Tuberculosis and HIV Co-Infection: Difference between revisions
| Line 44: | Line 44: | ||
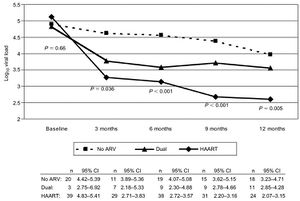
[[Image:Original.00002030-200201040-00010.FF1 (1).jpeg|thumb|300px|right|Figure 5.Mean Log10 viral load at each time point during TB treatment. ARV,antiretroviral therapy; HAART, highly active antiretroviral therapy]] | [[Image:Original.00002030-200201040-00010.FF1 (1).jpeg|thumb|300px|right|Figure 5.Mean Log10 viral load at each time point during TB treatment. ARV,antiretroviral therapy; HAART, highly active antiretroviral therapy]] | ||
One study by Dean and his colleagues investigated the risks and benefits of administering HAART during the treatment of TB. In this study a group of HIV and TB co-infected patients who being treated for TB and HIV were observed. The patients were treated for TB and also either being treated with no antiretroval viral therapy, HAART or both antiretrovial therapy and HAART. For each group of patients, Viral load and CD4 cell counts were recorded for each patient at 3,6,9 and 12 months after diagnosis(Figure 5). Treating both infections simultaneously resulted in a reduction in viral load and the greatest reduction was associated with the use of HAART. Although this reduction in viral load was observed, it is recommended that in patients with high enough CD4 levels that HIV HAART therapy be put off. This is because results of this study showed that the use of HAART in patients co- infected with HIV and TB also led to interruptions in TB treatments. The results from this study suggests HAART therapy should be used in conjunction with TB treatments only in patients who have advanced HIV. | One study by Dean and his colleagues investigated the risks and benefits of administering HAART during the treatment of TB. In this study a group of HIV and TB co-infected patients who being treated for TB and HIV were observed. The patients were treated for TB and also either being treated with no antiretroval viral therapy, HAART or both antiretrovial therapy and HAART. For each group of patients, Viral load and CD4 cell counts were recorded for each patient at 3,6,9 and 12 months after diagnosis(Figure 5). Treating both infections simultaneously resulted in a reduction in viral load and the greatest reduction was associated with the use of HAART. Although this reduction in viral load was observed, it is recommended that in patients with high enough CD4 levels that HIV HAART therapy be put off. This is because results of this study showed that the use of HAART in patients co- infected with HIV and TB also led to interruptions in TB treatments. The results from this study suggests HAART therapy should be used in conjunction with TB treatments only in patients who have advanced HIV (Dean et al. 2002) | ||
The biggest problem that is faced in the treatment of TB in patients who are HIV positive and patients who are HIV arises when patients do not take their antibiotic treatments as prescribed. If the wrong doses of medication are taken or patient stop taking the drugs before they are supposed the TB infection can return and the remaining bacteria can become resistant to the drug that they were originally treated with. When a patient begins taking medicine in order to treat tuberculosis, the symptoms will begin to disappear and sometime patients stop taking their medication regularly. This can lead to drug resistant strains of <i>M.tuberculosis</i>, which can be more difficult to treat, and requires a longer treatment period (Tuberculosis). | The biggest problem that is faced in the treatment of TB in patients who are HIV positive and patients who are HIV arises when patients do not take their antibiotic treatments as prescribed. If the wrong doses of medication are taken or patient stop taking the drugs before they are supposed the TB infection can return and the remaining bacteria can become resistant to the drug that they were originally treated with. When a patient begins taking medicine in order to treat tuberculosis, the symptoms will begin to disappear and sometime patients stop taking their medication regularly. This can lead to drug resistant strains of <i>M.tuberculosis</i>, which can be more difficult to treat, and requires a longer treatment period (Tuberculosis). | ||
Revision as of 02:38, 8 May 2014
By Michelle Picard
Introduction
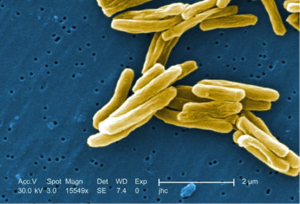
The bacteria Mycobacterium tuberculosis causes tuberculosis. Mycobacterium tuberculosis is an acid fast, rod shaped, gram-positive bacteria that has a unique cell wall compared to other gram-positive bacteria(Image 1). The cell wall of these bacteria contains mycolic acids, lipid complexes and porins to transfer materials in and out of the cell. In addition to the cell wall these bacteria do not have an outer cell membrane and have layers of arabinogalactan and peptidoglycan under the cell wall. The structure of the unique mycolic acids located in the cell wall make it difficult for nutrients to move in and out of the cell, which results in a slow growth rate compared to other bacteria (Cole,1998). M. tuberculosis mainly infects the lungs but also has the ability to spread to other areas of the body. One of the reasons that M. tuberculosis usually infects the lungs because M.tubercuolsis is an obligate aerobic and grows best under high oxygen conditions.
