Staphylococcus epidermidis
A Microbial Biorealm page on the genus Staphylococcus epidermidis
Classification
Higher order taxa
Bacteria; Firmicutes; Bacillales; Staphylococcus (1)
Species
Genus Species: Staphylococcus epidermidis
Other Names: Micrococcus epidermidis, Albococcus epidermidis, Staphylococcus epidermidis albus (2)
|
NCBI: Taxonomy |
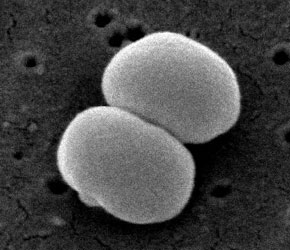
Description and significance
Staphylococcus epidermidis is a gram-positive and coagulase-negative staphylococci (4). It typically lives on the human skin and mucosa and the most common infections on catheters and implants (5). S. epidermidis is one of five most common organisms that cause noscomial infections due to the increase in usage of biomaterials in the clinical environment (8). The nosocomial pathogen causes infections on prosthetic valves, cerebrospinal fluid shunts, joint prosthesis vascular prostheses, valves, and in postoperative wounds and the urinary tract. It is also the most frequent organism found in the blood of bone marrow transplant patients and on central venous catheters for patients of total parenteral nutrition (4).
S. epidermidis strain from healthy adult nares show that there are many kinds of the organism in each individual (9). A common S. epidermidis strain RP62a (ATCC 35984) was isolated in Memphis, Tennessee during 1979-1980 in a wide spread of intravascular catheter sepsis. RP62a is a strain that produces slime, grows collectively and forms biofilm. The treatment of S. epidermidis infections caused by biofilm with antibiotics is often ineffective and results in the necessity to remove the implants (5). Another strain is S. epidermidis ATCC 12228 which does not produce biofilm (7).
The ability to produce slime allows the pathogen to stay on biomaterials. Different strains of S. epidermidis can be distinguished by whether or not they produce slime. In clinical laboratories, S. epidermidis infections are studied by the use of antibiograms, biotyping, plasmid profiles, and slime production; whereas in research, phagetyping, serotyping, restrict enzyme analysis and DNA-DNA hybridization are used (4).
Staphylococcus epidermidis is often compared to Staphylococcus aureus. These bacteria are the two main pathogens in the genus due to the one million serious infections caused in hospitals per year. S. epidermidis is the dominant species that lives mostly on the skin while S. aureus lives mostly on mucosal surfaces. Since these species are resistance to many antibiotics and antimicrobials, the only remaining treatment for most of these staphylococci is glycopeptide antibiotic vancomycin; however, a vancomycin resistant strain of S.aureus was recently found(7).
A controversial issue on S. epidermidis argues whether or not all strains can equally cause disease and if a specific genotype determines a specific disease (6).
Genome structure
Random shotgun method was used to completely sequence the ~2.6-Mb genome S. epidermidis RP62a at The Institute for Genomic Research (TIGR) (7). RP62A’s chromosome length is 2,616,530bp, contains 32.10% of G+C content, 6 rRNA operons and plasmid with 28,080bp and 32% G+C content (11). Two plasmids vSe1 and vSe2 were identified in the strains RP62a and ATCC 12228 and have phrophage integrase genes. The plasmid vSe1 have genes for cadmium resistance whereas a second strain-specific sortase and two LPXTG surface attachment proteins is encoded by vSe2 of ATCC 12228 (7).
S. epidermidis RP62A genome was compared to ATCC 12228 genome to analyze and discover the evolution of the virulence and resistance of them. The nonsyntenic parts of the genome islands are where the differences of resistance and pathogenicity are located. Staphylococci and low-GC-content gram-positive bacteria assisted in changing their virulence and resistance. The cap operon which is the top virulence factor in Bacillus anthracis is also found in S. epidermidis (7).
When the whole genome of S. aureus and S. epidermidis is analyzed it showed that they are overall syntenic, but with differences in genome islands, integrated prophage, IS elements, composite transposons, and integrated plasmids (disease and virulence). TIGR found a new genomic island vSaγ which is contained in all S. aureus and S. epidermidis genomes (7).
Cell structure and metabolism
When compared to other bacteria such as micrococcus, S. epidermidis’ cell wall is much stronger. The addition of lysostaphin can differentiate S. epidermidis from micrococcus. Micrococcus is more likely to lyse whereas the cell wall of S. epidermidis contains chemical properties of the peptidoglycan that prevent it from lysis. There are endopeptidases that cut the glycl-glycine bonds in the penta or hexpeptide crossbridge of the peptidoglycan of S. epidermidis. The strains that contain serine in the interpeptide bridges are more resistant to lysis (4).
The cell wall of Staphylococci contain teichoic acids which are connected to the peptidoglycan by covalent bonds. The teichoic acids are composed of either glycerol or ribitol which are connected by phosphodiester bonds. They are water soluble polymers made up of 30-50% of the dry components of the cell. S. aureus and S. epidermidis can be distinguished by having ribitol or glycerol. S. epidermidis has glycerol teichoic acid glucosyl residues while S. aureus has N-acetylglucosamine ribitol teichoic acid (4).
S. epidermidis is capable of growing using glucose anaerobically but cannot create coagulase or ferment mannitol. Most strains of S. epidermidis make acetoin, phosphatase and reduce nitrate. With oxygen, all strains can produce acid when exposed to glucose, fructose, maltose, sucrose, and glycerol and 70%-90% with galactose, mannose, and lactose. Acid cannot be formed from mannitol, trehalose, rhamnose, xylose, or arabinose (4).
