Ebola virus entry into host cells
Introduction
By Issam Hamdallah
Ebola viruses belong to the family, Filoviridae. Ebolavirus is one of two filovire geneses, Marburgvirus and Cuevavirus. There are five known species of ebolavirus; Bundibugyo ebolavirus (BDBV), Zaire ebolavirus (EBOV), Reston ebolavirus (RESTV), Sudan ebolavirus (SUDV), and Taï Forest ebolavirus (TAFV). The virus got its name from the Ebola river, the river that runs near the first discovery site in sub-Saharan Africa. Species such as Zaire ebolavirus (EBOV) cause hemorrhagic fever and have up to a 90% mortality rate in humans (Leroy et al. 2001). Due to the very high mortality rate, this virus is of great concern to scientists today and is considered to be a risk group 4 pathogen. Even species such as Reston ebolavirus, which causes illness in infected, non-human primates but not in humans, are still of great concern because there is a chance that the virus could mutate and become pathogenic to humans (Weingartl et al. 2012). Moreover, since there is no effective vaccine, treatment, or cure for the virus, the virus could potentially be used as a bioterrorism agent. For these reasons, access to the virus is strictly regulated.
The natural reservoir of the virus is still unknown. The virus is believed to have originated in fruit bats, but that has not been confirmed. Outbreaks of ebolavirus tend to occur in places where the consumption of “bushmeat” is commonplace, such as Sub-Saharan Africa. This is strong evidence that the virus infects the human population first through animal-human contact, then through human-human contact.
Transmission
Ebolavirus is transmitted through the blood, the exchange of bodily fluids, contact with infected humans, and infected animals such as primates, fruit bats and pigs. Consumption of “bushmeat” such as primates, or bats is just one way that ebolavirus infects the human population. Unprotected sex, the sharing of needles, and burial practices that involve excessive physical contact with infected corpses are other means by which the virus is transmitted. There is also evidence that EBOV is transmitted from pigs to non-human primates via aerosols (Weingartl et al. 2012). This means that EBOV could be transmitted from infected animals to humans similarly, which demonstrates how dynamic ebolavirus can be.
Symptoms
Initially symptoms of ebolavirus include headache, muscle aches, fever, and fatigue. These symptoms are very similar to other common diseases in Sub-Saharan Africa such as Malaria. One theory of how EBOV initially spread is that a person infected with EBOV showing symptoms similar to Malaria, received a Malaria vaccine at a local missionary (Preston, 1994). The same needle used to give him that vaccine, was used to give others the same vaccine and a lethal amount of EBOV. Soon after initially falling ill, symptoms more specific to EBOV begin to surface as the virus begins replicating inside of the host.
Symptoms of ebolavirus infection include vomiting, damage to the lungs, spleen, liver, and blood vessels all of which result in excessive internal and external bleeding. Those infected with EBOV usually die within days of infection. Since the virus cannot survive without a host, EBOV increases its chances of colonizing another host by causing hemorrhagic fever, where those infected go into shock and “bleed out”. Strains of ebolavirus that have not been found to be pathogenic in infected humans include Taï Forest ebolavirus (TAFV), which was first discovered in China, and Reston ebolavirus (RESTV), which was isolated from monkeys in the Philippines. These two strains of ebolavirus are very lethal to nonhuman primates, but not to humans. Strains of ebolavirus originating in Sub-Saharan Africa such as Bundibugyo ebolavirus (BDBV), Zaire ebolavirus (EBOV), and Sudan ebolavirus (SUDV) are much more deadly in humans.
Structure
Ebolavirus possesses a single-stranded, non-segmented, negative RNA strand genome that contains seven genes: NP, VP35, VP40, GP, VP30, VP24 and L. Ebolavirus contains its genetic information in a nucleocapsid. Once Ebolavirus has successfully entered a host cell, it hijacks the transcription and translation of the host. Ebolavirus can infect an array of host cells which makes the virus a very successful infectious agent. The diameter of Ebolavirus is a consistent 80 nm, but the length ranges from 600 to 1400 nm (Aleksandrowicz et al. 2011).
Entry into host cell
EBOV uses macropinocytosis, or clathrin-mediated endocytosis in order to gain access into target host cells. Macropinocytosis is normally used to incorporate larger virus particles into the host cell, whereas clathrin-mediated endocytosis is used to incorporate smaller virus particles into the host cell. Macropinocytosis is a process in which the Eukaryotic host cells form macropinosomes, segments of plasma membranes that extend out from the cell approximately 0.2-10 µm, in order to incorporate the virus into the cell. The formation of macropinosomes occur spontaneously, as a result of the activation of various growth factors, or simultaneously with the intake of cellular molecules or extracellular fluid.
