Syphilis in China: Difference between revisions
No edit summary |
|||
| Line 1: | Line 1: | ||
{{Uncurated}} | |||
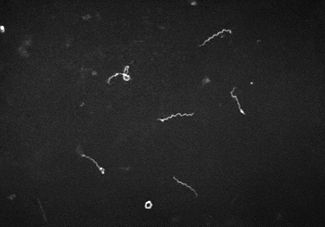
[[Image:syphilisbacteria.jpg|thumb|325x375px|I. Treponema pallidum]] | [[Image:syphilisbacteria.jpg|thumb|325x375px|I. Treponema pallidum]] | ||
Latest revision as of 15:56, 16 September 2010
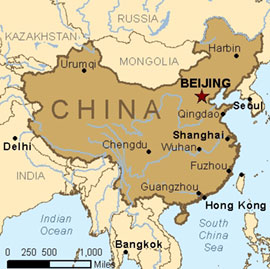
Introduction
Syphilis, a sexually transmitted disease caused by the bacterium Treponema pallidum, was first documented in China in 1505. By the 1940’s, Syphilis had become a major epidemic within China. As the communist party took over China in 1949, the political party made the disease a priority and launched a campaign in 1952 to abolish the disease [1]. Before the party launched its campaign, it was estimated that 5% of the population in large cities carried the disease. The campaign consisted of wide screening, free treatment, and a crack down on prostitution – a major factor for the spread of the disease [2]. By 1964, Syphilis had become a rarity and infection nearly eliminated, until its international borders were opened in the 1980’s [1].
A natural development of immunity towards Syphilis is possible. However, due to the fact that China had been “cleaned” of Syphilis for about 20 years after the campaign, the young sexually active generation lacked the natural immunity. This resulted in detrimental effects to China when unprotected sexual contact was made with foreigners that had the disease [1]. The disease spread over time, as sex education was practically nonexistent and public awareness of the disease dwindled. The result was a heavy resurgence of Syphilis in the late 1990’s and early 2000’s. Recent data has shown that the rate of syphilis has jumped from 0.2 cases per 100,000 people in 1993 to 5.7 per 100,000 in 2005. In even larger cities, such as Shanghai, the rate is estimated to be as high as 55 cases per 100,000 people [2]. Congenital syphilis cases, in which the disease is passed on through the mother to a newborn, are estimated to be about 3,400 a year [2].
Description of Syphilis
Syphilis is a disease caused by a spirochetal bacterium known as Treponema pallidum. “The spiral-shaped body of T. pallidum is surrounded by a cytoplasmic membrane, which is enclosed by a loosely associated outer membrane. A thin layer of peptidoglycan between the membranes provides structural stability” [4]. T. pallidum contains spirochetes that have an endoflagella which allows the bacteria to move in a corkscrew formation through the viscous fluid of the periplamic space; thus T. pallidum is a Gram Negative Bacterium.
What is interesting to note is that T. pallidum cannot live independently. It can only survive inside host cells of mammals, thus T. pallidum is an endosymbiont. Once it penetrates into the host cell, “T. pallidum derives most essential macromolecules from the host, using interconversion pathways to generate others” [4].
T. pallidum has a slow growing rate relative to other bacteria. One reason is due to the fact that T. pallidum does not contain a tricarboxylic acid cycle and an electron transport chain. So it depends only on glycolysis, which makes 2 ATP molecules per glucose. Therefore the low energy source slows the growth rate significantly. Moreover, “because of a lack of enzymes such as catalase and oxidase that detoxify reactive oxygen species, the in vitro survival of T. pallidum is prolonged by low oxygen concentration” [4].
Finally, motility of the T. pallidum depends upon adhesions and the process of chemotaxis. The bacteria use its pili as an adhesion to attach to host cells, and they use treponems in the adhesion process. Moreover, T. pallidum uses methyl accepting chemotaxis transmembrane proteins (MCPs) that “sense attractants and repellents in the environment; glucose and histidine are molecules that may have affinity for T. pallidum MCPs. Pathogenic processes such as crossing the endothelial barrier to reach the bloodstream are likely to depend upon mechanisms that allow T. pallidum to sense and respond to nutrient gradients” [4].
