Methicillin Resistant Staphylococcus Aureus (MRSA): Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
{{Curated}} | {{Curated}} | ||
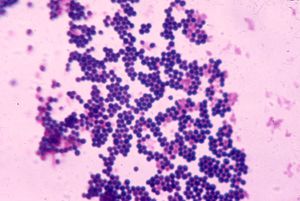
[[Image:MRSAmicroscopic.jpeg|thumb|300px|left|''Gram-stained Staphylococcus aureus. From: Microbeworld.org [http://www.microbeworld.org/component/jlibrary/?view=article&id=7611]]] | |||
==Etiology/Bacteriology== | ==Etiology/Bacteriology== | ||
===Taxonomy=== | ===Taxonomy=== | ||
| Line 17: | Line 17: | ||
===Description=== | ===Description=== | ||
<i>[[Staphylococcus aureus]]</i> is a Gram-positive, non-spore forming, nonmotile, cocci bacterium that colonizes in yellow clusters. This facultative anaerobe is considered natural flora in 20-30% of humans, living in the anterior nares and on the skin and was first isolated in the 1890’s from the pus from a surgical abscess in a knee joint. <i>S. aureus</i> is the most common type of staphylococci to cause infections because of its ability to evade the immune system and many antibiotics. These “Staph infections” can cause bacteremia, endocarditis, soft tissue infections, pneumonia, bone and joint infections, CNS, toxic shock syndrome, and even food poisoning. The most notorious strain of <i>Staphylococcus aureus</i> was identified in the 1960's and is known as the methicillin resistant strain, commonly known for causing mild to severe skin infections resulting in death if not treated promptly. The most common place to contract Methicillin Resistant Staphylococcus aureus (MRSA) infection is typically in a hospital, but community outbreaks during the past decade have been widely observed, leading scientists to distinguish between [[Hospital-acquired Methicillin Resistant Staphylococcus Aureus (MRSA)]] and [[Community-Acquired Methicillin-Resistant Staphylococcus Aureus (CA-MRSA)]]. | <i>[[Staphylococcus aureus]]</i> is a Gram-positive, non-spore forming, nonmotile, cocci bacterium that colonizes in yellow clusters. This facultative anaerobe is considered natural flora in 20-30% of humans, living in the anterior nares and on the skin and was first isolated in the 1890’s from the pus from a surgical abscess in a knee joint. <i>S. aureus</i> is the most common type of staphylococci to cause infections because of its ability to evade the immune system and many antibiotics. These “Staph infections” can cause bacteremia, endocarditis, soft tissue infections, pneumonia, bone and joint infections, CNS, toxic shock syndrome, and even food poisoning. The most notorious strain of <i>Staphylococcus aureus</i> was identified in the 1960's and is known as the methicillin resistant strain, commonly known for causing mild to severe skin infections resulting in death if not treated promptly. The most common place to contract Methicillin Resistant Staphylococcus aureus (MRSA) infection is typically in a hospital, but community outbreaks during the past decade have been widely observed, leading scientists to distinguish between [[Hospital-acquired Methicillin Resistant Staphylococcus Aureus (MRSA)]] and [[Community-Acquired Methicillin-Resistant Staphylococcus Aureus (CA-MRSA)]]. | ||
Revision as of 12:07, 23 July 2013
Etiology/Bacteriology
Taxonomy
| Domain = Bacteria | Phylum = Firmicutes | Class = Bacilli | Order = Bacillales | Family = Staphylococcaceae | Genus = Staphylococcus | species = S. aureus
|
NCBI: Taxonomy Genome: Staphylococcus aureus |
Description
Staphylococcus aureus is a Gram-positive, non-spore forming, nonmotile, cocci bacterium that colonizes in yellow clusters. This facultative anaerobe is considered natural flora in 20-30% of humans, living in the anterior nares and on the skin and was first isolated in the 1890’s from the pus from a surgical abscess in a knee joint. S. aureus is the most common type of staphylococci to cause infections because of its ability to evade the immune system and many antibiotics. These “Staph infections” can cause bacteremia, endocarditis, soft tissue infections, pneumonia, bone and joint infections, CNS, toxic shock syndrome, and even food poisoning. The most notorious strain of Staphylococcus aureus was identified in the 1960's and is known as the methicillin resistant strain, commonly known for causing mild to severe skin infections resulting in death if not treated promptly. The most common place to contract Methicillin Resistant Staphylococcus aureus (MRSA) infection is typically in a hospital, but community outbreaks during the past decade have been widely observed, leading scientists to distinguish between Hospital-acquired Methicillin Resistant Staphylococcus Aureus (MRSA) and Community-Acquired Methicillin-Resistant Staphylococcus Aureus (CA-MRSA).
Pathogenesis
Transmission
Since S. aureus are a part of the natural flora in many humans’ nose and mouths, especially humans working in hospitals, the transmission of these bacteria can be difficult to prevent. Because the bacterium is nonmotile, S. aureus is most commonly spread through human-to-human contact or through contaminated surfaces./foods MRSA is typically spread from human-to-human by the hands. In a few cases MRSA can be transmitted through the cough of someone infected with MRSA pneumonia.
Infectious dose, incubation, and colonization
Epidemiology
Virulence factors
Clinical features
Symptoms
Morbidity and Mortality
Diagnosis
Treatment
Prevention
Immune Response
Host Response
Bacterial Evasion
References
Created by Dehra McGuire, student of Tyrrell Conway at the University of Oklahoma.
