Smallpox and Anthrax as Agents of Bioterrorism: Difference between revisions
| Line 51: | Line 51: | ||
<br> | <br> | ||
According to the CDC, smallpox is labeled as one of the most dangerous potential agents of bioterrorism in the world.<ref name=s3></ref> It earns this title because of the agent's ease of transmission, the world population's lack of immunity, and the speed of spread from one infected person to another.<ref name=s12>[https://www.sciencedirect.com/science/article/abs/pii/S016635420200195X?casa_token=BAEEGzZOu1QAAAAA:jxDQksNJlx34KwNixNQR0UV6v2aAMlqQRAzTNSdddhULo97VugZPdM6YqsVLmW8w00j6Fq-DwQ Whitley, R. (2003). Smallpox: a potential agent of bioterrorism. Science Direct, 57(1-2). | According to the CDC, smallpox is labeled as one of the most dangerous potential agents of bioterrorism in the world.<ref name=s3></ref> It earns this title because of the agent's ease of transmission, the world population's lack of immunity, and the speed of spread from one infected person to another.<ref name=s12>[https://www.sciencedirect.com/science/article/abs/pii/S016635420200195X?casa_token=BAEEGzZOu1QAAAAA:jxDQksNJlx34KwNixNQR0UV6v2aAMlqQRAzTNSdddhULo97VugZPdM6YqsVLmW8w00j6Fq-DwQ Whitley, R. (2003). Smallpox: a potential agent of bioterrorism. Science Direct, 57(1-2). | ||
]</ref> It is theoretically possible to artificially make a variola major from confirmed and published gene sequences. The technology exists for creation of live poxviruses from existing genetic material fragments. | ]</ref> It is theoretically possible to artificially make a variola major from confirmed and published gene sequences. The technology exists for creation of live poxviruses from existing genetic material fragments. An instance of smallpox bioterrorism occurred in the 1700’s when the British and French invaders gave Native Americans blankets that were contaminated with smallpox, when the Natives were not compliant with the European’s expansion westward. Additionally, during the time of World War Two, America, Japanese, British and Soviet researchers all looked into producing smallpox as a biological weapon. | ||
<br> | <br> | ||
<br><b>Population immunity</b> | <br><b>Population immunity</b> | ||
Revision as of 01:20, 17 April 2023
Introduction to Bioterrorism
By Emily Rogers
Bioterrorism is defined as using “using biological agents to inflict disease and/ or death on humans, animals or plants, and motivations for pursuing such an attack could have religious, political, or criminal motivations.”[1] People that plan and perform bioterrorism attacks could also be a part of nationalist, separatist, or apocalyptic cult groups.[2] Biological agents can also be used by military and government agencies in warfare.[2] Early records of bioterrorism in the 14th century include the Tartar group attacking the city Kaffa by catapulting cadavers infected with the plague, caused by the bacteria Yersinia pestis, over the walls of the city, causing the plague to spread over the Mediterranean.[2] More recently in 1984, a cult following the Rajneeshee movement poisoned a restaurant in Oregon with Salmonella bacteria because they had political motives to win an election.[2] Unlike other types of terror attacks, bioterrorism has the unique ability to go undetected for a severe length of time, in which infected individuals can spread the agent even further, before the attack event is even detected.[2]
Starting in 2001 and last reviewed in 2018, the Centers for Disease Control and Prevention (CDC) has published a list of the most dangerous infectious agents that could be used for bioterrorism acts.[3]
Starting in 2001 and last reviewed in 2018, the Centers for Disease Control and Prevention (CDC) has published a list of the most dangerous infectious agents that could be used for bioterrorism acts.[3] The list is organized into three classes of identification, category A, category B, and category C. In this ranking system, category A contains a list of diseases and biological agents which are perceived to pose the biggest bioterrorism threat to the United States. Category A biological agents consist of those which fit the four following characteristics: they are easily transmitted between people, result in high mortality rates, could cause high levels of community panic, or require special or additional public health measures for treatment and preparedness. Category B biological agents are those which are less easy to disseminate than agents in category A, but still are moderately easy to transmit. They have low mortality rates, but high morbidity rates. They require specific enhanced action from the CDC’s current capacity and disease surveillance. Category C biological agents are the third priority behind categories A and B. They are emerging agents that have the potential to be developed and used for a bioterrorism attack. They have the potential to be available, easy to produce and disseminate, and have the potential to have a serious impact on the public health of populations. The goal of having these lists of potential infectious agents for bioterror attacks is to educate and prepare medical professionals and the population before the event that an attack occurs.[3] The goal of this list is awareness of the biological agents that the United States healthcare system should be prepared to fight against.[3] Two of the Category A agents that will be discussed on this page are Bacillus anthracis, which the bacterium that causes anthrax disease, and Variola major, which is the virus that causes smallpox disease.
