Effects of Scleroderma on Human Microbiome: Difference between revisions
No edit summary |
No edit summary |
||
| Line 3: | Line 3: | ||
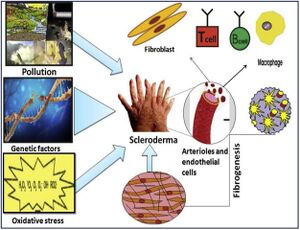
Scleroderma (or systemic sclerosis) is an autoimmune rheumatological disorder in which hardening of the skin and other organs occurs through increased amounts of collagen in the skin. <ref>[https://reader.elsevier.com/reader/sd/pii/S0928468018303924?token=8F02A57093F6C8AE3F082EBD1B190C612F7F84CDF702F29BD6BE6A3BF5D1AFB5E60593EDF69565862C3C69E54EEDAFBA&originRegion=us-east-1&originCreation=20211106180118=PDF Singh, Deependra, Arun KS Parihar, Satish Patel, Shikha Srivastava, Prakriti Diwan, and Manju R. Singh. 2019. “Scleroderma: An Insight into Causes, Pathogenesis and Treatment Strategies.” <i>Pathophysiology</i> 26 (2): 103–14.] </ref> Additionally, there are significant impacts on the vascular system by this hardening. There are two types of scleroderma, localized and systemic. Localized is when the hardening occurs exclusively in the skin and muscular tissues. Systemic occurs when the hardening is widespread throughout many organs in the body. Additionally, there are a variety of factors suggested in the pathogenesis of scleroderma, namely, environmental, genetic, and oxidative stressors. Further, sex is known to be a major risk factor for scleroderma and autoimmune disorders in general, with autoimmune disorders occurring in those of the female sex at double the frequency. <ref> [https://www.cureus.com/articles/31952-the-prevalence-of-autoimmune-disorders-in-women-a-narrative-review=PDF Angum, Fariha, Tahir Khan, Jasndeep Kaler, Lena Siddiqui, and Azhar Hussain. 2020. “The Prevalence of Autoimmune Disorders in Women: A Narrative Review.” Cureus, May.]</ref> A potential cause of these sex disparities is the difference in the human microbiome between the sexes. It has been noted that autoimmunity is able to be characterized by changes in the gut microbiome. Moreover, these changes occur more frequently in the female sex.<ref>[https://reader.elsevier.com/reader/sd/pii/S1521661615001576?token=4EFC97E26924F1784391E11D7B4489E5542AC39C7ED230D27CDF381936DD35E609E6302A465443F0DE5BCD10AF13A26C&originRegion=us-east-1&originCreation=20211106181020 Gomez, Andres, David Luckey, and Veena Taneja. 2015. “The Gut Microbiome in Autoimmunity: Sex Matters.” <i>Clinical Immunology</i> 159 (2): 154–62.]</ref><br><br> | Scleroderma (or systemic sclerosis) is an autoimmune rheumatological disorder in which hardening of the skin and other organs occurs through increased amounts of collagen in the skin. <ref>[https://reader.elsevier.com/reader/sd/pii/S0928468018303924?token=8F02A57093F6C8AE3F082EBD1B190C612F7F84CDF702F29BD6BE6A3BF5D1AFB5E60593EDF69565862C3C69E54EEDAFBA&originRegion=us-east-1&originCreation=20211106180118=PDF Singh, Deependra, Arun KS Parihar, Satish Patel, Shikha Srivastava, Prakriti Diwan, and Manju R. Singh. 2019. “Scleroderma: An Insight into Causes, Pathogenesis and Treatment Strategies.” <i>Pathophysiology</i> 26 (2): 103–14.] </ref> Additionally, there are significant impacts on the vascular system by this hardening. There are two types of scleroderma, localized and systemic. Localized is when the hardening occurs exclusively in the skin and muscular tissues. Systemic occurs when the hardening is widespread throughout many organs in the body. Additionally, there are a variety of factors suggested in the pathogenesis of scleroderma, namely, environmental, genetic, and oxidative stressors. Further, sex is known to be a major risk factor for scleroderma and autoimmune disorders in general, with autoimmune disorders occurring in those of the female sex at double the frequency. <ref> [https://www.cureus.com/articles/31952-the-prevalence-of-autoimmune-disorders-in-women-a-narrative-review=PDF Angum, Fariha, Tahir Khan, Jasndeep Kaler, Lena Siddiqui, and Azhar Hussain. 