African Trypanosomiasis: a parasitic disease of the CNS: Difference between revisions
Mclaughlin2 (talk | contribs) |
Mclaughlin2 (talk | contribs) No edit summary |
||
| Line 38: | Line 38: | ||
The genome of <i>T.brucei</i> is 26 Mb, contains roughly 1700 variant surface glycoproteins along with around 900 pseudogenes [11]. Genome analysis has shown horizontal gene transfer allows for increased metabolic properties for trypanosome parasites [11]. <i>T.b. gambiense</i> is the strain mainly responsible for human infection, accounting for 98% of all diagnosed cases of african trypanosomiasis [3]. This strain is also responsible for retaining the majority of the genetic information with a smaller genome. | The genome of <i>T.brucei</i> is 26 Mb, contains roughly 1700 variant surface glycoproteins along with around 900 pseudogenes [11]. Genome analysis has shown horizontal gene transfer allows for increased metabolic properties for trypanosome parasites [11]. <i>T.b. gambiense</i> is the strain mainly responsible for human infection, accounting for 98% of all diagnosed cases of african trypanosomiasis [3]. This strain is also responsible for retaining the majority of the genetic information with a smaller genome. | ||
===Virulence Factors=== | |||
There are a number of cellular mechanisms, structures, and molecules that allow for full parasitic function of trypanosomes. Regarding immune response, <i>T. brucei</i> parasites are capable of invading a host's immune system through the use of a variable surface glycoprotein (VSG) [7]. VSGs aid in protecting these parasites from lytic factors, ultimately evading the natural host immune response. As infection is prevalent, gene conversion between VSGs occurs at the trypanosome expression site [8]. This is considered an antigenic variation which enables the parasite to avoid the body's immune response as well as continue infection throughout the host. This constant switching also has made it challenging for clinicians to develop a vaccine that trypanosomes cannot evade. | |||
Another strategy to evade immune response is through production of serum resistance associated proteins (SRAs) [7]. SRAs are unique to <i>T.b rhodesiense</i> and considered members of VSGs. They are exported to the flagellar pocket of trypanosomes before getting taken up by extracellular vesicles [12]. Serum resistant forms of <i>T.b rhodesiense</i> express and mRNA encoding protein, associated with surface glycoproteins [12]. Presence of SRAs aid in the survival of parasites, elongating the length and path of infection in a host. SRAs have the potential to evade cell lysis, preventing the breakdown of any present trypanosomes. | |||
An important mechanism of <i>T. brucei</i> parasites is their flagellum. The flagellum is essential for parasite motility, pathogenesis, transmission of infection as well as immune evasion. Their flagellum is surrounded by its own membrane and attaches by length to the trypanosome cell body [10]. This wrap-around is vital for trypanosomes to invade other tissues throughout the body, given its extracellular characteristics. Moreover, <i>T.brucei</i> contain a flagellar pocket which is essential for the export of VSGs to other tissues throughout the body as well as the protection of extracellular macromolecules from the host’s immune response [10]. The flagellum oversees host cell attachment through attachment plaques, allowing parasites to develop a VSG coat [10]. Once coated, parasites are released into salivary glands, unleashing infection within the host. | |||
===Epidemiology=== | ===Epidemiology=== | ||
| Line 69: | Line 78: | ||
===Prevention=== | ===Prevention=== | ||
==Next Steps== | ==Next Steps== | ||
Revision as of 23:48, 13 April 2024
Introduction
By Maeve McLaughlin
Human African Trypanosomiasis (HAT) informally known as African Sleeping Sickness is an infection directly linked to a microscopic parasitic species known as Trypanosoma brucei. T. brucei are members of the Trypanosoma genus as well as the Trypanosomatidae family of unicellular parasites [3]. HAT is an extremely rare disease in the United States with fewer than 1,000 cases per year, but has a history of epidemics in Sub-Saharan regions of Africa [1]. There are a number of species of trypanosomes but only 2 have been known to infect humans, those being T.b gambiense and T.b rhodesiense [1].
Its transmission occurs through the tsetse fly, a member of the Glossina genus, only found in regions of Sub-Saharan Africa [1]. A bite from the infected species enters the human bloodstream, allowing the parasite to colonize areas up through the lymph nodes. Once infected, the spread of the disease easily develops into the central nervous system working its way to the brain. There are two main stages early and late, the late stage results in neurological defects. Early symptoms commonly consist of headache, fever, rash, or drowsiness [1].
Infected hosts may experience differences in circadian rhythm, insomnia, drowsiness throughout the day, and eventually potential death if left untreated [1]. Those in late stages of the disease experience disturbances in their circadian rhythm, insomnia, or other psychological symptoms such as dementia, depression, mania, irritability, or memory loss [1]. If left untreated, almost all patients are left in a coma, often resulting in death.
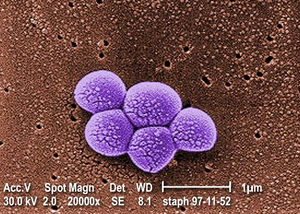
At right is a sample image insertion. It works for any image uploaded anywhere to MicrobeWiki.
