Gut Microbiota and Autism: Difference between revisions
| Line 15: | Line 15: | ||
The microbiome of individuals with autism spectrum disorder differs from that of the average person. Firstly, the intestinal environment itself is abnormal in patients with ASD compared to the typical person. Approximately one third of patients with ASD displayed a higher percentage of abnormal permeability in their intestines compared to the approximately 5% of abnormal permeability in the control population.<ref name=deMagistris>de Magistris L, Familiari V, Pascotto A, Sapone A, Frolli A, Iardino P, et al. Alterations of the Intestinal Barrier in Patients With Autism Spectrum Disorders and in Their First-degree Relatives. Journal of Pediatric Gastroenterology and Nutrition. 2010 Oct;51(4):418–24.</ref> This increased intestinal permeability causes an increased antigenic load from the GI tract. This allows more chemical signals originating from the GI tract to enter the circulation and then cross over the blood-brain barrier to deliver these chemical signals to the brain where they induce immune responses.<ref name=Li/> Therefore, the microbiota of ASD patients may have even more influence through the gut-brain axis than in the average person. | The microbiome of individuals with autism spectrum disorder differs from that of the average person. Firstly, the intestinal environment itself is abnormal in patients with ASD compared to the typical person. Approximately one third of patients with ASD displayed a higher percentage of abnormal permeability in their intestines compared to the approximately 5% of abnormal permeability in the control population.<ref name=deMagistris>de Magistris L, Familiari V, Pascotto A, Sapone A, Frolli A, Iardino P, et al. Alterations of the Intestinal Barrier in Patients With Autism Spectrum Disorders and in Their First-degree Relatives. Journal of Pediatric Gastroenterology and Nutrition. 2010 Oct;51(4):418–24.</ref> This increased intestinal permeability causes an increased antigenic load from the GI tract. This allows more chemical signals originating from the GI tract to enter the circulation and then cross over the blood-brain barrier to deliver these chemical signals to the brain where they induce immune responses.<ref name=Li/> Therefore, the microbiota of ASD patients may have even more influence through the gut-brain axis than in the average person. | ||
<br><br> | <br><br> | ||
Patients with ASD have different species of bacteria prevalent in their gut microbiome. The maternal immune activation (MIA) mouse model is an ideal model for studying ASD as it displays many features of the disorder. One study found that offspring of mothers with MIA had more <i>Porphyromonadaceae, Prevotellaceae, </i>unclassified<i> Bacteroidales, </i>and<i> Lachnospiraceae</i> bacterias, whereas control offspring had more <i>Ruminococcaceae, Erysipelotrichaceae, </i>and <i>Alcaligenaceae</i> bacterias.<ref name=Hsiao>Hsiao EY, McBride SW, Hsien S, Sharon G, Hyde ER, McCue T, et al. Microbiota Modulate Behavioral and Physiological Abnormalities Associated with Neurodevelopmental Disorders. Cell. 2013 Dec 19;155(7):1451–63.</ref> | Patients with ASD have different species of bacteria prevalent in their gut microbiome. The maternal immune activation (MIA) mouse model is an ideal model for studying ASD as it displays many features of the disorder. One study found that offspring of mothers with MIA had more <i>Porphyromonadaceae, Prevotellaceae, </i>unclassified<i> Bacteroidales, </i>and<i> Lachnospiraceae</i> bacterias, whereas control offspring had more <i>Ruminococcaceae, Erysipelotrichaceae, </i>and <i>Alcaligenaceae</i> bacterias.<ref name=Hsiao>Hsiao EY, McBride SW, Hsien S, Sharon G, Hyde ER, McCue T, et al. Microbiota Modulate Behavioral and Physiological Abnormalities Associated with Neurodevelopmental Disorders. Cell. 2013 Dec 19;155(7):1451–63.</ref> Another model system for studying ASD can be created by inducing autistic-like behaviors in offspring of mice through the administration of valproic acid in pregnant mice. In all offspring of the VPA treated mice, Bacteroidetes and <i>Desulfovibrionales</i> increased in prevalence while Firmicutes decreased. Additionally, male VPA offspring had more <i>Alistipes, Enterorhabdus, Mollicutes</i> and <i>Erysipelotrichalis</i> bacteria. | ||
==Development of Gut Microbiota and ASD== | ==Development of Gut Microbiota and ASD== | ||
Revision as of 06:42, 7 April 2021
Introduction
By Bailey Fitzgerald
3000 words
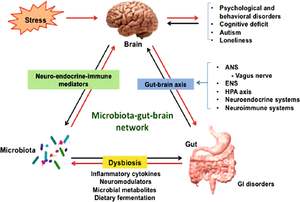
A healthy adult human intestine harbors billions of bacteria of over 1000 different species.[1][2] These bacteria play a large role in human health through digestion and aiding in immune system development.[2] However, these bacteria can also have a direct influence on their human host’s behavior. Gut microbes have the ability to bidirectionally communicate with the central nervous system and influence both emotional and cognitive centers of the brain.[3] This makes maintenance of the gut microbiome especially important in people with a variety of neurological conditions, including autism spectrum disorder (ASD).
