Hookworm: Difference between revisions
No edit summary |
No edit summary |
||
| Line 63: | Line 63: | ||
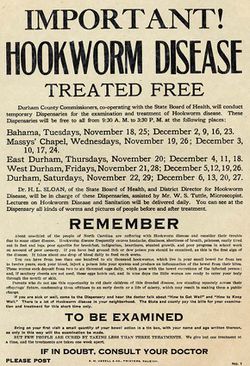
In 1910, nearly 40% of the southern US was infected with hookworm. Some even say hookworm contributed to the stereotype of southerners as lazy [[#References|[5]]]. The Rockefeller foundation launched the Rockefeller Sanitary Commission. The 5 year-program focused on eliminating hookworm in the south. They had three goals, to educate southerners on the spread of hookworm, to treat the infected, to encourage wearing shoes and to build sanitary outhouses [[#References|[5]]]. Within 5 years the program was a success-- nearly eradicating the hookworm in eleven states. | In 1910, nearly 40% of the southern US was infected with hookworm. Some even say hookworm contributed to the stereotype of southerners as lazy [[#References|[5]]]. The Rockefeller foundation launched the Rockefeller Sanitary Commission. The 5 year-program focused on eliminating hookworm in the south. They had three goals, to educate southerners on the spread of hookworm, to treat the infected, to encourage wearing shoes and to build sanitary outhouses [[#References|[5]]]. Within 5 years the program was a success-- nearly eradicating the hookworm in eleven states. | ||
[[File:hookworm_treated.jpeg|thumb|250px|right| | [[File:hookworm_treated.jpeg|thumb|250px|right|Hookworm sanitary commission flier. [http://docsouth.unc.edu/nc/hookworm/image.jpg]]] | ||
==Host Immune response== | ==Host Immune response== | ||
The larval sheath antigens are immunogenic. Most larvae cast off their outer sheath upon penetration. Potentially, diverting the immune response away from the larvae [[#References|[6]]]. In a study with infected individuals all five human immunoglobuilin isotypes were found in response to larvae and adult hookworm antigens. However, the responses varied in larval antigens. Detection of IgE antibodies against ‘’necator’’ proved to be a highly specific test for diagnosing hookworm infection [[#References|[6]]]. Adult hookworms induce the production of IgE, IgG and IgM, but not IgA[[#References|[7]]]. | The larval sheath antigens are immunogenic. Most larvae cast off their outer sheath upon penetration. Potentially, diverting the immune response away from the larvae [[#References|[6]]]. In a study with infected individuals all five human immunoglobuilin isotypes were found in response to larvae and adult hookworm antigens. However, the responses varied in larval antigens. Detection of IgE antibodies against ‘’necator’’ proved to be a highly specific test for diagnosing hookworm infection [[#References|[6]]]. Adult hookworms induce the production of IgE, IgG and IgM, but not IgA[[#References|[7]]]. | ||
Revision as of 16:53, 29 July 2014


Etiology/Bacteriology
Taxonomy
| Domain = Eukaryota | Phylum = Nematoda | Class = Secernentea | Order = Strongylida | Family = Ancylostomatidae | Genus = Necator/ Ancylostoma | species = [[ N. americanus/ A. duodenale]] [1,2].
Description

The hookworm is a soil-transmitted helminth that is common in many third world and developing countries[3]. There are several types of hookworms that infect dogs, cats and other mammals. However, there are only two species that typically infect human beings— N. americanus and A. duodenale[4]. Hookworms are located in areas with warm, moist climates. Most people with hookworm infections have no symptoms. In some cases, the worms' voracious appetite for blood can lead to anemia and protein loss[3]. The loss of vital nutrients for a third world inhabitant reduces the ability to fight future infections. While mortality from hookworm is low-- hookworm-related deaths are under-recognized. Additionally, severe anemia can retard childhood development. Malnutrition from hookworm infection can cause low levels of hemoglobin, causing vigorous labor to be impossible. [3].
Pathogenesis
Transmission
An infected human being will have eggs in their stool[4]. Under favorable conditions, 20-30°C, the larvae will hatch and mature in 5 to 10 days. Once the larvae have matured to the third-larval stage or L3, they can invade the epithelium[7]. During the L3 stage the hooworm is about 600 microns in length. Under the apporiate growth conditions the hookworm will remain alive for weeks in the soil. If another human walks barefoot on the soil where the larvae reside, they can become infected [4]. After 5 or more minutes of skin contact the larvae will penetrate the skin [3].
Infectious dose, incubation, and colonization
As little as ten hookworms can infect a host [9]. After entering the skin larvae penetrate the blood vessels and are carried to the lungs where they penetrate into the pulmonary alveoli [3]. Afterwards, they ascend the bronchial tree and are then swallowed and attach to the small intestine. Where they remain and produce eggs that are excreted out of the host. During this time, the hookworms excrete chemicals that allow them to travel throughout the body—as well as avoid the immune response. N. americanus can only infect by penetration of the host skin. Unlike N. americanus, A. duodenale can be ingested and still infect the host.
Virulence Factor
Eggs are only able to hatch under the correct conditions. They require damp soil and an optimal temperature of 20-30°C [4]. While the larvae are able to penetrate skin they still need at least 5 minutes to fully penetrate into the host. The hookworm is able to survive the brief amount of time it takes for it to travel to the small intestine.