Syphilis’s microbe, Treponema pallidum, has very strong motility to swim through gel-like fluids; but it is a sensitive bacterium that is very dependent on its host cell to survive. If this Gram Negative Bacterium is removed from the mammalian cell it will die within hours because of the lack of nutrients that the host cell can provide.
Transmission of Syphilis
Transmission
Syphilis transmission occurs via direct contact, usually sexual, with primary or secondary lesions. Treponema pallidum, the bacterium that causes the disease, begins to spread within hours of infection and microbes can settle in a variety of tissues [4].
Stages
It is a multistage disease and the primary stage begins with the appearance of a chancre at the site of infection. The chancre can appear between 10 and 90 days after exposure and usually emerges around 3 weeks after infection. This chancre typically ulcerates, but is not painful and does not produce a discharge. Primary chancres usually appear on the penis, rectum, anal canal, oral cavity, labia, or cervix. Because some of these locations are not always visible and the chancre is painless, primary syphilis can go undetected until a later stage. Within 4 to 6 weeks of appearance the primary chancre will spontaneously heal [4].
Symptoms of secondary syphilis usually begin to develop three months after exposure to the disease. The most common materialization of secondary syphilis is a scattered rash, frequently found on the palms of the hands and soles of the feet. Other manifestations such as sore throat, muscle aches, weakness or depression, and weight loss can occur during secondary syphilis. Symptoms of secondary syphilis usually resolve naturally within three months of development [4].
In untreated individuals, syphilis can become asymptomatic after secondary syphilis symptoms have healed. This stage is called latent syphilis and it is recognized by positive serological tests for activity with absence of other manifestations of the disease [5]. Latent syphilis is described in two stages: early and late. Early latent syphilis defines the first year after infection, but an individual can enter late latent syphilis if the disease is asymptomatic beyond the first year following infection [4]. Sexual transmission is highly unlikely during the late latent syphilis. Latent syphilis ceases when treatment is administered or when symptoms of tertiary syphilis appear [4].
The tertiary phase of untreated syphilis occurs 20 -40 years after infection [4]. Three syndromes are associated with late manifestations of syphilis: gumma, cardiovascular syphilis, and late neurosphilis. In gumma, increased inflammation causes a rubber, tumor-like lesion. These lesions usually occur on the skin and bones, but can appear in internal organs, such as the liver, heart, brain, stomach, and upper respiratory tract [4]. With proper antibiotic treatment these lesions will heal. In cardiovascular syphilis, damage results from infection of the aorta and can cause an aneurysm. Before the use of penicillin treatment it was believed that the majority of deaths from syphilis occurred because of cardiovascular infection [4]. Penetration of the central nervous system can occur during the primary and secondary stages of syphilis, but neurosyphilis is most commonly associated with tertiary syphilis. A majority of individuals with invasion of the central nervous system to resolve the infection, but early attack can progress to meningovascular syphilis or late parenchymatous syphilis [4]. Manifestations of meningovascular syphilis are similar to the symptoms of meningitis caused by other diseases and are a result of inflammation of the meninges, which are the membranes that cover the brain and spinal cord [6]. Symptoms prior to diagnosis include vertigo, insomnia, personality changes, as well as loss of consciousness and seizures [4]. Late parenchymatous syphilis is an invasion of the functional tissue of the central nervous system, as opposed to connective tissue or tissue that may offer structural support. It manifests as general paresis (chronic inflammation and degeneration of cerebral tissue) or as tabes dorsalis (hardening of dorsal columns of the spinal cord). Symptoms of general paresis include personality change, emotional instability, memory impairment, hallucinations, and hyperactive reflexes. Characteristics of tabes dorsalis include loss of coordination in the lower extremities, tingling, and sudden-onset vomiting or abdominal pain [4].
Congenital Syphilis
At any time during pregnancy and at any stage of syphilis T. pallidum can infect a developing fetus. In a pregnant woman with syphilis, organisms can cross the placenta to infect the fetus. There is a higher risk for transmission when the mother is in the earlier stages of syphilis, but transmission can still occur even when the mother is the in late latent stage when sexual transmission is highly unlikely. If the pregnant woman goes untreated, spontaneous abortion, stillbirth, and premature delivery can result. If the baby survives it may be infected with syphilis, which is typically associated with a low birth rate and additional risk for pulmonary hemorrhage, secondary bacterial infection and severe hepatitis [4].