The insertion code consists of:
Double brackets: [[
Filename: PHIL_1181_lores.jpg
Thumbnail status: |thumb|
Pixel size: |300px|
Placement on page: |right|
Legend/credit: Electron micrograph of the Ebola Zaire virus. This was the first photo ever taken of the virus, on 10/13/1976. By Dr. F.A. Murphy, now at U.C. Davis, then at the CDC. Every image requires a link to the source.
Closed double brackets: ]]
Other examples:
Bold
Italic
Subscript: H2O
Superscript: Fe3+
Overview of Smallpox
The Virus
Variola major is the virus that causes smallpox.[4] Symptoms of smallpox include fever and the characteristic skin rash of pox, and it has a 30% mortality rate.[4] The mortality rate of smallpox for pregnant females was very high, up to 70% for those unvaccinated.[4] Ocular variola and resulting blindness was common in smallpox patients in Asia.[4] Smallpox in children caused elbow and knee joint problems in around 2% of unvaccinated children.[4] Those who survived having smallpox were left with many scars on their body.[4]
History
Variola virus emerged thousands of years ago and has subsequently infected many human populations throughout history, causing epidemics of smallpox.[4] The oldest description of smallpox came from China in the 4th century CE. Remnants of smallpox pustules have been found on Egyptian mummies that were 3,000 years old.[4] It is theorized that trade and exploration contributed to the spread of smallpox.[4] Variolation was an early method for control of smallpox, invented by Edward Jenner in 1796 when he took matter from a pustule of a person infected with cowpox and inoculated another person with it.[4] Jenner exposed the inoculated person to variola virus and they did not get sick, confirming Jenner’s theory that exposure to cowpox could prevent a person from getting smallpox.[4] The ideas from his research lead to the first vaccination in the 1800’s.[4]
Eradication
Starting in 1959, the World Health Organization (WHO) initiated a design to eradicate smallpox from the world.[4] The last naturally occurring outbreak of smallpox in the United States happened in 1949, and by 1966 smallpox was still prevalent in outbreaks on the continents of Asia, Africa and South America.[4] After 1966, new developments contributed to the eradication cause, like the use of the bifurcated needle, higher quality freeze-dried vaccine, and campaigns for more vaccination.[4] By 1980, the World Health Assembly declared smallpox eradicated from earth.[4] After eradication, it was determined by health officials that research should still be done on variola virus.[4]
Smallpox as a Bioterrorism Agent
History
According to the CDC, smallpox is labeled as one of the most dangerous potential agents of bioterrorism in the world.[3] It earns this title because of the agent's ease of transmission, the world population's lack of immunity, and the speed of spread from one infected person to another.[5] It is theoretically possible to artificially make a variola major from confirmed and published gene sequences. The technology exists for creation of live poxviruses from existing genetic material fragments. An instance of smallpox bioterrorism occurred in the 1700’s when the British and French invaders gave Native Americans blankets that were contaminated with smallpox, when the Natives were not compliant with the European’s expansion westward. Additionally, during the time of World War Two, America, Japanese, British and Soviet researchers all looked into producing smallpox as a biological weapon.