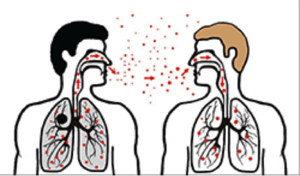
Mycobacterium tuberculosis is transferred through the air when someone a person who is infected with TB coughs or sneezes and another person inhales the contaminated air. (CDC, 2014). The tuberculosis infection can exist within the body two in different forms (Figure 2). A Tuberculosis infection is characterized as a latent infection when the body is infected by Mycobacterium tuberculosis and the body’s immune system fights the infection and is able to successfully stop the pathogen from reproducing, growing and spreading. Individuals that have the latent form of TB do not have any symptoms, do not appear to be sick, and cannot transmit the Mycobacterium tuberculosis bacteria to others. A latent TB infection has the ability to become active within the body when the immune system can no longer control the infection. An individual becomes infected with active TB when the immune system cannot stop the bacteria from multiplying inside the body. Symptoms of an active TB infection include chest pain, coughing up blood, fever, fatigue, and weight loss. Some people who come into contact with M. tuberculosis will develop an active TB infection and show symptoms quickly, while it can remain latent in others for years. In some individuals the infection will remain latent and never become active. The development of a TB infection from latent to active is a result of the immune system response of the host. Some individuals are at greater risk for developing active TB infections then others. Individuals who have with compromised immune systems or diseases that make in difficult to fight infection are at a higher risk for tuberculosis. Individuals previously had a TB infection did not get proper treatment are also at a higher risk (CDC,2014).
Immune Response to Tuberculosus
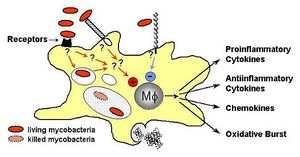
The body’s immune response when infected with Mycobacterium tuberculosis determines the effect that the bacteria will have on the host. Some individuals who are infected develop the active form of the disease while others do not. When Mycobacterium tuberculosis first enters to body, the bacteria are ingested by macrophages. The bacteria are recognized by a variety of receptors that are located on the surface of phagocytes. Some of the receptors on the phagocyte that are responsible for identifying foreign bacteria are the complement receptor 1 (CR1), Complement receptor 3 (CR3), complement receptor 4 (CR4), mannose receptor, and type A scavenger receptor. The host phagocyte has a difference response to the pathogen depending on which receptor recognizes the pathogen. If M.tuberculosis is bound by CR1 it has a better chance of survival then if it is recognized by one of the CR3 or CR4 phagocyte receptors. M. tuberculosis bacteria that are ingested by macrophages and due to recognition of surfacant protein A have an increased ability to represses nitrogen intermediates. Nitrogen intermediates are one of the many important mechanisms involved in killing bacteria that invade the host (van Crevel et al., 2002)
Toll like receptors also play a role in the recognition and ingestion of Mycobacterium tuberculosis by macrophages. Recognition by macrophages occurs through identification of the cell wall component lipoarabinomanna. Toll-like receptor 2 (TRL 2) plays an important role in the innate response by turning on certain transcription factors and signaling defenses and responses. Activation of macrophages by toll-like receptors results in the production of cytokines, which play an important role in granuloma formation. A granuloma is a cell structure that is made up of macrophages, lymphocytes, and dendritic cells. The formation of granuloma is a characteristic immune response to M. tuberculosis. The function of a granuloma is to contain the bacteria and localize the infection in order to prevent it from spreading and reproducing throughout the body by activation addition macrophages and T-cells (Schluger et al. 1998). Toll-like receptors are important because they are required for activation of the immune response. Macrophages fight against Mycobacterium tuberculosis using a variety of methods including reactive oxygen intermediates, reactive nitrogen intermediates, phagosome-lysosmes fusion, and apoptosis(Figure 3).(van Crevel et al., 2002).