Autism spectrum disorder is a neurological and developmental disorder characterized by deficits in social communication and social interaction, repetitive patterns of behavior or activities, and restricted interests.[4] ASD can range in severity from very high-functioning (formerly known as Asperger’s syndrome) in which the individual is able to go about daily life with little to no assistance to low-functioning individuals that need assistance with basic care and needs or anywhere in between. It is also common to have other diseases and conditions along with autism spectrum disorder. These comorbidities can include sleep disorders, seizure disorders, gastrointestinal disorders, metabolic disorders, and hormonal dysfunction.[5]
Gastrointestinal (GI) issues, such as frequent abdominal pain, gaseousness, diarrhea, constipation or pain on stooling, are a very common comorbidity in ASD patients.[6][7] Studies have found that 23 to 70% of people with ASD suffer from gastrointestinal dysfunction, with the wide range attributed to variances in survey methods.[7] Additionally, the prevalence of more gastrointestinal symptoms was strongly correlated with the severity of autism in patients.[8] These gastrointestinal issues can be attributed to a disturbance to normal gut flora composition.[8] Although the cause of the abnormal gut microbiome in patients with ASD is not certain, researchers hypothesize that it could be due to atypical eating habits.[9] Thus, therapies targeting the gut microbiome could have potential in treating and managing autism spectrum disorders. Because the exact causes of ASD and the mechanisms behind the disorder are difficult to identify, there are very few effective therapies available.[10] This makes the potential of microbiome treatments for ASD ever more promising and hopeful for managing the disorder.
Composition of the ASD Microbiome
The microbiome of individuals with autism spectrum disorder differs from that of the average person. Firstly, the intestinal environment itself is abnormal in patients with ASD compared to the typical person. Approximately one third of patients with ASD displayed a higher percentage of abnormal permeability in their intestines compared to the approximately 5% of abnormal permeability in the control population.[11] This increased intestinal permeability causes an increased antigenic load from the GI tract. This allows more chemical signals originating from the GI tract to enter the circulation and then cross over the blood-brain barrier to deliver these chemical signals to the brain where they induce immune responses.[6] Therefore, the microbiota of ASD patients may have even more influence through the gut-brain axis than in the average person.
Patients with ASD have different species of bacteria prevalent in their gut microbiome. The maternal immune activation (MIA) mouse model is an ideal model for studying ASD as it displays many features of the disorder. One study found that offspring of mothers with MIA had more Porphyromonadaceae, Prevotellaceae, unclassified Bacteroidales, and Lachnospiraceae bacterias, whereas control offspring had more Ruminococcaceae, Erysipelotrichaceae, and Alcaligenaceae bacterias.[12] Another model system for studying ASD can be created by inducing autistic-like behaviors in offspring of mice through the administration of valproic acid in pregnant mice. In all offspring of the VPA treated mice, Bacteroidetes and Desulfovibrionales increased in prevalence while Firmicutes decreased. Additionally, male VPA offspring had more Alistipes, Enterorhabdus, Mollicutes and Erysipelotrichalis bacteria.
Development of Gut Microbiota and ASD
Autism spectrum disorder has been observed to have both genetic and environmental factors to its development.[13] Environmental factors specifically affecting the composition and development of the gut microbiome may have an effect on the development of autism spectrum disorder. The most crucial environment in ASD development is the prenatal conditions within their mother’s womb. This is largely determined by maternal health.