Population immunity
The world population's lack of immunity to smallpox is due to the fact that anyone born after the 1970’s will not have been vaccinated because most countries stopped providing the vaccine after the virus was eradicated from Earth.[6] Among people who had the vaccine before the 1970’s, it is assumed that their immunity has worn off so they would be susceptible to the virus, because immunity from vaccination is said to only last 3-5 years.[6] However, there is some debate about the true level of susceptibility of the population vaccinated before 1970, because there has been research that suggests they could still have some level of immunity.[6] This point of view has highlighted the need for continued research about smallpox immunity. [6]. Continued research could help inform public health decisions if an incident of smallpox bioterrorism were to occur.[6] Such decisions could be about who receives vaccines first if an outbreak occurs while vaccines are still limited.[6]. If, for example, continued research shows that people who were vaccinated before 1970 still retain their immunity to smallpox, this could indicate that a smallpox bioterrorism attack would not be as devastating as originally thought, because those people would survive, and vaccination resources could be allocated to those born after 1970 and who are unvaccinated. [6]. However, the theory that a smallpox vaccine provides a lifetime of immunity is an unproven theory, and more research should be done to build the best possible reaction if a smallpox bioterrorism attack were to occur.[6]
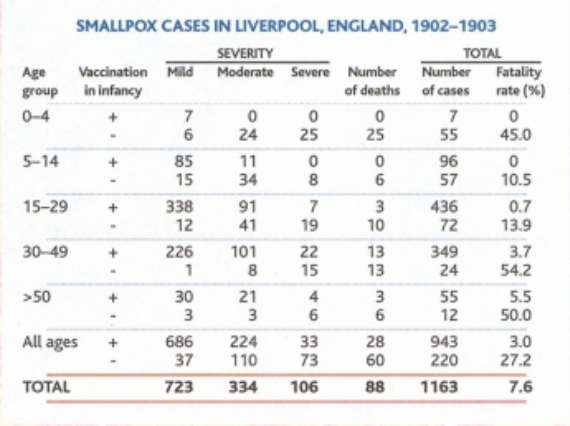
Researchers analyzed a smallpox outbreak in Liverpool, England in 1902 in order to observe whether vaccination at birth was sufficient in protecting people exposed to smallpox later in life. The data is shown in the figure to the right.
Ultimately, researchers did find that vaccination at birth was not completely sufficient in protecting adults who got exposed to smallpox.(See figure) This finding led to the idea that booster shots should be needed every ten years. However, the research also showed that among the unvaccinated population, mortality was higher.(See figure) This data from Liverpool England in the 1900’s goes to show that vaccination against smallpox at birth could actually provide some protection against the disease later in life. More research should be done before this finding is used in actual practice or planning for a bioterrorism attack response, but the nature of this research is difficult since the existing variola major viruses are under extreme protection and their existence has sparked controversy recently.
Research
After smallpox eradication from the natural world, there was debate whether the remaining Variola virus in controlled laboratory environments should be destroyed completely, or should be kept alive for further research on smallpox disease.[7] Since smallpox in the natural world was destroyed before it had the chance to be studied in a modern clinal setting, the World Health Organization (WHO) in 1999 allowed research on Variola major to happen under a WHO committee.[7] The problems the researchers were addressing were a lack of understanding the pathophysiology of the smallpox disease, a lack of an adequate animal model system to study the virus, a need to improve function of laboratory tests, a lack of an antiviral drug to work against Variola major, and lack of knowledge about the overall genetic makeup of the virus.[7] There are currently two known places on Earth where variola virus is stored and researched: the Centers for Disease Control and Prevention in Atlanta Georgia USA, and the State Research Center of Virology and Biotechnology in Koltsovo Russia.[7] Since 1999, many clinical questions about smallpox have in fact been answered and thus there is controversy whether the variola virus stored and researched in these labs should be destroyed, or should be continued to be studied.[7]
Overview of Anthrax

The Bacterium
Bacillus anthracis is the bacterium that causes anthrax disease.[8] The bacterium is gram-positive, rod-shaped, and spore-forming.[8] B. anthracis is naturally found in the soil, and anthrax is spread to animals that graze and ingest the spores.[8] The spores have a protective coating that makes them immune to environmental factors and host defenses.[8] Anthrax can infect the body by getting into cuts, being ingested or being inhaled, and spores being inhaled has been determined to be the most likely form of distribution that would be in a bioterror attack.[8]
History
It is believed that anthrax has ancient origins in Egypt, Mesopotamia and Greece.[9] Ancient depictions lead scholars to think that anthrax might be written about in the Bible as the fifth plague of Egypt, and also in the Iliad by Homer.[9]
Scientist Louis Pasteur created the first anthrax vaccine in 1881. In 1979 the former Soviet Union experienced an accidental release of anthrax aerosols that caused an epidemic. The anthrax aerosol traveled up to 50 km and killed around 60 people and many livestock animals, proving that the released spores can have a significant impact.
In fact, very soon after the terrorist attack in the United States on September 11th 2001, the country experienced another terror attack, in the form of Bacillus anthracis spores being sent in the mail. This event caused 22 cases of anthrax and 5 deaths.
