Cognitive and Physical Effects of Bacterial Meningitis
Introduction
By Alyssa Gest
Meningitis, characterized by the inflammation of the meninges surrounding the brain and spinal cord, poses a significant threat to human health, especially acute bacterial meningitis [1]. Understanding the etiology and virulence factors of bacterial meningitis is crucial for prevention, diagnosis, and treatment. Such pathogens include Streptococcus pneumonia, Neisseria meningitidis, Haemophilus influenza, and Listeria monocytogenes [2] They demonstrate various mechanisms to break through the blood-brain barrier and invade the central nervous system[3] . These lead to altercations in the brain and spinal cord and later the infected person can develop cognitive impairment and physical consequences. These mechanisms enable bacterial colonization inside the hose cell and promote their survival. They also involve complex interactions with the virulence factors of the pathogenesis bacteria and the host cell immune mechanisms.[3] These processes help scientists and doctors develop targeted therapies and vaccines for bacterial meningitis.
Background
Historical Perspective
Evidence of central nervous system (CNS) infections are one of the oldest infections known in mankind[4]. In the 17th and 18th centuries, brain fever was frequently referred to as “phrenitis” and “cephalitis” which today, is classified as meningitis. These patients reported symptoms like headaches, fever, and delirium [4].The clinical characterization of meningococcal disease outbreak was first found in Genvea in 1805, by a general practitioner, Gaspard Vieusseux[5]. The initial occurrence in Africa was documented in 1840 but it wasn't identified as meningococcal bacteria as the causative agent of meningitis by Austrian bacteriologist Anton Vaykselbaum [6].
Pathophysiology of Bacterial Meninigitis
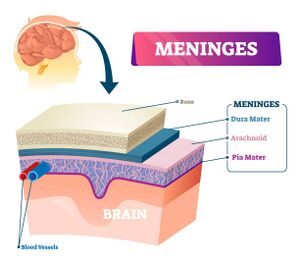
The meninges, consisting of three protective layers surrounding the brain and spinal cord, play a vital role in guarding these organs while providing nourishment and support[7]. The meninges contain three layers, the outer layer is called the dura mater, the middle layer is the arachnoid mater, and the inner layer is called the pia mater (the arachnoid mater and pia mater are the leptomeninges)[7]. Between the leptomeninges is a space called the subarachnoid space which holds cerebrospinal fluid (CSF)[7]. It is a clear water fluid that is pumped around the brain and spinal cord, to protect them from impact/contact and contains nutrients[7]. The CSF is held under some pressure, below 200mm of water which is less than ⅕ of the mean arterial pressure[7]. There is about 150mL of CSF in the body which is constantly refilled with 500mL of new fluid every day and the excess is absorbed into the bloodstream (350mL)[7]. For nutrients to enter and exit the CSF/brain, they have to go through the stringently controlled blood-brain barrier[7]. The endothelial cells in the blood vessels are so tightly packed next to each other that they prevent leakage and only allow specific molecules to pass through[7]. This is the same concept as the phospholipid bilayer in eukaryotic cells. Inflammation occurs in the leptomeninges, not the brain itself (which is called encephalitis). However, these can occur at the same time which is referred to as meningoencephalitis [7].
What triggers inflammation?