CD4+ and CD8+ are the two types of T cells that are part of the immune response to TB infection. Previous studies have shown that both of these types of T-cells are important in recognizing a TB infection. CD4+ cells are responsible for recognizing infected macrophages. When an infected macrophage is found within the body CD4+ cell produce INF gamma. INF gamma can induce the expression of nitrogen and oxygen intermediates which kill that bacteria or can lead to lysis of infected cells (Pawlowski et al,. 2012). CD8+ T cells play a different role in the immune response. The job of CD8+ T cells is recognizing other cells that are infected. CD8+ cells are responsible for the lysis of these infected cells in the production of cytokines (Figure 3). (van Creval et al,. 2002).
Tuberculosis and HIV Co-Infection
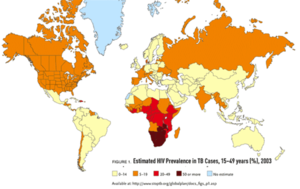
Of those infected with Mycobacterium tuberculosis, only between 10 and 20 percent will actually develop Tuberculosis and become ill. Previous studies have shown that people who are infected with HIV are 30 times more likely to develop a TB infection then individuals who do not have HIV (Pawloski et al,.2012) Even though TB is a treatable disease, it is the leading cause of death in individuals who are also infected with HIV. HIV and Tuberculosis co-infection is a serious problem in areas of the developing world where HIV affects a large percentage of the population is infected with HIV. In parts of the world where HIV is considered to epidemic, there has also been an acceleration of the tuberculosis epidemic (Karim et al,.2009). The majority of deaths that are a result of Tuberculosis occur in patients that are also infected with HIV. Efforts are being made in many areas of the developing world to increase the availability of antiretroviral drugs and decrease the number of deaths related to HIV, but if TB is not properly treated in individuals who are infected with both diseases a large number of people will continue to die from Tuberculosis. In sub Saharan areas of Africa the number of cases of tuberculosis has dramatically increased partly due to the HIV epidemic (King et al., 2006).
Risk Associated with Tuberculosis and HIV Co-Infection
TB is a major cause of death among individual who are infected with HIV. Individuals who are infected with HIV more likely to develop Tuberculosis then those who are HIV negative and they are at a greater risk to die from Tuberculosis (Diedrich et al., 2011). Individuals who are HIV positive are also more likely to develop an active TB infection that can eventually lead to death if left untreated. The effects that both of these diseases have on the body’s immune system. (Pawlowski et al., 2012).
Infection with HIV leads to a decrease in the number of CD4+ T cells in the body which significantly affects the body’s ability to fight against infection in a variety of ways. When an individual is infected with HIV T cells lose their ability to properly function in the human body. T cells can no longer produce cytokines in response to an antigen and T cells also lose the ability to control the replication of HIV. Macrophage function is also affected by HIV infection. Overall, there is down regulation of the body’s normal immune response. As previously discussed, both macrophages and CD4+ T cells play an important role in the body’s immune response to M.tuberculosis. These changes in the immune system as a result of HIV infection lead to a decrease in the ability of the body to form andorganize granulomas. Granulomas are an immune response which function to contain the growth and reproduction of M. tuberculosis. Without functional granulomas, there is an increase in bacterial growth and a M. tuberculosis infection has the ability to become active inside of the body( Diedrich et al., 2011).