A. duodenale can also infect by means of ingestion[3].
N. americanus can only infect through the skin.
Buccal capsule of an adult A duodenale develops a buccal capsule during migration from the lungs[3]. The capsule allows the worm to attach to the mucosal later of the small intestine. Instead of a buccal plate, N. americanus uses cutting plates to attach to the small intestine. During attachment tissue can be destroyed. Hyaluronidase is excreted by adult worms. This erodes blood vessels, providing blood for the hookworm. They also excrete an anticoagulant that facilitates blood flow.
Adult worms are also able to use factors, such as neutrophil inhibitory factor, to protect themselves from the host defenses.
Neither of the hookworm species multiply inside of the host. The natural life span for A. duodenale is 1 year and for N. americanus about 3-5 years.
Epidemiology
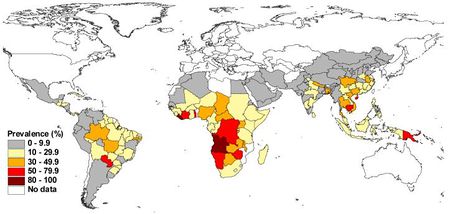
Around 500-750 million people in the world are infected with hookworm [4]. Third world countries' higher rates of poor sanitation and lack of access to clean water facilitates the prevalence of hookworm infection.In certain areas prevalence of hookworm infection can be 90%[3]. Agricultural laborers are at a high risk for hookworm—especially in areas where human feces is in fertilizer.
Clinical Features
Diagnosis
The standard method for diagnosis is looking for the presence of eggs in a stool sample. A concentration procedure is recommended, because eggs are hard to find in a light infection [4]. A rash during initial infection of the palms and soles can persist 1-2 weeks after initial infection [3]. When the worms enter the lungs-- coughing and wheezing as well as bronchoconstriction may be observed. For later infections, signs of anemia, chlorosis, hypothermia, spooning nails, or tachycardia may indicate hookworm. Intense infections can produce acute gastrointestinal hemorrhage, severe acute anemia and congestive heart failure. Children with infection typically are less productive in school. Children may also have stunted growth, due to the chronic iron-deficiency.
Treatment
Mortality is extremely low with hookworm infection. With proper nutrition during the infection, symptoms are minimal. For classic hookworm disease appropriate treatment is anthelmintic drugs [3]. Treatments that may be used are—Albendazole single 400-mg does for 3 days, Mebendazole 100 mg twice daily for 3 days, pyrantel pamoate in several 11 mg/kg doses over 3 days.
Prevention
The best way to avoid hookworm infection is to avoid walking barefoot in areas where hookworm infection is common. The avoidance of walking on human fecal material and improving the sewage disposal systems can reduce the risks of hookworm infection.
In 1910, nearly 40% of the southern US was infected with hookworm. Some even say hookworm contributed to the stereotype of southerners as lazy [5]. The Rockefeller foundation launched the Rockefeller Sanitary Commission. The 5 year-program focused on eliminating hookworm in the south. They had three goals, to educate southerners on the spread of hookworm, to treat the infected, to encourage wearing shoes and to build sanitary outhouses [5]. Within 5 years the program was a success-- nearly eradicating the hookworm in eleven states.
Host Immune response
The larval sheath antigens are immunogenic. Most larvae cast off their outer sheath upon penetration. Potentially, diverting the immune response away from the larvae [6]. In a study with infected individuals all five human immunoglobuilin isotypes were found in response to larvae and adult hookworm antigens. However, the responses varied in larval antigens. Detection of IgE antibodies against ‘’necator’’ proved to be a highly specific test for diagnosing hookworm infection [6]. Adult hookworms induce the production of IgE, IgG and IgM, but not IgA[7].
Typical immune responses for hookworm is similar to other helminths. The response is dominated by the production of Th2, IL-4, IL-5, IL-9, IL-10 and IL-13. This is consistent with the development of strong IgE, eosinophil and mast cell responses[7].
References
1. N americanus genome. http://www.ncbi.nlm.nih.gov/genome/?term=N+americanus
2. NCBI. http://www.ncbi.nlm.nih.gov/Taxonomy/Browser/wwwtax.cgi?name=Necator+americanus
3. Medscape. Hookworm. http://emedicine.medscape.com/article/218805-overview#aw2aab6b2b6
4. CDC. Hookworm. http://www.cdc.gov/parasites/Hookworm/
5. Eradicating Hookworm. http://www.rockefeller100.org/exhibits/show/health/eradicating-hookworm
6. Immune response in Hookworm Infections. Alex Loukas and Paul Prociv. Clinical Microbiology reviews. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC89000/
7. Human Hookworm Infection in the 21st century. Brooker, Simon. Jeeffrey Bethony and Peter J. Hotez. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2268732/#R79
8. Soil-transmitted helminth infections: updating the global picture. de Silva, Nilathi R, Simon Brooker, Peter J Hotez, Antonio Monstresor, Dirk Engels, Lorenzo Savioli. http://www.sciencedirect.com.ezproxy.lib.ou.edu/science/article/pii/S1471492203002757
9. Dose-ranging study for trials of therapeutic infection with Necator americanus in humans. Mortimer, K Brosm A, Feary J, Jagger C, Lewis S, Antoniak M, Pritchard D, Britton J. http://www.ncbi.nlm.nih.gov/pubmed/17123987