Congenital syphilis is also described in stages. The early stage is defined as manifestations within the first two years of life. The late stage describes symptoms after two years old. Early symptoms typically appear between two to 10 weeks after delivery. The early manifestations appear as severe symptoms of adult secondary syphilis and are infectious. The first development in about half of newborns infected with the microbe is a symptom called snuffles. T. pallidum invades the nasal mucosa causing inflammation, which results in a whitish discharge that occasionally also contains blood. Late congenital syphilis can result in damage to the cornea and iris, eighth nerve deafness, asymptomatic and symptomatic neurosyphilis, joint disease, and tooth deformities. Many of these developments occur even with treatment. [4]
Diagnosis and Treatment
The only definitive methods for diagnosing early syphilis are darkfield examinations and direct fluorescent antibody tests of lesion discharge or tissue, but the results of two types of serological tests can be indicative enough to diagnose syphilis. These two tests are nontreponemal, which measures antibody concentration which correlates to disease activity, and treponemal, which detects antibodies specific to T. pallidum. Both serological tests must be used in order to diagnose syphilis. Some patients infected with HIV may have unusual serological test results and biopsy or direct microscopy for a more definitive diagnosis. A diagnosis of neurosyphilis usually depends on a variety of combinations of reactive serological tests, atypical cerebrospinal fluid cell count or protein, or a reactive nontreponemal serological test of the cerebrospinal fluid [5].
The preferred treatment for all stages of the disease is benzylpenicillin administered parenterally, often through intramuscular injection. Oral preparations of penicillin are not appropriate for treating syphilis. Benzathine, aqueous procaine, or aqueous crystalline are all preparations used. The type of preparation, dosage, and duration of treatment all depend on the stage and manifestations of syphilis. Parenteral benzylpenicillin is the only treatment with documented success for treating syphilis during pregnancy. It is recommended that all women should be screened serologically for syphilis at the first prenatal visit. Maternal transmission can be prevented by treatment with penicillin and is also effective for treating fetal infection [5].
Why this Disease is a Problem in China
Since China defeated syphilis in the 1950’s, it has returned strong due to a variety of reasons. Since Mao Ze Dong’s rule, China has evolved socially, economically, and politcally. Biologically speaking, complete eradiction of the disease in earlier decades has reduced the amount of immunity for sexually active adults now (who were children at the time) [7]. This is because syphilis infection causes an immune response which reduces the possibility of re-infection in the future [8]; if they were not exposed to it at all their body has built no defense toward it.
The attitudes towards sex have also changed in that there is an increase in amount of sexual partners, extramarital relationships, and prostitution [8]. The less conservative view on sex coupled with lack of protection has contributed to the wider spread of the disease in the country. While the attitudes towards sex have changed, open communication about sexual relations hasn’t, making it difficult for patients possibly infected to be treated accordingly. Along with lack of communication to health care providers, lack of communication between sexual partners hampers spread from stopping [7].
Homosexuality once considered unacceptable in all realms is gaining momentum towards complete acceptability. In urban areas gay clubs/bars have opened and annual parades celebrate their lifestyle and culture. Studies show that the highest rates for syphilis in urban areas from China are from men having sex with men (MSM) [8].
Also feeding towards the spread is population mobility which was not feasible during Mae Ze Dong’s rule. Beginning in the late 1980’s the Chinese government started lifting travel restrictions allowing rural populations to move to cities to find work [8]. The number of rural-urban migrants went from 50 million in 1990 to 120 million in 2000, with estimates around 160 million by 2010 [8]. Although not supported by studies, it is assumed that migrants are feeding the demand for the sex industry, which leads to the spread of STD’s. Furthermore, businessmen moving into China are feeding the sex industry - a study among sex workers in brothels in Yunnan Province shows that almost all of the clients were foreign business men [8].
Lastly, a major player in the syphilis epidemic is the collapse of the universal free health care (and public health in general) in the 1970’s [8]. Currently, much of the healthcare is privatized with patients paying out of pocket. This is an issue because people possibly infected are not seeking health treatment due to lack of funds. This was demonstrated in a study done in an area outside of Beijing where 80% of women with genitourinary symptoms did not seek health care partially due to cost (in other part lack of understanding toward the severity of the problem) [8].
Overall: The symptons of syphilis can be wide ranging, often being confused with other conditions, and may also be asymptomatic, making diagnosis a particular challenge (Hesketh).
