Chlamydia Pneumoniae

Etiology/Bacteriology
Taxonomy
| Order = Chlamydiales
| Family = Chlamydiaceae
| Genus = Chlamydia
| Species = Chlamydia pneumoniae
|NCBI: Taxonomy Genome: Genome|}
Description
Chlamydophila pneumonia (TWAR) is a recently recognized third species of the genus Chlamydia that causes acute respiratory disease. The strain name TWAR was derived from the first conjunctival isolates of the species (TW-183 and AR-39), although the pathogen initially colonizes the reparatory tract. [1]
Pathogenesis
Incubation and Colonization
The incubation period of C pneumoniae is approximately 3-4 weeks, with a usually gradual onset.[6] If upper respiratory tract symptoms (eg. rhinitis, laryngitis, pharyngitis, sinusitis) increase in severity to bronchitis or pneumonia, symptoms can present in an additional 1-4 weeks.[6] The symptoms are not always biphasic, however, and many hosts do not show symptoms beyond a mild initial respiratory infection. As C. pneumoniae is a respiratory pathogen, its initial sites of colonization are the oral and nasal mucosa. Once it colonizes the lungs, it is distributed by monocytes through blood circulation to other areas of the body.
Epidemiology
The estimated number of cases of pneumonia caused by C pneumoniae in the United States is 300,000 cases per year, and the pathogen is estimated to cause 10-20% of community-acquired pneumonia (CAP) cases among adults.[6] While all ages are at risk, C. Pneumoniae infection is most common in children between 5 and 14 years old. In the United States, about 50% of adults have evidence of past infection by age 20, and reinfection throughout life is common.[7] C. pneumoniae appears to have a worldwide distribution, although the prevalence of infection varies by region.[7] Studies of adults from 10 areas of the world have shown a higher population prevalence in tropical, less developed countries.[7]
Most of the fatalities associated with C. pneumoniae infection have been in persons with underlying illness and complications [7]. C. pneumonia has been known to contribute to serious morbidity and mortality among populations with weakened immune responses such as residents of nursing homes who suffer respiratory disease outbreaks.[17]
Transmission
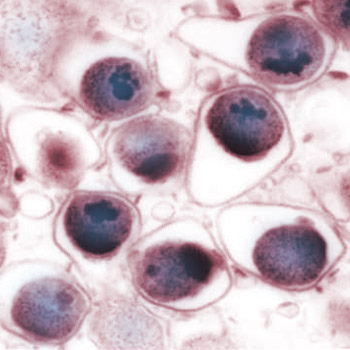
C. pneumoniae exists in one of two states. Its infectious, non-replicating state, known as the elementary body (EB) is stationary and extracellular. In this stage, C. pneumoniae has the ability to withstand environmental stresses until it is transferred to a new host’s lungs through small droplets. Once in the lungs, the EB is taken up into an endosome by phagocytosis. However, the EB is not destroyed by fusion of the endosome with a lysosome, as is typical for phagocytosed pathogens. Instead, it transforms into a larger intracellular form, or reticulate body (RB), that begins to replicate within the endosome. [7] After multiple rounds of division, the RBs are re-differentiated into an infectious EBs that are released into the cytoplasm to initiate new cycles in new host cells. [16] C. pneumoniae also tends to infect endothelial cells, the cells that line blood vessels[4] . The ensuing inflammation results in the creation of new blood cells that draw in the pathogen, providing additional hosts for the bacterial parasite that allow it to further spread through the body. If Chlamydia is residing in peripheral blood cells and inflammation occurs in the host’s body, the inflammatory process can become secondarily infected by Chlamydia, no matter what the source of the inflammation. [4] Vascular infection further infects bone marrow cells, which then produce infected and dysfunctional immune cells (macrophages, neutrophils, etc.). [18]
Clinical Presentation
Symptoms
Because the initial site of colonization is the lungs and ciliated cells of the airways, pneumonia and bronchitis are the most common clinical manifestations of infection by C. pneumonia. Additional symptoms include gradual onset of cough with low-grade fever. Less common presentations are pharyngitis, laryngitis, and sinusitis. [3] Respiratory manifestations can be biphasic, with resolution of pharyngitis prior to development of a more typical bronchitis or pneumonia syndrome [7]. A cough can persist for weeks to months despite appropriate use of antibiotics. [6]
Associated Diseases
The ability of C. pneumoniae to spread to various tissues after respiratory infection and infect various cell types is fundamental for its pathogenesis, and results in diverse possibilities for manifestation of infection.[16] The locus of the Cpn infection determines which disease will result and manifest symptomatically. Although some studies clearly associate C pneumoniae organisms with diseases such as Coronary Artery Disease, multiple sclerosis[14], asthma[15], Alzheimer’s disease[9], and Atherosclerosis [11], the role of C pneumoniae in the pathogenesis of these diseases requires further definition [6]. We will only examine the current research in C.pnemoniae-associated Alzheimer’s Disease and Atherosclerosis here.