Modern anthrax vaccines have been more successful if they contain a combination of plasmid DNA that encodes for important outer proteins PA and BclA, than those vaccines that only contain plasmids for one of these proteins.[8]
Bioterrorism
Anthrax spores are consistently labeled a leading bioweapon threat due to their ease of dispersal and their stability.[8] There have been independent terrorist groups that threaten to use anthrax spores as a bioterrorism agent.[8] Additionally, biological weapons programs in Iraq and the former Soviet Union have been known to study delivery of pathogenic aerosols by aircraft, including anthrax aerosols.[8] Many systems have been put into place to detect the first cases of anthrax or another illness due to a potential bioterrorism attack.[10] The Department of Health and Human Services (DHHS) provided over 918 million dollars to state and local health departments to assist their preparations for terrorist attacks.[10] In the United States in 2001, at the time of the anthrax bioterrorism attacks, the Laboratory Response Network for Bioterrorism (LRN) tested about one million environmental specimens.[10] Since then, because of the success and importance of these laboratories, more specialty LRN laboratories have been created in the United States, and they now have the capacity to test for microbes that cause anthrax, botulism, tularemia, and plague in the event of a bioterrorist attack.[10]
Responses to the 2001 Anthrax Bioterrorism Attacks
In 2001, 18 cases of anthrax occurred in the United States after people received letters in the mail that contained anthrax spores, a clear example of a bioterrorism attack.[11] Following this event, experts evaluated and revamped bioterrorism response plans with the new information gathered from this tragedy. [11]The following section discusses some of these plans and ideas about how the attack influenced the future of bioterrorism preparedness.
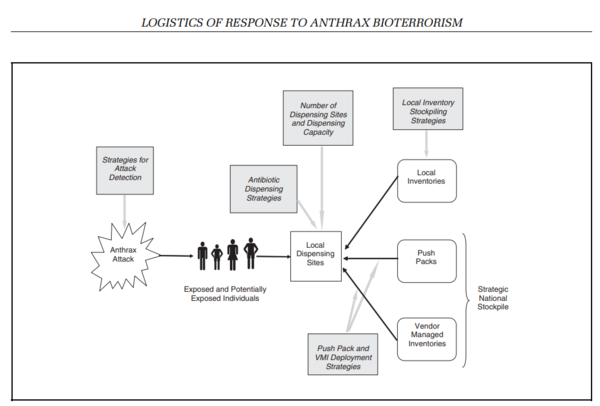
A study done, led by Gregory Zaric at the University of Western Ontario, Canada, aimed to model the preparedness of communities to an anthrax bioterrorism attack.[12] This study summarizes a mathematical model used in Excel to attempt to answer situational questions, and help inform local community leaders what the facts are about preparedness, and offers insight to how funds should be allocated to maximize preparedness.[12] The flow chart at right depicts a standard method of action outlined in this study were an anthrax bioterrorism attack to occur.
Because of the apparent risk anthrax poses as a potential agent of bioterrorism, there have been extensive procedures published, preparing for an attack on the United States, with the goal of creating a logistic mathematical model for the allocation and timely distribution of medical supplies.[12] There are three organizational levels of funds and supplies, and those are the national, regional and local levels.[12] It is imperative that first responders, elected officials and medical personnel from all three levels work in line with the plan in order to work efficiently in the event of a bioterrorism attack.[12] At the federal level, agencies that would be involved with the planning and execution of a response to a bioterrorism attack would be the CDC, the National Institute of Health, the Food and Drug Administration, the Agency for Health Care Research and Quality, and the Office of Emergency Preparedness.[11] Additionally, other federal agencies could have input into a plan, such as the Department of Agriculture, the Department of Commerce, and the Justice Department.[11] All planning and execution for bioterrorism response preparedness requires cooperation and clearly defined responsibilities from the parties involved. At the regional and local levels, all responders should know when, where and how to initiate their responses.[11]
After planning, the next step in a response initiative is detection.[11] Detection of a bioterrorist attack involves surveillance programs of public health, including 911-calls, emergency rooms, hospitals, poison control centers, veterinarians and pharmacies. Detection of a bioterrorism attack is not straightforward, and could be confused with a new emerging disease outbreak.[11] But indicating clues of a bioterrorism attack could be prevalence of a disease at the wrong time of year, unusual modes of transmission, or clusters of diseased individuals in certain areas.[11]
After the detection of a bioterrorist attack, the next step is mass diagnosis.[11] Healthcare professionals should be familiar with rare diseases that might be used in a bioterrorism attack, anthrax being one example.[11] Improving on the ability to screen for pathogens is important for the ability to diagnose those who have been impacted by a bioterrorist event.[11]
Once a local area has realized they are under a bioterrorism attack, there should be clear instructions in place for requesting and obtaining medical supplies.[11] At the national level of organization, in the United States, stockpiles of supplies such as antibiotics and antidotes for many possible bioterrorism agents are held at the national level at the Strategic National Stockpile.[12] These supplies are called “push packs” and can be distributed to any local community at the time of a bioterrorism attack.[12] In addition to these nationally held push packs are “Vendor Managed Inventories” of supplies held at the regional or state level which can be distributed at the local level in the event that the national stockpile needs assistance.[12] Additionally at the local level, communication and media messages should be used at the local level to curb hysteria from the citizen population.