The rising rates of syphilis in China are largely attributed to factors regarding socioeconomic, educational and lifestyle issues. The current clinical guidelines for syphilis detection are based on symptomatic criteria, overlooking opportunities to assess risk factors to further improve disease control. This method does not include blood tests, such as the toluidine red unheated serum test (TRUST) and Treponema pallidum particle agglutination test (TPPA), which can detect syphilis even if an individual does not show any hallmark symptoms of the disease [9].
In Guangxi, China, a study investigating the effectiveness of a potential screening tool revealed that 40.9% of patients that tested seropositive did not show the hallmark signs of syphilis [9]. The study indicates that the current testing guidelines for syphilis are not efficient in detecting positive cases in which symptomatic signs are not visible [9]. These shortcomings are problematic due to their low efficacy rates in disease detection.
The current testing guidelines also lack behavioral risk assessment as a factor in detecting sexually transmitted diseases. In the aforementioned survey, women were less likely to disclose risk behaviors due to fear of stigma associated with sexual behaviors [9]. The shame associated with revealing such behaviors lowers the chance of discovering risk behaviors that would indicate the presence of a sexually transmitted disease.
Congenital syphilis is another major problem among pregnant women in China. In one particular area, Shenzhen, China, syphilis cases began to reappear in 1983, after having been nearly extinguished in the 1960’s. From 1996 to 2001, the number of congenital syphilis cases had risen from one to 36 reported cases. In a study in Shenzhen that screened and treated pregnant women for congenital syphilis, most of the infected pregnant women fit into specific demographics. The majority were young, had poor educational backgrounds, tended to migrate frequently, and usually worked in the commercial or service industries or were unemployed. Their lack of knowledge of STD’s, in addition to their lack of communication with the healthcare system, placed these women at high risk for congenital syphilis. In the study, 63% of mothers who had transmitted congenital syphilis had never had prenatal examinations before childbirth. Also, the fact that many of these women migrated so often lowered the chances that women would return to clinics for follow-ups, a major factor in preventing congenital syphilis and the transmission of the disease from mother to child. [10]
What is Being Done to Address this Problem
The National Center for AIDS/STD Control and Prevention in China focuses mainly on prevention and spread of HIV and AIDS [11]. Many of their funds and focus are towards controling the spread of the disease and taking precautionary measures to avoid contracting it in the first place. While STD’s are lumped along with it, infectious diseases including syphilis are over shadowed by the mass attention given to HIV and AIDS; this is not to negate the fact that some attention has been given to the disease.
Under the Laws of the People’s Republic of China there is a law on Prevention and Treatment of Infectious Diseases. Syphilis, AIDS,and other diseases such as gonorrhea are placed under the same group- Class B [12]. Under this law there are chapters on prevention and control. Under the chapter of prevention, Article 11 states: “Medical care and health institutions at various levels and of different types shall set up preventive health organizations or assign personnel to undertake the prevention and control of infectious diseases and the management of the epidemic situation in their respective units or in the communities for which they are responsible” [12] . As for Chapter IV including control, under Article 24 it says “For patients of B Class infectious diseases other than AIDS… necessary treatment and control measures shall be taken according to the patients' conditions” [12].
In the past (up until October 2003) screening for syphilis was included in a compulsory premarital examinationwhich had to be completed before marriage; since it has become voluntary and the rates for people screened dropped dramatically [8]. However, seeing how important it is one province Heilongjiang has re-introduced it as mandatory, with other provinces possibly following. Another program that was implemented recently in more rural areas includes 100% Condom Use. These were tested in the provinces: Jiangsu, Hubei, Hunan, Guangxi, and Hainan provinces, all of which showed reduction of syphilis prevalance in female sex workers – whom have sexual contact with many different men [8]. Worth mentioning is the use of tufuling or Rhizoma Smilacis Glabrae a home remedy which is used in China to treat syphilis (dating as far back to 5th century A.D.), how it treats the disease is not known [13].
Dr. Mryon S. Cohen, who has worked in China since 1979, worked in collaboration with Dr. Xiang-Sheng Chen from the National Center for STD Control in Nanjing to compile a report on the Syphilis resurgence. The compiled report provides data to let the government know where to allocate their resources. As a result, a “China Syphilis Working Group” has formed, working with the UNC, China's National Center for STD Control, the World Health Organization, the United Nations Center for Disease Control and the London School of Hygiene [1].
