Visceral Leishmaniasis (Kala azar)

Etiology/Bacteriology
Taxonomy
Description
Pathogenesis
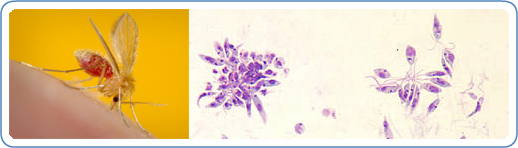
Transmission/Reservoirs
Visceral leishmaniasis is most commonly transmitted through the bite of an infected female phlebotomine sand fly. The infected stage of visceral leishmaniasis is called promastigotes. Less common forms of transmission include blood transfusions, contaminated needles, and from pregnant mother to her child. This does not form until two to eight months after the person has been bitten by an infected sand fly. Phelobotomine sandflies feed on the blood humans and animals, which allows them to develop their eggs. If a female phlebotomine sand fly bites an infected animal or human the next person who receives a bite from the sand-fly will be infected and develop into visceral leishmaniasis (http://www.doctorswithoutborders.org/our-work/medical-issues/kala-azar-leishmaniasis).
Infectious Dose
The infectious dose is unknown. (http://www.msdsonline.com/resources/msds-resources/free-safety-data-sheet-index/leishmania-spp.aspx). However, the number of parasites transmitted by an infected sand fly can influence the immune response. The higher the infectious dose the stronger the immune response which limits the spread of the parasite. This helps protect the patients visceral organs from infection. (SOURCE)
Incubation
The incubation period can be from two to six months. (SOURCE)
Colonization
After being bitten by an infected sand fly, the promastigotes are phagocytized by host macrophages. The parasite is now able to turn the macrophage into amastigotes. Amastigotes is the tissue stage. After the parasite is in the tissue stage, it can proliferate to infect other mononuclear phagocytic cells in different tissues. The main organs infected include spleen, liver, and bone marrow. If left untreated it is a life threatening disease. (http://www.cdc.gov/parasites/leishmaniasis/biology.html) .
Epidemiology
There are approximately 200,000 to 400.000 cases of visceral leishmaniasis every year. There are over 20,000 deaths annually. Over 90% of visceral leishmaniasis cases occur in the India, Bangladesh, Nepal, Sudan, South Sudan, Ethiopia and Brazil. Visceral leishmaniasis is not commonly found in the United States. If visceral leishmaniasis is found in the United States the person who contracted it traveled to other places where visceral leishmaniasis is common. The host range includes humans, wild rodents, and domesticated dogs. This disease in humans is reduced in areas where dog populations have been dramatically reduced. CDC
Virulence Factors
Clinical Features
Diagnosis
In order to diagnosis visceral leishmaniasis, a sample from bone marrow of the infected patient is necessary. The bone marrow then can be examined under a microscope or in special cultures. Another way visceral leishmaniasis can be detected is through a blood test. This type of test can detect antibodies that the host immune system makes to defend itself against the pathogen. A quick way to detect visceral leishmaniasis is by polymerase chain reaction (PCR). Other ways of detecting visceral leishmaniasis by coagulation studies, liver function test, and peripheral blood smears. (http://emedicine.medscape.com/article/220298-overview)
Treatment
Prevention
There is no vaccines available to prevent people from visceral leishmaniasis It is important for people to avoid outdoor activities, especially in the evening and night, because this is when sandflies are most active. When outdoors in areas where visceral leishmaniasis is endemic, one should minimize the amount of exposed skin. It is important to wear long-sleeved. In the evening, it is highly recommended to use a sleeping net to keep the sandflies out and other potentially harmful vectors. Insect repellent is another way to help prevent contracting visceral leishmaniasis. (CDC).
Host Immune Response
References
Created by Taylor Caswell Student of Dr. Tyrrell Conway, University of Oklahoma