Ebolavirus like particles (EBOV-VLPs), the viruses used by Aleksandrowicz et al. 2011 in their study of ebolavirus entry into host cells, reach a length as long as 2 µm, but stimulate the formation of vesicles approximately 0.5 - 3.5 µm in diameter. EBOV-VLPs enter the protruding segment of the membrane after which the membrane encloses around the EBOV-VLP forming a vesicle and incorporates the virus into the cell. Evidence for this type of activity is demonstrated by the unusually high amount of actin ruffles located on the parts of the eukaryotic plasma membrane with a high concentration of EBOV-VLPs in close proximity. Cells treated with EBOV-VLPs spawned an increase in the number of vesicles formed by eukaryotic cells. Cells that were not treated with EBOV-VLPs did not see any change in the formation of vesicle formation. The formation of the vesicles via macropinocytosis occurs as a result of actin-mediated ruffle formation which is activated by the presence of EBOV-VLPs.
Further evidence that EBOV-VLPs use macropinocytosis to gain access to target host cells is seen when drugs are used to inhibit signals and mechanisms required for the host cell to incorporate the EBOV-VLPs via macropinocytosis. Latruncluin A, a toxin that inhibits the binding of actin polymerization, 5(N-Ethyl-N-isopropyl)-amilorid, which inhibits an Na+/H+ antiporter, and wortmannin, a toxin that inhibits PI14-kinase, were the drugs used to inhibit macropinocytosis. In each of the drug treatments, the relative infection rates experienced a significant decline which means that the EBOV-VLPs were not successfully incorporated into the cells. This is evidence that macropinocytosis is an essential means by which EBOV-VLPs cause infections in host eukaryotic cells.
Another means by which EBOV-VLPs gain access to host cells is clathrin-mediated endocytosis. Clathrin is a protein that is important for vesicle formation. Eukaryotic cells with depressed levels of clathrin demonstrated a reduction of EBOV-iVLP infection up to about 25% (Figure 5). This is evidence that clathrin- mediated endocytosis is an essential part of the uptake of EBOV-VLPs into eukaryotic host cells.
Numerous factors specific to Ebolavirus (EBOV) are necessary in order for Ebola virus to gain access into a host cell. One of the components that have been found to be required in order for EBOV to enter a host cell are EBOV envelope glycoproteins (GP). EBOV GP aids in the binding of EBOV to the host cell by binding to surface receptors on the host cell (Lee and Saphire, 2009). EBOV GP is the only protein expressed by EBOV on the surface membrane of the virus. In a paper published in 2009, Lee and Saphire proposed five cellular factors, DC-SIGN/L-SIGN, LSECtin, hMGL, β-integrins, and Tyro3 family receptors that may be required for attachment to the host cell surface, but none of the cellular factors turned out to be required for viral entry.
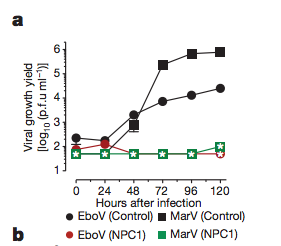
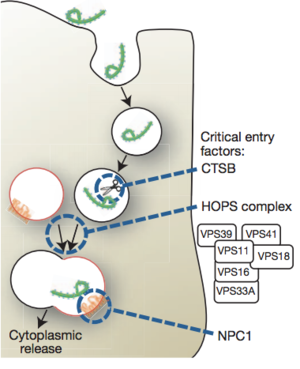
The data published by Lee and Saphire in 2009 laid the foundation for Carette et al. (2011) to find that Niemann-Pick C1 (NPC1), a cholesterol transporter, is required for Ebola entry into the host cell. Lee and Saphire, 2009, found that the entry of ebolavirus is facilitated by viral glycoproteins (GP). Glycoproteins served to attached Filoviruses to the host’s surface, send the viruses to endosomes, and aid in the fusion between the virus and membranes of the endosomes. Carette et al. 2011 created mutations in the homotypic fusion and vacuole protein-sorting (HOPS) complex, which aids in the fusion of endosomes to lysosomes, and they also created mutations in the edosomal and lysomal cholesterol transporter protein NPC1 in order to determine both of their involvement in Ebola virus entry. It was determined that the NPC1 cholesterol transporter, which is found in the lysosomal membrane, is required for ebolavirus infection of host cell (Figure. 2). NPC1 plays an important role in the entry of the virus and the release of the virus from the vacuole into the cytoplasm of the host (Figure. 3). The HOPS complex was found to be an important component in the process of viral infection, but is not essential.