It can be caused by an autoimmune disease, where the body attacks itself or the body could experience having an unfavorable reaction to a certain medication. This can occur during intrathecal therapy (medication is injected directly into the CSF). The most common way of contracting the disease is by infection across all ages (ex. Neisseria meningitidis bacteria or herpes simplex virus). There are two routes the infection can take to reach the leptomeninges and the CSF. The first route is direct spread, which is when the pathogen gets inside the spinal column or skin and then penetrates the meninges, leading into the CSF. The pathogen will either come through the skin or up the nose. The second route is through hematogenous spread, which is when the pathogen enters the bloodstream and moves through the endothelial cells in the blood vessels making up the blood-brain barrier and entering the CSF. Bacteria will do this by binding to surface receptors on the endothelial cells to get across the barrier. If not, they will find other areas to damage like the choroid plexus. Once it enters the CSF, it can start replicating and spreading. The white cells will eventually detect the pathogenic cells and send cytokines to bring in more immune cells. “Over time, a microliter of CSF might go on to contain up to thousands of white blood cells, but any more than five usually defines meningitis. In most bacterial cases, there’ll be above 100 white blood cells per microliter and more than 90% PMNs. In most viral cases, there’ll be 10 to 1000 white blood cells; over 50% lymphocytes, and under 20% PMNs. In most fungal cases, there’ll be 10-500 white blood cells, with over 50% lymphocytes. In most cases of tuberculous meningitis, there’ll be 50-500 white blood cells with over 80% being lymphocytes”. The pressure from the additional immune cells will most likely rise above 200 nm of water. The immune system will also induce the glucose concentration to drop in the CSF, up to below 2 ⁄ 3 of the concentration in the blood, making the protein levels increase to over 50 mg/dL[7]
Causes and Risk Factors
Age
Everyone is susceptible to catching bacteria meningitis. However, there are multiple pathogens that infect certain age groups more than others. Infants are most likely infected by Group B streptococcus (ex. Streptococcus agalactiae), gram-negative enteric organisms (ex. E.coli), and Listeria monocytogenes (L. monocytogenes)[8]. 1 to 23 month olds are susepctiable to Streptococcus pneumonia (S. pneumonia), Neisseria meningitidis (N. meningitides), S. agalactiae, Haemophilus influenzae (H. influenza), and E.coli[8]. Children and teens are most likely infected with N. meningitidis and S. pneumoniae [7]. Those who are adults and elderly will most likely contract S. pneumoniae, and L. monocytogenes [7]. If you are over 50 years of age, N. meningitidis is also likely as well [8].The immunocompromised status of the infected patient is also an important factor to consider for the rate of survival[8].
Bacterial Families
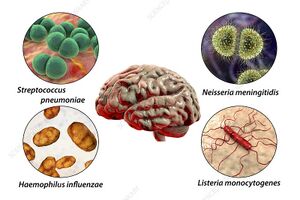
As previously mentioned, multiple bacteria can cause bacterial meningitis. Some examples are Group B Streptococcus, E.coli, H. Influenza, M. tuberculosis, S. pneumonia, and N. meningitidis [9]. Group B Streptococcus measures between 0.5-1.25 micrometers [10], E.coli measures between 1.0-2.0 micrometers long [11], H.influenzae measures between 0.3-1 mircrometers [12], S. pneumonaie measures between 0.5-1.25 micrometers long[13]. Bacterial meningitis can spread through various ways, depending on the bacteria causing the infection. Some individuals will not experience symptoms, but will still be "carriers" of that bacteria that can still be spread to those around them[14]. For instance, Group B Streptococcus and E.coli are usually passed from the mothers to newborns during childbirth[14]. H. influenza, M. tuberculosis, and S. pneumonia are typically transmitted through respiratory droplets through coughing and sneezing during close contact interactions[14]. N. meningitidis, however, spreads through the sharing of respiratory or throat secretions such as saliva or split, which occurs through living in the same proximity, kissing, and coughing[14]. E.coli can be transmitted through food consumption or by the preparation of the food[14]
Symptoms and Diagnosis
Symptoms
Meningitis displays a variety of symptoms and is usually characterized by a sudden onset of a fever, stiff neck, and headache [9]. Individuals may also experience sensitivity to light (photophobia), nausea, vomiting, and altered mental status (ex. confusion)[9]. Individuals may also experience phonophobia which is displaying discomfort due to loud noises [7]. However, newborns and babies may not have these more common symptoms but rather show different signs. These include feeding poorly, irritability, slow/inactive movements, vomiting, abnormal reflexes, or a bulging fontanelle will form on the baby's skull ("soft spot")[9].
Treatment
Include some current research, with at least one figure showing data.
Cognitive and Physical Conseqences
Conclusion
References
- ↑ Zainel, Abdulwahed, Hana Mitchell, and Manish Sadarangani. 2021. "Bacterial Meningitis in Children: Neurological Complications, Associated Risk Factors, and Prevention" Microorganisms 9, no. 3: 535. https://doi.org/10.3390/microorganisms9030535
- ↑ Mehlhorn, Allana, and Brandon Sucher. Chrome-Extension://EFAIDNBMNNNIBPCAJPCGLCLEFINDMKAJ/https://www.nejm.org/doi/pdf/10.1056/nejmoa1905795?articletools=true, April 1, 2007. https://hdl.handle.net/10520/AJA16836707_629.