2020. “The Prevalence of Autoimmune Disorders in Women: A Narrative Review.” Cureus, May.]</ref> A potential cause of these sex disparities is the difference in the human microbiome between the sexes. It has been noted that autoimmunity is able to be characterized by changes in the gut microbiome. Moreover, these changes occur more frequently in the female sex.<ref>[https://reader.elsevier.com/reader/sd/pii/S1521661615001576?token=4EFC97E26924F1784391E11D7B4489E5542AC39C7ED230D27CDF381936DD35E609E6302A465443F0DE5BCD10AF13A26C&originRegion=us-east-1&originCreation=20211106181020 Gomez, Andres, David Luckey, and Veena Taneja. 2015. “The Gut Microbiome in Autoimmunity: Sex Matters.” <i>Clinical Immunology</i> 159 (2): 154–62.]</ref><br><br> | ||
[[Image:Scleroderma Pathogenesis Image.jpg|thumb|300px|left|A diagram of potential mechanisms for the development of scleroderma. Shown are pollution, genetic factors, and oxidative stress.[https://www.researchgate.net/publication/333197287_Scleroderma_An_insight_into_causes_pathogenesis_and_treatment_strategies] | [[Image:Scleroderma Pathogenesis Image.jpg|thumb|300px|left|A diagram of potential mechanisms for the development of scleroderma. Shown are pollution, genetic factors, and oxidative stress.[https://www.researchgate.net/publication/333197287_Scleroderma_An_insight_into_causes_pathogenesis_and_treatment_strategies]]] | ||
| Line 12: | Line 12: | ||
==Microbiome== | ==Microbiome== | ||
It has been observed specifically in the GI tract that scleroderma symptoms are associated with a change in the gut microbiome.<ref>[https://doi.org/10.1016/j.berh.2021.101687 Tan, Tze Chin, Maria Noviani, Ying Ying Leung, and Andrea Hsiu Ling Low. 2021. “The Microbiome and Systemic Sclerosis: A Review of Current Evidence.” <i>Best Practice and Research: Clinical Rheumatology.</i> Bailliere Tindall Ltd.]</ref>In studies of scleroderma patients’ gut microbiomes who displayed the SSc GI tract phenotype (scleroderma patients with GI symptoms), increased levels of <i>Fusobacterium</i> and <i>Prevotella</i> were observed.<ref>[https://doi.org/10.1002/art.39572 Volkmann, Elizabeth R., Yu Ling Chang, Nashla Barroso, Daniel E. Furst, Philip J. Clements, Alan H. Gorn, Bennett E. Roth, et al. 2016. “Association of Systemic Sclerosis with a Unique Colonic Microbial Consortium.” <i>Arthritis and Rheumatology</i> 68 (6): 1483–92.]</ref> This suggests that the gut microbiome contributes to the development of the SSc GI tract phenotype. Moreover, due to the established link between <i>Prevotella</i> in the gut and diet, it is suggested that dietary changes to lower the levels of <i>Prevotella</i> in the gut microbiome might reduce the effects of the SSc GI tract phenotype.<br><br> | It has been observed specifically in the GI tract that scleroderma symptoms are associated with a change in the gut microbiome.<ref>[https://doi.org/10.1016/j.berh.2021.101687 Tan, Tze Chin, Maria Noviani, Ying Ying Leung, and Andrea Hsiu Ling Low. 2021. “The Microbiome and Systemic Sclerosis: A Review of Current Evidence.” <i>Best Practice and Research: Clinical Rheumatology.</i> Bailliere Tindall Ltd.]</ref>In studies of scleroderma patients’ gut microbiomes who displayed the SSc GI tract phenotype (scleroderma patients with GI symptoms), increased levels of <i>Fusobacterium</i> and <i>Prevotella</i> were observed.<ref>[https://doi.org/10.1002/art.39572 Volkmann, Elizabeth R., Yu Ling Chang, Nashla Barroso, Daniel E. Furst, Philip J. Clements, Alan H. Gorn, Bennett E. Roth, et al. 2016. “Association of Systemic Sclerosis with a Unique Colonic Microbial Consortium.” <i>Arthritis and Rheumatology</i> 68 (6): 1483–92.]</ref> This suggests that the gut microbiome contributes to the development of the SSc GI tract phenotype. Moreover, due to the established link between <i>Prevotella</i> in the gut and diet, it is suggested that dietary changes to lower the levels of <i>Prevotella</i> in the gut microbiome might reduce the effects of the SSc GI tract phenotype.<br><br> | ||