The disruption of granuloma formation can lead to the activation of a TB infection because patients who are infected with HIV has a decreased number of CD4+ cells. CD4+ T cells and tumor necrosis factor are essential elements in the formation and organization of granulomas. It has been shown that HIV impairs the function of both TFN- mediated macrophage response to M. tuberculosis. Because of the role that T cells play, it is hypothesized that HIV induces active or reactivates latent tuberculosis infections by reducing the number of T-cells within the granulomas, which leads to an increase in the ability of Mycobacterium tuberculosis to replicate within the body (Schluger et al.,1998).
HIV has a significant effect on macrophage function within the granuloma. HIV can disrupt the function of macrophages within the granuloma making the body more susceptible to infection. The function of macrophages are infected by HIV can be changed so that the macrophage no longer has the ability to kill Mycobacterium tuberculosis. Macrophages are important because they are the primary immune cells in the lungs. Macrophage apoptosis plays an important role in the body’s immune response to Mycobacterium tuberculosis infection. Ex-vivo it has been demonstrated with HIV decrease macrophage response to Mycobacterium tuberculosis and HIV infection of macrophages leads to reduced apoptosis (Diedrich et al., 2011).
Research has also shown the infection with HIV and TB has negative impacts of the immune system’s ability to fight against HIV. Tuberculosis has the ability to increase HIV viral replication .HIV replication can increases in areas of M.tuberculosis infection within the body including infected macrophages because M.tuberculosis is able to create a favorable environment for HIV infection by increasing the expression of CXCR4 and CXCR5 receptors, which favor the replication of HIV. Studies also suggest that certain components of the M.tuberculosis cell wall can also aid in HIV replication through a transcriptional pathway (Pawloski et al., 2012).
Treatment of Tuberculosis in HIV patients
As Tuberculosis becomes an increasing problem in the developing areas of the world, a major concern is controlling the spread of both HIV and TB. Tuberculosis can be treated by a variety of different antibiotics. The most common antibiotics that are prescribed as part of a treatment plan to treat Tuberculosis include Isoniazid, Rifampicin, Pyrazinamide, and Ethambutol. It is easier to treat TB in patients with a latent infection because there is a smaller amount of bacteria in the body. If an individual has a active TB infection, it is harder to treat because the bacteria are multiplying and reproducing within the body. Combinations of antibiotics are usually used in order to prevent antibiotic resistant strains of M.tuberculosis from developing (Aaron et al., 2004)
In patients that are also HIV positive, treatment of an active TB is infection is the priority because Tuberculosis can easily be spread between individuals. If possible antituberculosis treatments should be given first before a patient is treated with HAART, but it a patient is at significant risk due to an extremely low CD4+ T cell count, an appropriate treatment plan needs to devised. When devising a treatment plant for TB in HIV positive patients who are being treated with HAART, possible interactions between antiretroviral drugs used to treat HIV and antibiotics must also be taken into consideration. Highly Active Antriretroviral Therapy (HAART) is the latest advancement in HIV treatment. This treatment combines multiple drugs along with nucleoside reverse transcriptase inhibitors (NRTIs) and a protease inhibitor (PI). Other risks include inflammatory reactions, suboptimal adherence and increased pill burden (Aaron et al., 2004).