Several studies have found a significant connection between maternal obesity, gestational diabetes (GDM), and pregestational diabetes (PGDM) in increased risk of ASD.[14][15][16] Having just one of these conditions during pregnancy is associated with a 1.5 to 2 times increased risk factor for ASD. Whereas when obesity and GDM or obesity and PGDM were both present in mothers, ASD risk showed approximately 2 to 4 times increase.[14][16]
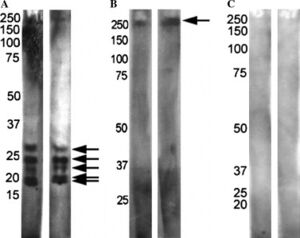
The maternal immune system and responses can also play a factor in ASD development. Mothers of children with ASD have been shown to possess different antibodies than mothers of neurotypical children.[17] When reacted with rat prenatal (PN18) brain proteins, mothers of children with ASD and children with ASD showed one of two patterns while control mothers and their neurotypical children typically showed no reactivity (Figure 3). This suggests these antibodies are pathogenic to fetal brains in autism.[17] Maternal antibodies have also been shown to react with lymphocytes in children with ASD which further suggests reactivity with other tissues in the developing embryo.[18]
A mother’s own microbiota can play a crucial role in fetal development. If the microbiome becomes imbalanced and pathogenic microbes are able to dominate, it can mean more than just illness for an expecting mother. Viral infections during the first trimester and bacterial infections during the second trimester have been associated with greater risk of ASD.[19] Additionally, delivery method can shape the microbiome of newborn babies. Infants delivered vaginally possess gut bacteria very similar to their mother’s vaginal microbiota, mostly composed of Lactobacillus, Prevotella, and Sneathis spp.; infants delivered via Cesarean section have a gut microbiome similar to the composition of their mother’s skin microbiota, mainly consisting of Staphylococcus, Corynebacterium, and Propionibacterium spp.[20] Autism spectrum disorder risk for infants delivered through Cesarean section has been found to be higher than in infants delivered vaginally.[21]
After birth, diet plays a critical role in shaping and maintaining the human gut microbiome. Risk of ASD has been observed to increase for infants that are not breastfed and decreases with longer periods of breastfeeding.[22] However, complications in breastfeeding infants with ASD, such as difficulty with the child’s engagement in the feeding process and temperamental or behavioral issues associated with ASD, may also be to blame for this correlation.[9] Later in life, feeding issues associated with ASD may contribute to an imbalanced gut microbiome. 90% of children with ASD display feeding related concerns, the most common of which is food selectivity.[23][9] This selectivity and imbalanced diet leads to many health concerns such as nutritional deficiencies and GI conditions.[9]
Animal Studies on ASD
Include some current research, with at least one figure showing data.
Microbiome Treatments for ASD
Conclusion
References
- ↑ Maukonen J, Saarela M. Human gut microbiota: does diet matter? Proceedings of the Nutrition Society. 2015 Feb;74(1):23–36.
- ↑ 2.0 2.1 Bull MJ, Plummer NT. Part 1: The Human Gut Microbiome in Health and Disease. Integr Med (Encinitas). 2014 Dec;13(6):17–22.
- ↑ Carabotti M, Scirocco A, Maselli MA, Severi C. The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Ann Gastroenterol. 2015;28(2):203–9.
- ↑ American Psychiatric Association, American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. 5th ed. Washington, D.C: American Psychiatric Association; 2013.
- ↑ Bauman ML. Medical comorbidities in autism: Challenges to diagnosis and treatment. Neurotherapeutics. 2010 Jul;7(3):320–7.
- ↑ 6.0 6.1 Li Q, Han Y, Dy ABC, Hagerman RJ. The Gut Microbiota and Autism Spectrum Disorders. Front Cell Neurosci [Internet]. 2017 [cited 2021 Mar 17];11. Available from: https://www.frontiersin.org/articles/10.3389/fncel.2017.00120/full?fbclid=IwAR04gQH8jD4LVLXEJnl7MfXsCyDR7USEauiGGIc1BXJY48GTn2L5GQg-Hk0
- ↑ 7.0 7.1 Chaidez V, Hansen RL, Hertz-Picciotto I. Gastrointestinal Problems in Children with Autism, Developmental Delays or Typical Development. J Autism Dev Disord. 2014 May 1;44(5):1117–27.
- ↑ 8.0 8.1 Adams JB, Johansen LJ, Powell LD, Quig D, Rubin RA. Gastrointestinal flora and gastrointestinal status in children with autism – comparisons to typical children and correlation with autism severity. BMC Gastroenterology. 2011 Mar 16;11(1):22.