The insertion code consists of:
Double brackets: [[
Filename: PHIL_1181_lores.jpg
Thumbnail status: |thumb|
Pixel size: |300px|
Placement on page: |right|
Legend/credit: Magnified 20,000X, this colorized scanning electron micrograph (SEM) depicts a grouping of methicillin resistant Staphylococcus aureus (MRSA) bacteria. Photo credit: CDC. Every image requires a link to the source.
Closed double brackets: ]]
Other examples:
Bold
Italic
Subscript: H2O
Superscript: Fe3+
Sample citations: [1]
[2]
A citation code consists of a hyperlinked reference within "ref" begin and end codes.
To repeat the citation for other statements, the reference needs to have a names: "<ref name=aa>"
The repeated citation works like this, with a forward slash.[1]
Trypanosoma Brucei
Trypanosoma brucei is an extracellular protozoan flagellate parasitic species belonging to the Trypanosoma genus, residing mainly in Sub-Saharan regions of Africa. T. brucei are frequently located extracellularly in blood and tissue regions of the mammalian host, transmitting via leech or arthropod vectors [3]. There are 3 subspecies of T. brucei, yet only 2 species, T. b. gambiense (Tbg), T. b. rhodesiense (Tbr) cause infection in humans [2]. In general, T.brucei has a larger genome than most bacteria, and is a motile bacteria.
The genome of T.brucei is 26 Mb, contains roughly 1700 variant surface glycoproteins along with around 900 pseudogenes [11]. Genome analysis has shown horizontal gene transfer allows for increased metabolic properties for trypanosome parasites [11]. T.b. gambiense is the strain mainly responsible for human infection, accounting for 98% of all diagnosed cases of african trypanosomiasis [3]. This strain is also responsible for retaining the majority of the genetic information with a smaller genome.
Virulence Factors
There are a number of cellular mechanisms, structures, and molecules that allow for full parasitic function of trypanosomes. Regarding immune response, T. brucei parasites are capable of invading a host's immune system through the use of a variable surface glycoprotein (VSG) [7]. VSGs aid in protecting these parasites from lytic factors, ultimately evading the natural host immune response. As infection is prevalent, gene conversion between VSGs occurs at the trypanosome expression site [8]. This is considered an antigenic variation which enables the parasite to avoid the body's immune response as well as continue infection throughout the host. This constant switching also has made it challenging for clinicians to develop a vaccine that trypanosomes cannot evade.
Another strategy to evade immune response is through production of serum resistance associated proteins (SRAs) [7]. SRAs are unique to T.b rhodesiense and considered members of VSGs. They are exported to the flagellar pocket of trypanosomes before getting taken up by extracellular vesicles [12]. Serum resistant forms of T.b rhodesiense express and mRNA encoding protein, associated with surface glycoproteins [12]. Presence of SRAs aid in the survival of parasites, elongating the length and path of infection in a host. SRAs have the potential to evade cell lysis, preventing the breakdown of any present trypanosomes.
An important mechanism of T. brucei parasites is their flagellum. The flagellum is essential for parasite motility, pathogenesis, transmission of infection as well as immune evasion. Their flagellum is surrounded by its own membrane and attaches by length to the trypanosome cell body [10]. This wrap-around is vital for trypanosomes to invade other tissues throughout the body, given its extracellular characteristics. Moreover, T.brucei contain a flagellar pocket which is essential for the export of VSGs to other tissues throughout the body as well as the protection of extracellular macromolecules from the host’s immune response [10]. The flagellum oversees host cell attachment through attachment plaques, allowing parasites to develop a VSG coat [10]. Once coated, parasites are released into salivary glands, unleashing infection within the host.
Epidemiology
African Sleeping Sickness, or HAT infection is limited to regions of Sub-Saharan Africa specifically. There are two strains of Trypanosoma that infect humans, each infecting separate regions of Africa. T.b. gambiense, is centered in Central and West Africa while T.b. rhodiense is found in the southern and eastern portions of Africa [3]. Poor and rural communities face an increased risk due to frequent interaction with the land and water which are breeding grounds for bacteria.
Previous epidemics of Human African Trypanosomiasis have been documented in Uganda, Congo, and Cameroon, all of which are located in Central Africa [3]. As of late, most reported cases of T.b gambiense are found in the Democratic Republic of Congo and continue to decrease at a steady rate, hovering in the low thousands [8]. Popular tourist destinations such as Kenya, Malawi, Uganda, and Zambia may also notice an increase in T.b. rhodesiense cases due to constant visitation [3]. Travelers still face an increased risk of possible infection, especially those staying in areas of wildlife and nature preserves.
Every point of information REQUIRES CITATION using the citation tool shown above.
Symptoms
\Include some current research, with at least one figure showing data.
Pathogenesis
Path of Infection
Impact on the Central Nervous System
Include some current research, with at least one figure showing data.
Diagnosis & Treatment
Diagnosis
Treatment
Prevention
Next Steps
Conclusion
References
Authored for BIOL 238 Microbiology, taught by Joan Slonczewski,at Kenyon College,2024