Vaccines
To date, there is no form of treatment, cure, or vaccine for ebolavirus infection. Carette et al. 2011 proposed a means for the development of potential antifilovirus pharmaceuticals by inhibiting the NPC1 cholesterol transporter. This has been demonstrated to inhibit EBOV infection in mice, but would block the cholesterol transport pathway; therefore, this form of treatment has not yet been found to be a cure.
More recently, an article written by Ferris Jabr in the April 2014 edition of Scientific American reported that small interfering RNA (siRNA) have been by used researchers at the University of Texas Medical Branch at Galveston to cure monkeys infected with ebola. The siRNA used target a protein in Ebola that inhibits viral replication. The siRNA used only targets the viral proteins; therefore, it does not affect any host cellular components. It is the most promising research to date.
Conclusion
Ebolavirus is a rare, yet deadly virus. Although it has not become a global pandemic,it is a very dangerous virus because of its high mortality rate in both humans and non-human primates, lack of an effective vaccine, and ability to mutate. Macropinocytosis and clathrin-mediated endocytosis are the main mechanisms utilized to gain access into target host cells. The method of entry depends primarily on the size of the particle. Macropinocytosis is the primary method for the entry of large viruses, and clathrin-mediated endocytosis uptakes smaller virus particles. Glycoproteins and NPC1 are also required for ebolavirus to enter and infect the host cell. Ebolavirus entry into the host is the first step towards infection; therefore, understanding the processes is crucial in finding a cure for ebolavirus infection.
References
J.E. Carette, M. Raaben, A.C. Wong, A.S. Herbert, G. Obernosterer, N. Mulherkar, A.I. Kuehne, P.J. Kranzusch, A.M. Griffin, G. Ruthel, P. D. Cin, J.M. Dye, S.P. Whelan, K. Chandran, T.R. Brummelkamp. 2011 .Ebola virus entry requires the cholesterol transporter Niemann-Pick C1. Nature. Vol. 477: 340-346
P. Aleksandrowicz, A. Marzi, N. Biedenkopf, S. Becker, T. Hoenen, H. Feldmann, H.J. Schnittler. 2011. Ebola Virus Enters Host Cells by Macropinocytosis and Clathrin-Mediated Endocytosis. Journal of Infectious Diseases. Vol. 204: 957-967
H.M. Weingartl, C. Embury-Hyatt, C. Nfon, A. Leung, G. Smith, G. Kobinger. 2012. Transmission of Ebola virus from pigs to non-human primates. Nature. Vol. 811: 1-4
W. Phoolcharoen J.M. Dye, J. Kilbourne, K. Piensook, W.D. Pratt, C.J. Arntzen, Q. Chen, H.S. Mason, M.M. Herbest-Kravlovetz. 2011. Proceeding of the National Academy of Sciences. A nonreplicating subunit vaccine protects mice against lethal Ebola virus challenge. Vol. 108(51): 20695–20700
Baylor College of Medicine. July, 02, 2013. Ebola Virus. https://www.bcm.edu/departments/molecular-virology-and-microbiology/ebola (4-12-14)
Albert Einstein College of Medicine of Yeshiva University. 2014. Researchers Find "Key" Used by Ebola Virus to Unlock Cells and Spread Deadly Infection. https://www.einstein.yu.edu/news/releases/695/researchers-find-key-used-by-ebola-virus-to-unlock-cells-and-spread-deadly-infection/ (4-12-14)
Tiffany Kaiser. August 15, 2011. Research Team Discovers How Ebola Virus Enters, Replicates in a Host Cell. http://www.dailytech.com/Research+Team+Discovers+How+Ebola+Virus+Enters+Replicates+in+a+Host+Cell/article22542.htm (4-12-14)
Preston, Richard. 1994. The Hot Zone. New York: Random House, 300.
Ferris Jabr. 2014. Scientific American. Defeating Nature’s Terrorist- An RNA-based treatment may stop the Ebola virus in its tracks. Scientific American. Vol. 310: 58
J.E. Lee, E.O. Saphire. 2009. Future Virology. Ebolavirus glycoprotein structure and mechanism of entry. Vol. 4: 621-635
Ed, Ward M.D. 3-25014. Update 3-25-14 of 11-16-13 Alert! Mutated Ebola Virus Epidemic In US?. http://edwardmd.wordpress.com/2013/11/16/breaking-alert-mutated-ebola-virus-epidemic-in-u-s/ (4-12-14)
World Health Organization. April 2014. Ebola virus disease. http://www.who.int/mediacentre/factsheets/fs103/en/