unknown [2]. Human-to-human transmission is rare however incidences have been observed and reported. It is thought that an infected person suffering from diarrheal symptoms will transmit the disease to others if proper hand washing techniques are not followed. Yersinia enterocolitica infection results in yersiniosis—a zoonotic disease that occurs in humans, cattle deer, birds and pigs [2]. Only a few strains cause infection in humans, and children are infected more often than adults. However, there are extreme cases in which Y. enterocolitica has been transmitted via blood transfusions. In such cases, transfusion acquired septicemia usually results from the infected blood serum. There are over 60 serotypes for Yersinia enterocolitica . The serotypes pathogenic to humans are O:3, O:5,27, O:8, O:9, and O:13 [1,2].
Invasion
Y. enterocolitica can efficiently colonize the small intestine. After entering the host, bacteria colonize on the lumen and invade the epithelial lining—resulting in peyer patches [1]. Y. enterocolitica colonization requires the transfer of the bacteria across the epithelial tissue barrier. Produces 3 invasions proteins—Ail, YadA and invasin [1]. These proteins promote adherence and invasion of M cells, a type of antigen-sampling intestinal epithelial cells.
Infectious dose, incubation, and colonization
According to the CDC Yersinia enterocolitica infectious dose is currently unknown, however according to the FDA although it is not known they estimate it to be between 104 to 106 organisms. The infectious does may depend on the strain and host factors, for example it will take a lower dose of organisms to cause yersiniosis in young children and the elderly that have weakened immune systems compared to a healthy host. Illness takes place between 24 and 48 hours after ingestion [3]. Illness typically presents as Diarrhea—sometimes bloody—low-grade fever, abdominal pain and vomiting is present in 15%-40% of cases [1]. Yersiniosis is a less common infection, because most food processing techniques eliminate the risk for infection [3].
Virulence Factors
Enterotoxicity
The toxin Yst including the genes ystA and ystB in the organism is a membrane-acting virulence factor. It is a heat-stable enterotoxin that is important in causing diarrhea in the host, however it is only present in virulent strains of Y. enterocolitica . It stimulates the cGMP synthesis in the intestinal lining, which leads to an overall effect of fluid loss and lack of fluid absorption. The enterotoxin produced by Y. enterocolitica is similar to E. coli . Nevertheless, the enterotoxin only plays a minor role in pathogenesis, because diarrheal symptoms have been observed with the absence of enterotoxin formation [1] . The outer membrane antigens are associated with bacterial resistance to opsonization and neutrophil phagocytosis [1].
Iron and pathogenicity
Y. enterocolitica is unable to chelate iron. Despite not being able to produce siderophores-- Y. enterocolitica can utilize siderophores produced by other bacteria [1]. This pathogen contains the plasmid PYV encoding virulence genes that affect pathogenesis. Included in these virulence genes it YadA (Yersinia adhesion A), which is an outer-membrane protein that is expressed by the organism. Also included is the type III secretory system guided by Yops proteins that offer Y. enterocolitica a way to resist phagocytosis and immune responses by the host.
Epidemiology
The most susceptible populations to Y. enterocolitica are small children, immuno-suppressed, and the elderly [3] . 75% of patients are between the age of 5-15 years [1]. Most isolates of the disease are type O:3 and O:9 serotypes in Canada and Europe. In the US it is estimated that approximately 5% of bacterial enteric infections for children under the age of 5.The CDC claims 17,000 cases annually in the United States [2]. The disease is much more common in Northern Europe, Scandinavia, and Japan.
Clinical Features
Yersinia enterocolitica normally causes diarrhea in all manifestations of the infection, with some severe cases having blood in the stools. Aside from diarrhea the disease may present differently when comparing adult and adolescent cases. Pediatric cases are characterized by fever, abdominal pain and more commonly present with bloody diarrhea. The most common presentation of Y. enterocolitica in children is enterocolitis. The symptoms include watery and mucoid diarrhea, fever and colicky abdominal pain, with blood and white blood cells in stools. Adults describe their symptoms as diarrhea, localized lower right quadrant abdominal pain, vomiting, and low-grade fever. Often the infection will clear without the aid of antibiotics, but those that do not may display more severe side effects including: red or purple raised lesions known as erythema nodosum and joint pain commonly in the knees, wrists or ankles. Erythema nodosum lesions appear 2-20 days after the onset of the infection and also resolve without medical treatment in about a month. Lesions are more commonly seen in females and appear on the patient’s trunk and legs. Joint pain may manifest about a month after the onset of symptoms and cease after 1 to 6 months. Septicemia, or bacteria in the blood, can occur in adults with predisposing conditions, such as diabetes mellitus, immune defect, alcoholism, thalassemia, sickle cell disease, or hemochromatosis. Septicemia can also cause metastatic infections including abscesses in the liver, spleen, kidneys and lungs.

Diagnosis
There are numerous tests that can be used to diagnose a Yersinia enterocolitica infection. A stool culture is the best way to confirm the presence of the pathogen but can take two weeks since the onset of the disease for the culture result to come back positive [1]. Other tests include tube agglutination, enzyme-linked immunosorbent assays, radioimmunoassays, ultrasonography or computed tomography scanning imaging studies, colonoscopy, and joint aspiration in certain cases [1]. A vast majority of Y. enterocolitica infections will clear up on their own with good nutrition and hydration. Severe or complicated infections can be treated with the antibiotics aminoglycosides, doxycycline, trimethoprim-sulfamethoxazole, or fluoroquinolones.
Treatment
Infections by Yersinia enterocolitica are usually self-limiting and will resolve on their own in most patients who recover without any antibiotic treatment within a seven days to three weeks. Hydration is important in uncomplicated cases of diarrhea caused by the organism and will be sufficient treatment in the infection, however in severe or more complicated cases of infection antibiotic treatment may be necessary. The antibiotics commonly used are aminoglycosides, doxycycline, trimethoprim-sulfamethoxazole, or fluoroquinolones.
Prevention
Prevention of Yersinia enterocolitica infection is easy if one is aware of what to avoid. The most common mode of transmission is via poultry and livestock. Thus, avoid raw or undercooked meats. Make sure that milk products are pasteurized before consumption. If raw meat must be handled, clean hands thoroughly to avoid cross-contamination. Beware of cross-contamination in the kitchen by cleaning all surfaces and appliances with soap and hot water. Animal feces may also be contaminated so dispose of all animal waste properly.
Host Immune Response
References
1. Medscape. http://emedicine.medscape.com/article/232343-overview
2. CDC. http://www.cdc.gov/ncidod/dbmd/diseaseinfo/yersinia_g.htm
3. FDA. http://www.fda.gov/Food/FoodborneIllnessContaminants/CausesOfIllnessBadBugBook/ucm070040.htm
4. Hindawi http://www.hindawi.com/journals/jpath/2011/429069/
Created by Emily Kurtz, Kristen Hoelscher, Dane Korber and Caitlyn Baukal, students of Tyrrell Conway at the University of Oklahoma