Ecology
The natural environment of S. epidermidis is the human body and usually originates from disease. Since the bacteria usually lives on the skin and nares of all human beings and is a nosocomial pathogen, it is imporant to be able to identify the specific strains. S. epidermidis is the most common staphylococcus on the human skin. In addition, S. epidermidis also covers 90%-100% staphylococci from the nares when S. aureus is not present. When S. aureus is present the S. epidermidis amount decreases drastically (4). The formation of biofilm allows S. epidermidis to attach and grow on biomedical devices and be released into the blood to infect new areas (8).
Pathology
The increase use of intravascular catheters has caused a similar increase in S. epidermidis infections. The increase causes a problem since S. epidermidis is resistant to methicillin and all penicillins, penems, carbapanems, and cephalosporins which are commonly used antibiotics (3). S. epidermidis has also been found to be more resistant to antibiotics than other species (4).
Although there are no one specific viruelence factors of S. epidermidis, the ability to form biofilm is one of the virulence factors (5,6). The biofilm allows the bacteria cells to adhere to an inert or living areas (5). When a biofilm has formed it becomes harder to treat since the cells inside the biofilm are guarded from antibiotics and the immune system (5). Biofilm also releases a host immune response to antigens which prevents the removal of the biofilm and may also result in tissue damage (9). The bacteria can be released into the blood from biofilms and start new infections by attachment to the medical devices, thus devices will be required to be removed (8).
Some preventive strategies for infections are to provide prohylatic antibiotic therapy to cover surgical insertions from temporary intravascular devices. There are also reports that warn to not use antibiotic prohylaxis, especially vancomycin for dialysis. Aseptic techniques should be used for catheter infections to prevent contamination. New techniques concentrate on physical electrical barriers for colonization and using biomaterials with antimicrobial agents already inside. However these new methods have not been tried in the clinical settings(9).
Application to Biotechnology
S. epidermidis contains a lipase gene that can increase lipase activity and improve substrate specificity with the use of site-directed mutagenesis. Wild type and mutant genes (M415A and V6491) are capable of making different flavor esters in aqueous solution. Flavoring components are often made by esters. They are used in fruit-flavored products, baked goods, wines and dairy products. However, they have been removed from major food systems because they are expensive. By using natural raw materials such as fatty acids and alcohols, the flavoring esters can be made cheaper. The lipases of S. epidermidis are able to produce esters without the use of organic solvents which is an advantage. When organic solvents are not used, toxicity and flammability can be prevented. In addition to simplifying the purification of the product, it can also form different types of esters such as medium-chain esters, geranyl esters and unsaturated esters and can be engineered to form short-chain esters and other fatty acids (10).
Current Research
In Tunisia, there is an increase of infections of the methicillin-resistant strain Staphylococcos epidermidis. 32 S. epidermidis strains were isolated from samples of the dialysis water and needles removed from a dialysis center in Kairouan (Centre of Tunisia). An ATB staph kit was used to determine the antibiotic resistance of the strains for 18 different antibiotics. The results showed that most strains were penicillin resistant (93.8%), tetracyline (68.7%) and kanamycin (53.2%). PCR assay was also used to identify the genes icaA/icaD (intercellular adhesion), mecA (oxacillin resistance), ermA/ermB/ermC (erythromycin methylase resistance) and msrA and mef (macrolide efflux gene). The results showed 71.9% icaA/icaD, 78.1% mecA, 12.5% ermA, 31.3% ermB, 53.1% ermC, 68.8% msrA, and 0% mef. The susceptibility results from the ATB staph and the identified genes from the PCR did not match and shows that PCR is too fast in the investigation of staphylococci when compared to traditional methods. However, it can assist in understanding nosocomial infections by examining the transmission patterns and determining antibiotic susceptibilities (3).
Since biofilm is one of the known virulence of S. epidermis, it is often the subject of research. Biocides such as hydrogen peroxide, povidone-iodine solution, 60% (v/v) N-propanol and a commercial mix of propanol/ethanol/chlorhexidine were added onto bacterial biofilms removed from cardiac implant infections and bacteraemia of catheters. The biofilms and controls were incubated for different lengths of times in the different biocides. The biofilms observed from the patients were thicker than the biofilms from the healthy volunteers (controls). The results showed that none of the S. epidermidis treated with alcohols, N-propanol or the propanol/ethanol/chlorhexidine mix were living in the biofilms. The incubation in hydrogen peroxide within 5 minutes reduced the living cells to <5. The cells incubated in povidine-iodine was less effective because there were many living cells after 30 minutes of incubation. Hydrogen peroxide (3%,5%) is the most efficient way to remove S. epidermidis because it effectivly reduces the amount of biofilm and kills the cells. Hydrogen peroxide can be used on biofilms in the clinical setting, but it is toxic and can irritate the skin when used for a prolonged time. Therefore, it can only be used on surfaces and must be analyzed before applying on wounds and fistulas (5).
Coagulase-negative staphylococci that are resistant to multiple treatments such as Staphylococcus epidermidis may be the cause of infection during bone marrow transplants. Two new antibiotics, daptomycin and tigecycline are effective towards gram-positive bacteria and staphylococci that are resistant to methicillin. A current study compares the effectivness of daptomycin and tigecycline to vancomycin and fosfomycin towards coagulase-negative staphylococci from infected bone marrow transpant patients. The minimal inhibitory concentrations (MIC) from in vitro susceptibility testing were used in comparison to determine the effectiveness of the antibiotics. The results show that all the staphylococci were susceptible by the new antibiotics and vancomycin. Vancomycin is still used during bone marrow transplants (12).
References
11. http://www.tigr.org/tdb/staphylococcus/jbacteriol_4_2005.pdf Image of Reference #7
Edited by Angela Cheng, student of Rachel Larsen at UCSD
Edited by KLB