Treating a patent certain antibiotics who also being treated with HAART could lead to drug-drug interactions. PIs and NRTIs are both metabolized by the same family of enzymes that are responsible for metabolizing rifampin, which is one of the antibiotics that is most commonly used to treat TB. Rifampicin is commonly used because treatment plans that include this antibiotic are much shorter, have higher cure rates and have lover rates of relapse, but problems can arise when it is used in combination with HAART (Aaron et al., 2004). An alternative antibiotic that can be used in treatment of TB in HIV positive patients who are being treated with HARRT is rifabutin. One issue with rifabutin being used as an antituberculosis treatment is that there is increased risk of Tuberculosis relapse in patients treated with rifabutin compared to those treated with rifampicin. Other antibiotics that are used to treat TB do not appear to interact with antiretroviral drugs. An appropriate treatment plan must be created based on a patient-to-patient basis (Aaron et al., 2004). This treatment plan is dependent of the T cell count of the patient and a variety of other factors. In some cases, it may be most beneficial to hold off on HARRT treatment while the Tuberculosis. In other cases, patients T cell maybe too low and the individual may not be able to have an untreated HIV infection.
One study by Dean and his colleagues investigated the risks and benefits of administering HAART during the treatment of TB. In this study a group of HIV and TB co-infected patients who being treated for TB and HIV were observed. The patients were treated for TB and also either being treated with no antiretroval viral therapy, HAART or both antiretrovial therapy and HAART. For each group of patients, Viral load and CD4 cell counts were recorded for each patient at 3,6,9 and 12 months after diagnosis(Figure 5). Treating both infections simultaneously resulted in a reduction in viral load and the greatest reduction was associated with the use of HAART. Although this reduction in viral load was observed, it is recommended that in patients with high enough CD4 levels that HIV HAART therapy be put off. This is because results of this study showed that the use of HAART in patients co- infected with HIV and TB also led to interruptions in TB treatments. The results from this study suggests HAART therapy should be used in conjunction with TB treatments only in patients who have advanced HIV (Dean et al. 2002)
The biggest problem that is faced in the treatment of TB in patients who are HIV positive and patients who are HIV arises when patients do not take their antibiotic treatments as prescribed. If the wrong doses of medication are taken or patient stop taking the drugs before they are supposed the TB infection can return and the remaining bacteria can become resistant to the drug that they were originally treated with. When a patient begins taking medicine in order to treat tuberculosis, the symptoms will begin to disappear and sometime patients stop taking their medication regularly. This can lead to drug resistant strains of M.tuberculosis, which can be more difficult to treat, and requires a longer treatment period (Tuberculosis).
Co-Infection in South Africa
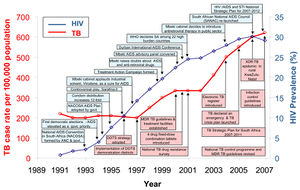
Historically, one area of the world that has been particularly affected by both HIV and TB epidemics in South Africa (Figure 4).South Africa has one of the highest numbers of individuals infected with HIV living in a single area. Tuberculosis was first introduced to South Africa by European immigrants who were infected with Mycobacterium tuberculosis. Social, Economic, and Environmental conditions have led to the spread of both TB and HIV throughout South Africa.The migrant worker system which resulted in thousands of workers living in crowded areas created an environment which increased the spread of TB and a variety of sexually transmitted diseases ( Karim et al. 2009).Lack of government response to TB and HIV has created problems in controlling the spread of these diseases (Figure 5).Currently,South Africa is considered to be the area of the world which is experiencing on the worst Tuberculosis and HIV epidemics The presence of these two diseases in this area has led to a large number of deaths due to co-infection. In addition, an increasing rate of antibiotic resistant strains of Mycobacterium tuberculosis has also been observed in areas of South Africa (Gandhi et al., 2006).