[[Image:Prevotella22.jpg|thumb|300px|right|A rendering of <i>Prevotella</i> bacteria.[https://www.ecured.cu/images/thumb/b/b0/Prevotella.jpg/260px-Prevotella.jpg]]] | |||
==Conclusion== | ==Conclusion== | ||
Revision as of 21:31, 14 November 2021
Introduction
Scleroderma (or systemic sclerosis) is an autoimmune rheumatological disorder in which hardening of the skin and other organs occurs through increased amounts of collagen in the skin. [1] Additionally, there are significant impacts on the vascular system by this hardening. There are two types of scleroderma, localized and systemic. Localized is when the hardening occurs exclusively in the skin and muscular tissues. Systemic occurs when the hardening is widespread throughout many organs in the body. Additionally, there are a variety of factors suggested in the pathogenesis of scleroderma, namely, environmental, genetic, and oxidative stressors. Further, sex is known to be a major risk factor for scleroderma and autoimmune disorders in general, with autoimmune disorders occurring in those of the female sex at double the frequency. [2] A potential cause of these sex disparities is the difference in the human microbiome between the sexes. It has been noted that autoimmunity is able to be characterized by changes in the gut microbiome. Moreover, these changes occur more frequently in the female sex.[3]
Genetics
Include some current research, with at least one image.
Microbiome
It has been observed specifically in the GI tract that scleroderma symptoms are associated with a change in the gut microbiome.[4]In studies of scleroderma patients’ gut microbiomes who displayed the SSc GI tract phenotype (scleroderma patients with GI symptoms), increased levels of Fusobacterium and Prevotella were observed.[5] This suggests that the gut microbiome contributes to the development of the SSc GI tract phenotype. Moreover, due to the established link between Prevotella in the gut and diet, it is suggested that dietary changes to lower the levels of Prevotella in the gut microbiome might reduce the effects of the SSc GI tract phenotype.

Conclusion
Overall text length (all text sections) should be at least 1,000 words (before counting references), with at least 2 images.
Include at least 5 references under References section.
References
- ↑ Singh, Deependra, Arun KS Parihar, Satish Patel, Shikha Srivastava, Prakriti Diwan, and Manju R. Singh. 2019. “Scleroderma: An Insight into Causes, Pathogenesis and Treatment Strategies.” Pathophysiology 26 (2): 103–14.
- ↑ Angum, Fariha, Tahir Khan, Jasndeep Kaler, Lena Siddiqui, and Azhar Hussain. 2020. “The Prevalence of Autoimmune Disorders in Women: A Narrative Review.” Cureus, May.
- ↑ Gomez, Andres, David Luckey, and Veena Taneja. 2015. “The Gut Microbiome in Autoimmunity: Sex Matters.” Clinical Immunology 159 (2): 154–62.
- ↑ Tan, Tze Chin, Maria Noviani, Ying Ying Leung, and Andrea Hsiu Ling Low. 2021. “The Microbiome and Systemic Sclerosis: A Review of Current Evidence.” Best Practice and Research: Clinical Rheumatology. Bailliere Tindall Ltd.
- ↑ Volkmann, Elizabeth R., Yu Ling Chang, Nashla Barroso, Daniel E. Furst, Philip J. Clements, Alan H. Gorn, Bennett E. Roth, et al. 2016. “Association of Systemic Sclerosis with a Unique Colonic Microbial Consortium.” Arthritis and Rheumatology 68 (6): 1483–92.
Edited by Andrew Van Horn, student of Joan Slonczewski for BIOL 116 Information in Living Systems, 2021, Kenyon College.