- ↑ 3.0 3.1 Herold, Rosanna, Horst Schroten, and Christian Schwerk. 2019. "Virulence Factors of Meningitis-Causing Bacteria: Enabling Brain Entry across the Blood–Brain Barrier" International Journal of Molecular Sciences 20, no. 21: 5393. https://doi.org/10.3390/ijms20215393
- ↑ 4.0 4.1 Author links open overlay panelKenneth L. Tyler, AbstractThomas Willis (1621–1675) described patients with, R.R. Carpenter, H.D. Chalke, H.V. Smith, J.H. Steele, J. Abercrombie, et al. “Chapter 28 a History of Bacterial Meningitis.” Handbook of Clinical Neurology, November 3, 2009. https://www.sciencedirect.com/science/article/abs/pii/S0072975208021283 Cite error: Invalid
<ref>tag; name "ac" defined multiple times with different content - ↑ “The History of Meningitis.” Meningitis Research Foundation. Accessed April 13, 2024. https://www.meningitis.org/blogs/the-history-of-meningitis#:~:text=Diagnosis%20%26%20Treatment&text=The%20first%20outbreak%20in%20Africa,as%20a%20cause%20of%20meningitis.
- ↑ “The History of Meningitis.” Meningitis Research Foundation. Accessed April 13, 2024. https://www.meningitis.org/blogs/the-history-of-meningitis#:~:text=Diagnosis%20%26%20Treatment&text=The%20first%20outbreak%20in%20Africa,as%20a%20cause%20of%20meningitis.
- ↑ 7.00 7.01 7.02 7.03 7.04 7.05 7.06 7.07 7.08 7.09 7.10 7.11 7.12 YouTube. (2017, November 8). Meningitis - causes, symptoms, diagnosis, treatment, pathology. YouTube. https://www.youtube.com/watch?v=gIHUJs2eTHA Cite error: Invalid
<ref>tag; name "nn" defined multiple times with different content Cite error: Invalid<ref>tag; name "nn" defined multiple times with different content - ↑ 8.0 8.1 8.2 8.3 Mehlhorn, Allana, and Brandon Sucher. Chrome-Extension://EFAIDNBMNNNIBPCAJPCGLCLEFINDMKAJ/https://www.nejm.org/doi/pdf/10.1056/nejmoa1905795?articletools=true, April 1, 2007. https://hdl.handle.net/10520/AJA16836707_629.
- ↑ 9.0 9.1 9.2 9.3 “Bacterial Meningitis.” Centers for Disease Control and Prevention, July 15, 2021. https://www.cdc.gov/meningitis/bacterial.html.
- ↑ Patterson, Maria Jevitz. “Streptococcus.” Medical Microbiology. 4th edition., January 1, 1996. https://www.ncbi.nlm.nih.gov/books/NBK7611/.
- ↑ National Research Council (US) Steering Group for the Workshop on Size Limits of Very Small Microorganisms. “Correlates of Smallest Sizes for Microorganisms.” Size Limits of Very Small Microorganisms: Proceedings of a Workshop., January 1, 1999. https://www.ncbi.nlm.nih.gov/books/NBK224751/#:~:text=Escherichia%20coli%20is%20a%20typical,with%20radius%20about%200.5%20micrometers.
- ↑ Khattak, Zoia E. “Haemophilus Influenzae Infection.” StatPearls [Internet]., April 27, 2023. https://www.ncbi.nlm.nih.gov/books/NBK562176/#:~:text=Haemophilus%20influenzae%20is%20characterized%20as,coccobacillus%20of%20the%20family%20Pasteurellaceae.
- ↑ Patterson, Maria Jevitz. “Streptococcus.” Medical Microbiology. 4th edition., January 1, 1996. https://www.ncbi.nlm.nih.gov/books/NBK7611/#:~:text=They%20divide%20in%20one%20plane,distinguish%20morphologically%20from%20other%20streptococci.
- ↑ 14.0 14.1 14.2 14.3 14.4 “Bacterial Meningitis.” Centers for Disease Control and Prevention, July 15, 2021. https://www.cdc.gov/meningitis/bacterial.html.
Authored for BIOL 238 Microbiology, taught by Joan Slonczewski,at Kenyon College,2024