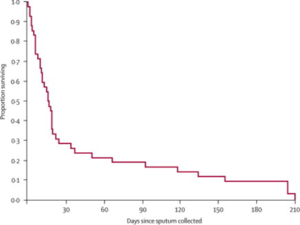
A study was conducted in KwaZulu Natal, South Africa with the purpose of determining how prevalent antibiotic resistant strains of Mycobacterium tuberculosis are the area and the way in which antibiotic resistant strains effect patients who are also HIV positive. In this area, there is a government sponsored TB treatment program that uses a strategy determined by the World Health Organization. Extensively resistant TB (XDR-TB) was prevalent among patients who were HIV positive and was fatal in 98% of cases. More than half of the patients who suffered from (XDR-TB) were never treated for tuberculosis before meaning that these patients did not develop the resistant form of TB as a result of failed treatment or issues with the proper use of prescribed antibiotics. The rise of drug resistant strains of Mycobacterium tuberculosis is an issue in this area of the world because of the number of individuals who are infected with HIV and the issues that are associated with TB and HIV co-infection. Individuals who are co-infected with HIV and TB who are being treated with antiretroviral drugs and antituberculosis have an increased chance of survival but, treatment is less likely to increase survival rates in individuals that contract drug resistant Tuberculosis. Drugs that are needed to treat XDR-TB are not available or have limited availability in most areas of the developing world and there are limited drugs available that can still be used to treat XDR-TB (Gandhi et al., 2006).
References
Aaron, L., Saadoun, D., Calatroni, I., Launay, O., Memain, N., Vincent, V., ... & Lortholary, O. (2004). Tuberculosis in HIV‐infected patients: a comprehensive review. Clinical microbiology and infection, 10(5), 388-398.
"Centers for Disease Control." Tuberculosis (TB). Centers for Disease Control and Prevention, 30 Apr. 2014. Web. 05 May 2014.
Cole, S., Brosch, R., Parkhill, J., Garnier, T., Churcher, C., Harris, D., ... & Barrell, B. G. (1998). Deciphering the biology of Mycobacterium tuberculosis from the complete genome sequence. Nature, 393(6685), 537-544.
Dean, G. L., Edwards, S. G., Ives, N. J., Matthews, G., Fox, E. F., Navaratne, L., ... & Pozniak, A. L. (2002). Treatment of tuberculosis in HIV-infected persons in the era of highly active antiretroviral therapy. Aids, 16(1), 75-83.
Diedrich, C. R., & Flynn, J. L. (2011). HIV-1/mycobacterium tuberculosis coinfection immunology: how does HIV-1 exacerbate tuberculosis?. Infection and immunity, 79(4), 1407-1417.
Gandhi, N. R., Moll, A., Sturm, A. W., Pawinski, R., Govender, T., Lalloo, U., ... & Friedland, G. (2006). Extensively drug-resistant tuberculosis as a cause of death in patients co-infected with tuberculosis and HIV in a rural area of South Africa. The Lancet, 368(9547), 1575-1580.
Karim, S. S. A., Churchyard, G. J., Karim, Q. A., & Lawn, S. D. (2009). HIV infection and tuberculosis in South Africa: an urgent need to escalate the public health response. the Lancet, 374(9693), 921-933.
King, Liza, and Shama Desai Ahuja. "TB and HIV Coinfection: Current Trends, Diagnosis and Treatment Update."Physicians Research Network . http://www.prn.org/index.php/coinfections/article/tb_hiv_coinfection_treatment_80, n.d. Web. 21 Apr. 2014. <http://www.prn.org/index.php/coinfections/article/tb_hiv_coinfection_treatment_80>.
"Mycobacterium tuberculosis."MicrobeWiki. Kenyon College, 3 Dec. 2012. Web. 21 Apr. 2014. <https://microbewiki.kenyon.edu/index.php/Mycobacterium_tuberculosis>.
Pawlowski, A., Jansson, M., Sköld, M., Rottenberg, M. E., & Källenius, G. (2012). Tuberculosis and HIV co-infection. PLoS pathogens, 8(2).
Schluger, N. W., & Rom, W. N. (1998). The host immune response to tuberculosis. American journal of respiratory and critical care medicine, 157(3), 679-691.
van Crevel, R., Ottenhoff, T. H., & van der Meer, J. W. (2002). Innate immunity to Mycobacterium tuberculosis. Clinical microbiology reviews, 15(2), 294