In July 2002, a three-year program was introduced to 61 hospitals in Shenzhen that focused on the free screening and treatment of pregnant women for syphilis. The Shenzhen Center for Disease Control and Prevention (SZCDC), conducted primary screenings using toluidine red unheated serum test (TRUST), then retested the positive results using the Treponema pallidum particle agglutination (TPPA) test. Women that tested positive were treated, and their babies were tested for congenital syphilis using the 19S-IgM FTA-Abs test [10].
The program managed the positive cases in accordance with China’s Diagnostic Criteria and Management of Syphilis guidelines as well as the US Center for Disease Control Guidelines for the Prevention and Control of Congenital Syphilis. The women that decided to terminate their pregnancies were treated with penicillin or azithromycin. Women that continued with their pregnancies were treated with benzathine benzylpenicillin or erythromycin [10].
Of the women who received intervention treatment for the prevention of mother-to-child transmission of the disease, 99.1% of potential cases were successfully prevented. By the time the program had finished, the average incidence rate of congenital syphilis cases was less than half that when the program started. The program relied partially on the political and financial support from the local government, which funded the free screening, treatment and follow-ups. The screening instruments and treatment medicines were effective and inexpensive [10].
What Else Could be Done to Address this Problem
In 1949, China experienced one of the worst syphilis epidemics, estimating that 5% of the population in large cities carried the disease. As the Communist party took power, free treatment and screening was offered for the disease. The Communist party cracked down on prostitution as well, which resulted in a near elimination of syphilis [2]. Ironically, due to the near elimination of Syphilis by the Communist party in the 1960’s, the unexposed Chinese population lacked this natural immunity, making them more susceptible to the disease [2] as their borders were opened internationally in the 1980's.
China was once successful in the eradication of syphilis but that was in a completely different social and political setting. In order for China to successfully deal with the syphilis epidemic some key changes can be made. First off, there must be commitment from politics – they already show commitment towards HIV and syphilis can be added onto the priorities for health. Political involvement in the 1950's was a crucial part to its sucess, and will need to be a crucial part now if syphilis will be controlled [8].
Moreover, syphilis detection guidelines could be greatly improved. Current guidelines for syphilis screening are based on detection through visible symptoms. Therefore, many syphilis cases remain undetected. Inexpensive screening tools, such as using surveys to assess behavioral risks, would provide a more thorough screening, thus strengthening current surveillance guidelines. Patients that do not show any physical symptoms would not normally have undergone any syphilis testing and would have been defined as non-triaged patients. Health care providers could use a simple survey to detect which non-triaged patients are still at high risk and should still undergo syphilis testing [9].
Affordable screening and free treatment played a big part in the successful eradication from the past. As stated above, the availability of healthcare and cost has deterred many from seeking screening and treatment. Also, screening of pregnant women is crucial because of congenital syphilis [8]. If the government makes healthcare more available the disease can be caught and treated before spread.
Furthermore, “the huge resources that have been allocated to free HIV voluntary counselling and testing programmes throughout the country should be extended to screen for syphilis” [8]. In China, the prevalence of syphilis is 10 times higher, the transmission faster, and the treatment effective. Since syphilis has relations to the rate of HIV spread (the presence of syphilis enhances the viral load in infected people, while also enhancing transmission of HIV), funds towards HIV should also bring into consideration syphilis which can increase infection rates [8].
Another thing the country can do to address the problem is simple: education and awareness about the disease. Education from health care providers to the general public about what it can cause if untreated, the symptoms to look out for, and encouragement to seek treatment or screening would be extremely helpful in fighting the spread. Once again, China has done a great job at HIV awareness but has provided little to no information in regards to syphilis. Promotion of condom use for high-risk groups like female sex workers, men having sex with men, and for people with multiple sex partners in general is crucial for obvious reasons [8].
Treating the disease in China is not a scientific problem, but a socio-political problem. China remains one of the most conservative countries in the world. As a result, topics of sexual intercourse are generally taboo, as well as sexually transmitted diseases [3]. To combat the vast increase within the past decade, China should reform it's educational system to include sex education. They should also publicly promote the use of protection. An entire reform from it's conservative culture is essentially required to best to address the problem. In addition, new adult screening programs should be established and antibiotics should be made easily available by the government to deal with the current syphilis outbreaks [2], as it did in 1949.