Conclusion
Smallpox disease caused by variola major virus and anthrax disease caused by bacillus anthracis bacteria are both classified by the CDC as high potential agents for bioterrorism. Due to their ease of transmission and spread, and the high mortality rate, an attack using these pathogens would be devastating to populations. Variola virus was eradicated from the natural world, but is currently being kept in two known laboratory locations in the United States and Russia. The World Health Organization deemed it appropriate in 1996 to keep the virus for research purposes. Many of those original research questions have been answered since then, so there is controversy whether the virus should be disposed of, or whether further research should be done. The potential of smallpox bioterrorism is another contributing factor to this debate. For example, there is not sufficient evidence for what length of time the smallpox vaccine provides an individual immunity. If more conclusive research could be done on this topic, it would aid in preparation for a smallpox bioterrorism event because public health planners would be able to determine who gets priority vaccination. Plans for vaccination and treatment at the time of a bioterrorism event are very important to mitigating mortality rates. This topic was discussed extensively in 2001 when the United States experienced an anthrax bioterrorism event. The importance of establishing roles and responsibilities of the national, regional, and local health departments is apparent. Plans for detection, diagnosis, and communication can help save lives.
References
- ↑ Klietmann, W., & Ruoff, K. (2001). Bioterrorism: Implications for the Clinical Microbiologist. Clinical Microbiology Reviews, 14(2).
- ↑ 2.0 2.1 2.2 2.3 2.4 Poupard J. A. and Miller L. A. History of biological warfare: catapults to capsomeres. Ann. N.Y. Acad. Sci. 666 1992 9 -20
- ↑ 3.0 3.1 Bioterrorism agents/ diseases. (2018, April 4). Centers for Disease Control and Prevention. Retrieved April 14, 2023, from https://emergency.cdc.gov/agent/agentlist-category.asp#catdef
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 4.15 4.16 History of smallpox. (2017, July 12). Centers for Disease Control and Prevention. Retrieved April 15, 2023, from https://www.cdc.gov/smallpox/history/history.html
- ↑ [https://www.sciencedirect.com/science/article/abs/pii/S016635420200195X?casa_token=BAEEGzZOu1QAAAAA:jxDQksNJlx34KwNixNQR0UV6v2aAMlqQRAzTNSdddhULo97VugZPdM6YqsVLmW8w00j6Fq-DwQ Whitley, R. (2003). Smallpox: a potential agent of bioterrorism. Science Direct, 57(1-2). ]
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 6.7 Cohen, J. (2001). Smallpox Vaccinations: How Much Protection Remains? American Association for the Advancement of Science, 294(5544).
- ↑ 7.0 7.1 7.2 7.3 7.4 Lane, J. M. (2011). Remaining Questions about Clinical Variola Major. Emerging Infectious Diseases, 17(4).
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 8.7 8.8 Bouzianas, D. (2009). Medical countermeasures to protect humans from anthrax bioterrorism. Science Direct, 17(12).
- ↑ 9.0 9.1 [https://www.cdc.gov/anthrax/basics/anthrax-history.html History of Anthrax. (2020, November 20). Centers for Disease Control and Prevention. Retrieved April 15, 2023, from https://www.cdc.gov/anthrax/basics/anthrax-history.html]
- ↑ 10.0 10.1 10.2 10.3 [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2730306/ Hughes, J., & Gerberding, J. (2002). Anthrax Bioterrorism: Lessons Learned and Future Directions. Emerging Infectious Diseases, 8(10).]
- ↑ 11.00 11.01 11.02 11.03 11.04 11.05 11.06 11.07 11.08 11.09 11.10 11.11 Brachman, P. (2002). Bioterrorism: An Update with a Focus on Anthrax. American Journal of Epidemiology, 155(11).
- ↑ 12.0 12.1 12.2 12.3 12.4 12.5 12.6 12.7 Zaric, G., Bravata, D., Cleophas Holty, J.-E., McDonald, K., Owens, D., & Brandeau, M. (2008). Modeling the Logistics of Response to Anthrax Bioterrorism. Medical Decision Making.
Authored for BIOL 238 Microbiology, taught by Joan Slonczewski, 2023, Kenyon College