Alzheimer's Disease
Alzheimer’s Disease (AD), considered the most significant single cause of senile dementia, is a progressive neurodegenerative disease associated with atrophy and death of neurons in affected brain regions [9]. The disease occurs in two forms: an early-onset form which is primarily genetically determined, and a far more common late-onset form which is not genetically determined [9]. Studies of brain tissue samples from late-onset AD patients has shown that C. pneumoniae DNA is widely present, while absent in non-Alzheimer’s control samples. [10] Essentially, the only risk factor generally accepted as valid for influencing the development of late-onset disease is possession of the ɛ4 allele type[10] Not all patients expressing the ɛ4 allele develop AD, but its presence increases risk for the disease. Experimental data has shown a relationship between possession of the ɛ4 allele and the pathobiology of Cpn [10] . Many AD studies indicate that treatment of AD patients with anti-inflammatory drugs is beneficial, [10] suggesting that the inflammation characterizing the AD brain is an important component of AD neuropathogenesis. Because all species of Chlamydia are known to cause inflammation at their sites of infection, these studies suggest that at least some portion of the AD-related inflammation can be attributed to chlamydial infection. [9]
Atherosclerosis
Atherosclerosis is a disease characterized by plaque build-up in arteries, which limits oxygen flow and can lead to complications such as heart attack, chronic kidney disease and stroke.[11] Death due to coronary atherosclerosis accounted for approximately 50% of all cardiac deaths in 2014, and 50% of coronary atherosclerosis deaths are sudden and unexpected. [12] As with other multifactorial, chronic diseases, the factors that cause atherosclerosis are complicated. The association between C. pneumoniae and atherosclerosis is difficult to prove and therefore a subject of debate. However evidence for the presence of Cpn in atherosclerotic lesions has emerged from nearly 40 distinct conducted around the world.[10] While the strength of association is debated, C. pneumoniae’s capactity to initiate and propogate inflammation can no doubt exacerbate symptoms of atherosclerosis. In addition, studies have shown that patients with cardiovascular disease have higher titres of anti-C. pneumoniae antibodies compared with control patients.[10] Further studies in vitro have shown that C. pneumoniae infection induces foam cell formation, a key event in early atheroma development. [13]
Diagnosis
Diagnosis of acute infections is reasonably well established in most laboratories, but chronic infections pose a different problem as the manifestation of infection is often caused by a multitude of factors. Diagnosis is typically based on direct microscopy and serology[19] . The majority of C. pneumoniae infections are asymptomatic or mild upper respiratory tract infections, most of which are mild and self-restricted and therefore often go undiagnosed.[16] Atypical pneumonia, bronchitis and sinusitis are the most frequent respiratory diseases caused by C. pneumonia, and persistent respiratory infections such as these can serve as an indicator for possible Chlamydia infection.[1]
Treatment
Macrolides are often the first-line treatment, while tetracyclines and fluoroquinolones are also effective. [3] C. pneumoniae is not susceptible in vitro to penicillin, ampicillin, or sulfa drugs [7]. Clinical experience shows that symptoms of C. pneumoniae infection frequently recur after short courses of antibiotics, and persistent infection has been documented by culture after treatment [7]. Therefore, intensive long-term treatment is recommended.
Damage Response Framework
The damage response framework is a recently proposed pathogen classification system that measures the interaction between the pathogen and the host and classifies the pathogen by the amount of damage done to the host.[8] By acknowledging both sides of the host-pathogen interaction, this theory is able to give an explanation as to why the same pathogen can cause different levels of damage depending on the host. According to the damage response framework, interaction between the two parties can result in damage to the host, benefit to the host, or can have no effect. These levels of damage can then lead to circumstances of symbiosis, colonization, commensalism, latency, and disease. [8].
Chlamydia species fall under the class of pathogens that cause damage across the spectrum of immune responses, but damage it causes can be enhanced by strong immune responses from the host (known as Class 5 in the damage-response framework.) [16] The pathogen has been shown to infect and proliferate in endothelial cells, smooth muscle cells and macrophages, aggravating existing inflammation and causing damage to the host in every instance of host response. Several in vitro experiments have shown that C. pneumonia infection induces the expression of pro-inflammatory cytokines such as TNF-α, IL-1βand IL-6 in vascular cells[16], which also contributes to existing inflammation and further exacerbates damage to the host.