References
[1]. University of North Carolina School of Medicine. "Resurgence And Spread Of Syphilis In China Is A Rapidly Increasing Epidemic". ScienceDaily. 12 January 2007. 25 August 2009 <http://www.sciencedaily.com/releases/2007/01/070112104258.htm>.
[2]. Roxanne Khamsi. “Syphilis rates skyrocket in China”. New Scientist. 12 January 2007. 25 August 2009 <http://www.newscientist.com/article/dn10940>.
[3]. Iamseven. “Syphillis on the rise in China”. Digital Journal. Jan 11, 2007. 25 August 2009 <http://www.digitaljournal.com/article/90014>.
[4]. LaFond, Rebecca E., Lukehart, Sheila A. "Biological Basis for Syphilis". Clinical Microbiology Reviews. 2006. Volume 19. p.29-49. <http://cmr.asm.org/cgi/content/full/19/1/29>.
[5]. Levine, William C., Workowski, Kimberly A. “Sexually Transmitted Diseases Treatment Guidelines.” May 2002. Centers for Disease Control and Prevention. 24 August 2009. <http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5106a1.htm>.
[6]. "Syphilitic aseptic meningitis: MedlinePlus Medical Encyclopedia." August 2009. National Library of Medicine. 26 August 2009. <http://www.nlm.nih.gov/medlineplus/ency/article/000724.htm#Signs%20and%20tests>.
[7]. McGivering, Jill. "Syphilis Rates 'Soaring in China'." BBC News 12 JAN 2007 Web.26 Aug 2009. <http://news.bbc.co.uk/2/hi/asia-pacific/6253807.stm>.
[8]. Hesketh, T, XJ Ye, and WX Zhu. "Syphilis in China: The Great Comeback." Emerging Health Trends Journal 2008 Web.22 AUG 2009. < http://www.eht-forum.org/ehtj/journal/v1/pdf/ehtj08006a.pdf>.
[9]. Chen, Q, Cheng, F, Cohen, M, Fu, Z-Z, Gao, X, Liu, M-S, Wei,, W-H, Wong, S, Yu, Y-H. "Improving Strategies for Syphilis Control in China: Selective Testing of Sexually Transmitted Disease Patients- Too Little, Too Late?". International Journal of STD and AIDS. 2008. Volume 19. p.838-842. <http://ijsa.rsmjournals.com/cgi/content/full/19/12/838>.
[10]. Cai, Y M, Cheng, J Q, Hong, F C, Pan, P, Zhang, D, Zhang, Y J."Syphilis Screening and Intervention in 500,000 Pregnant Women in Shenzhen, the People's Republic of China." British Medical Journal. 2007. p.83, 247-250. <http://sti.bmj.com/cgi/content/full/83/5/347>.
[11]. "A Brief Introduction to the National Center for AIDS Prevention and Control, China CDC." National Center for AIDS/STD Control and Prevention, China CDC. NCAIDS. 26 Aug 2009 <http://www.chinaids.org.cn/n443289/n443290/n447111/index.html>.
[12]. "Prevention and Treatment of Infectious Diseases." Laws of the People's Republic of China . 01 SEP 1989. 26 Aug 2009 <http://www.asianlii.org/cn/legis/cen/laws/patoid454/>.
[13]. "Treatment of Syphilis with Tufuling." Leung's Chinese Herb News. 30 AUG 2007. 26 Aug 2009 <http://leungschineseherbnews.blogspot.com/2007/08/treatment-of-syphilis-with-tufuling.html>.
IMAGES:
I. phil.cdc.gov/PHIL_Images/10179/10179_lores.jpg
II. http://www.cdc.gov/flu/weekly/intsurv.htm
III. http://www.cdc.gov/Tuskegee/syphilis.htm
IV. http://www.adhb.govt.nz/newborn/teachingresources/dermatology/InfectiveLesions.htm
V. www.cdc.gov/ieip/china.html
VI. http://www.nlm.nih.gov/medlineplus/syphilis.html
VII. http://www2a.cdc.gov/ecards/cards/STDAwareness/SyphilisAwareness.jpg
Edited by Hazel Biag, Yuli Chen, Ashley Cohen, Anna Prendergast, Nicola Zenaty; students of Rachel Larsen