- ↑ 9.0 9.1 9.2 9.3 Mulle JG, Sharp WG, Cubells JF. The Gut Microbiome: A New Frontier in Autism Research. Curr Psychiatry Rep. 2013 Feb 1;15(2):1–9.
- ↑ Rossignol DA, Frye RE. A review of research trends in physiological abnormalities in autism spectrum disorders: immune dysregulation, inflammation, oxidative stress, mitochondrial dysfunction and environmental toxicant exposures. Molecular Psychiatry. 2012 Apr;17(4):389–401.
- ↑ de Magistris L, Familiari V, Pascotto A, Sapone A, Frolli A, Iardino P, et al. Alterations of the Intestinal Barrier in Patients With Autism Spectrum Disorders and in Their First-degree Relatives. Journal of Pediatric Gastroenterology and Nutrition. 2010 Oct;51(4):418–24.
- ↑ Hsiao EY, McBride SW, Hsien S, Sharon G, Hyde ER, McCue T, et al. Microbiota Modulate Behavioral and Physiological Abnormalities Associated with Neurodevelopmental Disorders. Cell. 2013 Dec 19;155(7):1451–63.
- ↑ Hallmayer J. Genetic Heritability and Shared Environmental Factors Among Twin Pairs With Autism. Arch Gen Psychiatry. 2011 Nov 1;68(11):1095.
- ↑ 14.0 14.1 Connolly N, Anixt J, Manning P, Lin DP-I, Marsolo KA, Bowers K. Maternal metabolic risk factors for autism spectrum disorder—An analysis of electronic medical records and linked birth data. Autism Research. 2016;9(8):829–37.
- ↑ Jo H, Eckel SP, Chen J-C, Cockburn M, Martinez MP, Chow T, et al. Gestational diabetes mellitus, prenatal air pollution exposure, and autism spectrum disorder. Environment International. 2019 Dec 1;133:105110.
- ↑ 16.0 16.1 Li M, Fallin MD, Riley A, Landa R, Walker SO, Silverstein M, et al. The Association of Maternal Obesity and Diabetes With Autism and Other Developmental Disabilities. Pediatrics [Internet]. 2016 Feb 1 [cited 2021 Apr 6];137(2). Available from: https://pediatrics.aappublications.org/content/137/2/e20152206
- ↑ 17.0 17.1 Zimmerman AW, Connors SL, Matteson KJ, Lee L-C, Singer HS, Castaneda JA, et al. Maternal antibrain antibodies in autism. Brain, Behavior, and Immunity. 2007 Mar 1;21(3):351–7.
- ↑ Warren RP, Cole P, Odell JD, Pingree CB, Warren WL, White E, et al. Detection of Maternal Antibodies in Infantile Autism. Journal of the American Academy of Child & Adolescent Psychiatry. 1990 Nov 1;29(6):873–7.
- ↑ Atladóttir HÓ, Thorsen P, Østergaard L, Schendel DE, Lemcke S, Abdallah M, et al. Maternal Infection Requiring Hospitalization During Pregnancy and Autism Spectrum Disorders. J Autism Dev Disord. 2010 Dec;40(12):1423–30.
- ↑ Dominguez-Bello MG, Costello EK, Contreras M, Magris M, Hidalgo G, Fierer N, et al. Delivery mode shapes the acquisition and structure of the initial microbiota across multiple body habitats in newborns. Proceedings of the National Academy of Sciences. 2010 Jun 29;107(26):11971–5.
- ↑ Curran EA, O’Neill SM, Cryan JF, Kenny LC, Dinan TG, Khashan AS, et al. Research Review: Birth by caesarean section and development of autism spectrum disorder and attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. Journal of Child Psychology and Psychiatry. 2015;56(5):500–8.
- ↑ Al-Farsi YM, Al-Sharbati MM, Waly MI, Al-Farsi OA, Al-Shafaee MA, Al-Khaduri MM, et al. Effect of suboptimal breast-feeding on occurrence of autism: A case–control study. Nutrition. 2012 Jul 1;28(7):e27–32.
- ↑ Ledford JR, Gast DL. Feeding Problems in Children With Autism Spectrum Disorders: A Review. Focus Autism Other Dev Disabl. 2006 Aug 1;21(3):153–66.
Authored for BIOL 238 Microbiology, taught by Joan Slonczewski, 2021, Kenyon College.