References
1. Grayston, J. T., C.-C. Kuo, L. A. Campbell, and S.-P. Wang. 1989. Chlamydia pneumoniae sp. nov. for Chlamydia sp. strain TWAR. Int. J. Syst. Bacteriol. 39:88–90.
2. Kuo, C., & Grayston, J. (n.d.). Chlaymydia spp. strain TWAR A newly recognized organism associated with atypical pneumonia and other respiratory infections. Clinical Microbiology Newsletter, 137-140.
3. "Chlamydophila Pneumoniae Infection." Centers for Disease Control and Prevention. Centers for Disease Control and Prevention, 7 Feb. 2014. Available at: http://www.cdc.gov/pneumonia/atypical/chlamydophila.html
4. Humphrey, Nancy. "Chlamydia Pneumoniae Not Caught like You Thought (04/23/99)." Reporter: Vanderbilt University Medical Center. Available at: http://www.mc.vanderbilt.edu:8080/reporter/index.html?ID=779.
5. Oba, Yuji. "Chlamydial Pneumonias." : Overview, Pathophysiology, Epidemiology. 2 Nov. 2013. Available at: http://emedicine.medscape.com/article/297351-overview#a1.
6. Kuo CC, Jackson LA, Campbell LA, Grayston JT. Chlamydia pneumoniae (TWAR). Clinical Microbiology Reviews. 1995;8(4):451-461.
7. Casadevall A, Pirofski L. 2003. The Damage Response Framework of Microbial Pathogenesis. Nat Rev 1:17-24.
8. Hudson, MAP. What is the evidence for a relationship between Chlamydia pneumoniae and late-onset Alzheimer's disease? Laboratory Medicine. 2001:680–685.
9. Gérard, H. C., Dreses-Werringloer, U., Wildt, K. S., Deka, S., Oszust, C., Balin, B. J., Frey, W. H., Bordayo, E. Z., Whittum-Hudson, J. A. and Hudson, A. P. (2006), Chlamydophila (Chlamydia) pneumoniae in the Alzheimer's brain. FEMS Immunology & Medical Microbiology, 48: 355–366. doi: 10.1111/j.1574-695X.2006.00154.x
10. Mahony JB, Coombes BK. Chlamydia pneumoniae and atherosclerosis: does the evidence support a causal or contributory role? FEMS Microbiol Lett. 2001;197:1-9.
11. Farb A, Tang AL, Burke AP, Sessums L, Liang Y, et al. Sudden coronary death. Frequency of active coronary lesions, inactive coronary lesions, and myocardial infarction. Circulation. 1995;92:1701–1709.
12. Kalayoglu, M. V., & Byrne, G. I. (1998). A Chlamydia pneumoniae Component That Induces Macrophage Foam Cell Formation Is Chlamydial Lipopolysaccharide. Infection and Immunity, 66(11), 5067–5072.
13. Layh-Schmitt G, Bendl C, Hildt U, Dong-Si T, Juttler E, Schnitzler P, Grond-Ginsbach C, Grau AJ: Evidence for infectionwithChlamydiapneumoniaeina subgroupofpatientswithmultiplesclerosis.AnnNeurol47,652-655 (2000).
14. Hahn DL, Schure A, Patel K et al. (2012). "Chlamydia pneumoniae-specific IgE is prevalent in asthma and is associated with disease severity". PLoS ONE 7 (4): e35945. doi:10.1371/journal.pone.0035945. PMC 3335830. PMID 22545149.
15. Bailey, Leslie. "Infection Biology of Chlamydia Pneumoniae." Department of Molecular Biology: Laboratory for Molecular Infection Medicine Sweden (MIMS), 2008. <http://www.diva-portal.org/smash/record.jsf?pid=2:141442>.
16. Troy CJ, Peeling RW, Ellis AG, et al. Chlamydia pneumoniae as a New Source of Infectious Outbreaks in Nursing Homes. JAMA. 1997;277(15):1214-1218. doi:10.1001/jama.1997.03540390044033.
17. Mussa FF, Hong Chai H, Wang X et al. Chlamydia pneumoniae and vascular disease: an update. J Vasc Surg 2006; 43: 1301–1307.
18. Saikku, P. (1998). Diagnosis of Chlamydia pneumoniae. Clinical Microbiology and Infection, 4(4), 4S7–4S13-4S7–4S13. doi:doi:10.1111/j.1469-0691.1998.tb00698.x
Created by Erika Cummings, a student of Tyrrell Conway at the University of Oklahoma.
